The most common upper respiratory tract infections are infections of the lining of the nose (ie, rhinitis or “runny nose”), throat infections (pharyngitis), and infections of the voice box or larynx (laryngitis).
The first place where pathogenic microorganisms (usually viruses, and sometimes bacteria) settle is the nasopharynx area. The symptoms are almost always the same: sore throat, runny nose and cough. Rhinopharyngitis is the most common reason for consultation with general practitioners. This pathology is nothing more than a cold, which is an inflammation of the nasopharynx in adults and children and is mainly viral in nature. It is essentially an infectious disease that causes inflammation in the upper part of the throat and usually goes away on its own after 7 or 10 days. But what is it - nasopharyngitis?
General description of nasopharyngitis
Rhinopharyngitis (nasopharyngitis) - inflammation of the mucous membrane of the nasopharynx. It is a mild illness, most common in children aged six months to four years, but can also affect adults.
Rhinopharyngitis can be caused by more than 200 types of viruses, the most common are:
- rhinoviruses, which make up 30-80%;
- influenza viruses - 10-15%;
- adenovirus - 10-15%.
Nasopharyngitis caused by a rhinovirus is most contagious during the first three days after symptoms appear.
Most of these viruses are predominant in winter, but you can get nasopharyngitis at any time of the year.
And even if this is not a serious disease, it still needs to be treated correctly in order to get rid of it as soon as possible.
Rhinopharyngitis is mainly of viral origin, but can recur up to several times a year; in this case, it is necessary to look for an allergic cause: mites, pollen or animal dander.
Types of nasopharyngitis:
- catarrhal;
- atrophic;
- purulent;
- chronic;
- allergic;
- subatrophic rhinopharyngitis;
- rhinonasopharyngitis.
Factors that contribute to the development of nasopharyngitis include dry and damaged mucous membranes during cold periods, a suppressed immune system, stress, fatigue and an overall unhealthy lifestyle.
Complex treatment of patients with exacerbation of chronic hypertrophic pharyngitis
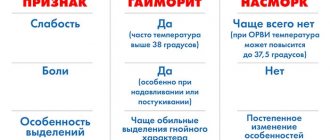
Local sore throat is the main, and sometimes the only symptom in a number of acute and chronic diseases of the pharynx. The accompanying intoxication syndrome in patients with exacerbation of chronic diseases of the pharynx and the associated increase in body temperature, weakness and fatigue may not be expressed. On the contrary, pain—intense, long-lasting, causing difficulty in swallowing and often resistant to self-treatment—is the main reason why patients seek medical attention.
Therapy for pain syndrome during exacerbations of chronic inflammatory processes in the pharynx traditionally comes down to a combination of local procedures: warm alkaline rinses, inhalations, astringents, menthol, etc., with antiseptic or antibacterial drugs. In addition, some pharmaceutical manufacturers include local anesthetic drugs, such as xylocaine, in antiseptic agents.
The prescription of drugs with systemic analgesic, anti-inflammatory and antipyretic effects (non-steroidal anti-inflammatory drugs (NSAIDs)) for chronic diseases of the pharynx is not widespread due to low efficiency and the impossibility of long-term treatment.
More promising seems to be the use of the unique composition of the drug strepfen (flurbiprofen), produced by the pharmaceutical company Boots Healthcare International (UK).
Flurbiprofen belongs to the group of non-selective NSAIDs: by inhibiting the enzymes cyclooxygenase type 1 and cyclooxygenase type 2, it leads to inhibition of the synthesis of prostaglandins - mediators of pain and inflammation. The analgesic and anti-inflammatory effect of flurbiprofen develops much faster compared to the effects of selective NSAIDs (type 2 cyclooxygenase inhibitors). This property of the drug has found application in ophthalmology and rheumatology, where flurbiprofen is prescribed in external forms.
One strepfen tablet contains 8.75 mg of flurbiprofen, which is quite enough to develop a persistent (up to 3 hours) anti-inflammatory and analgesic effect within 15–30 minutes. This dosage of the drug is sufficient to develop a pronounced local effect. At the same time, it is insignificant for the development of a systemic effect and associated undesirable side effects characteristic of drugs from the NSAID group. Despite the high absorption and affinity of flurbiprofen for plasma proteins (99%), systemic side effects can only be observed when the recommended daily dose is exceeded by 3–6 times.
Our study involved 40 patients with exacerbation of chronic hypertrophic pharyngitis: 28 women and 12 men aged 16 to 68 years. The duration of exacerbation of chronic hypertrophic pharyngitis ranged from 5 days to 3 weeks.
All patients complained of sore throat of varying intensity. In 23 people, the pain was constant and was accompanied by a feeling of “swelling of the mucous membranes” or a feeling of a “foreign body” in the throat. In 27 patients, pain increased with swallowing. In the majority of patients, treatment was preceded by self-initiated treatment (gargling, local antiseptics, antibacterial therapy), which had an insignificant and short-term effect. Almost half of the patients (19 people) had a history of bilateral tonsillectomy.
The localization of the hypertrophic process in the pharynx was distributed as follows: hypertrophy of the lateral columns of the pharynx - 17 people, hypertrophy of the islands of lymphoid tissue on the posterior wall of the pharynx (granular pharyngitis) - 9 people, palatal niches (in patients with a history of tonsillectomy) - 2 people, mixed localization - 12 people. In 19 patients, local inflammation of the lymphoid tissue was combined with severe catarrhal inflammation of the oropharyngeal mucosa.
The exclusion criteria from the study were: erosive and ulcerative lesions of the gastrointestinal tract in the acute phase; bronchial asthma, urticaria and rhinitis caused by taking NSAIDs; severe dysfunction of the liver and kidneys; pregnancy and lactation; as well as a history of hypersensitivity to flurbiprofen or components of the drug.
The patients were divided into two groups. All patients underwent double cauterization of lymphoid granules of the oropharynx with a 10% solution of silver nitrate (lapis) with an interval of one day (the first and third days of treatment). Half of the patients (20 people)—the main study group—were prescribed strepfen at a dosage of 8.75 mg (1 tablet) 5 times a day (with an interval of 3 hours). Patients were advised to dissolve the tablet in the mouth until it is completely dissolved. Treatment began 5–6 hours before the first cauterization procedure with a solution of silver nitrate. The course of treatment was 3 days.
Patients assessed the severity of pain in the throat using a visual analogue scale (VAS) from 0 to 10 points. In this case, the absence of a sign was taken as 0, and its maximum severity was taken as 10. At the end of treatment, patients characterized the general dynamics of symptoms (pain in the throat, sore throat, dryness, feeling of a foreign body in the throat) (VAS 0–10 points), as well as drug tolerance (good, satisfactory, unsatisfactory). The doctor assessed hyperemia and the degree of infiltration of granules of lymphoid tissue of the oropharynx (0–5 points).
All patients receiving strepfen already 10 minutes after the first dose of the drug showed a decrease in sore throat, in most cases significant, up to complete relief of the pain syndrome (in 5 patients). The day after the cauterization procedure (second day of treatment), patients in both groups noted a decrease in sore throat, which was more significant in the group of patients receiving strepfen (almost 2 times). On the third day of treatment, before the second cauterization of granules of lymphoid tissue of the oropharynx, the severity of pain was also assessed. Patients of the first group receiving strepfen noted a further significant reduction in sore throat compared to the previous day (by almost 50%). In the second group of patients who did not receive strepfen, slight positive dynamics also remained, although two patients noted a slight increase in pain compared to the previous day. The day after the second cauterization procedure (4th day of observation), patients in both groups noted a decrease in sore throat compared to the previous day, and more pronounced positive dynamics were observed in the second group of patients - in the first group of patients on the 4th day of treatment there was strepfen was canceled (Table 1, Fig. 1).
| Table 1. Dynamics of the intensity of sore throat during treatment with strepfen (group I) and without the use of the drug (group II) (VAS 0–10 points) |
| Figure 1. Dynamics of the intensity of sore throat during treatment with strepphen (group I) and without the use of the drug (group II) VAS 0–10 points) |
A visual examination of the oropharynx of patients in both groups revealed a decrease in the degree of infiltration of lymphoid tissue that was cauterized with silver nitrate. The positive dynamics of this indicator was slightly higher in the group of patients receiving strepfen (Table 2, Fig. 2). The intensity of hyperemia of granules of lymphoid tissue of the oropharynx, as the main indicator of the severity of inflammation, significantly decreased during treatment in patients receiving strepfen (by 80%) (Table 3, Fig. 3).
| Table 2. Dynamics of the degree of infiltration of granules of lymphoid tissue of the pharynx during treatment with strepfen (group I) and without the use of the drug (group II) (VAS 0–5 points) |
| Figure 2. The severity of lymphoid tissue infiltration after cauterization during treatment with strepphen (group I) and without the use of the drug (group II) (VAS 0–5 points) |
Considering the above data, we can confidently say that the use of flurbiprofen in combination with chemical cauterization with a 10% silver nitrate solution in the treatment of exacerbations of chronic hypertrophic pharyngitis provides a significantly more pronounced regression of inflammatory symptoms and provides a high analgesic effect.
| Table 3. Dynamics of the severity of hyperemia of granules of lymphoid tissue of the pharynx during treatment with strepfen (group I) and without the use of the drug (group II) (VAS 0–5 points) |
| Figure 3. The severity of hyperemia of lymphoid tissue granules during treatment with strepfen (group I) and without the use of the drug (group II) (VAS 0–5 points) |
Analysis of the treatment results showed that the use of local anti-inflammatory therapy with flurbiprofen significantly increases the effectiveness of chemical cauterization of inflamed hypertrophied areas of the lymphoid tissue of the oropharynx. Complete remission after 3 days of treatment was achieved almost 2 times more often compared to the control group (Table 4).
The tolerability of the drug strepfen was assessed as good in most cases. One patient (5%) experienced a metallic taste in the mouth on the second day of treatment, which was not a reason to discontinue the drug.
| Table 4. Outcome of the disease after a course of treatment with strepfen (group I) and without the use of the drug (group II) |
From the above, the following conclusions can be drawn.
- The use of the drug strepfen in combination with chemical cauterization with a 10% silver nitrate solution provides a high analgesic effect and a significantly more pronounced regression of inflammatory symptoms compared to cauterization monotherapy in the treatment of patients with exacerbation of chronic hypertrophic pharyngitis.
- The use of local anti-inflammatory therapy with the drug strepfen significantly increases the effectiveness of chemical cauterization of inflamed hypertrophied areas of lymphoid tissue of the posterior pharyngeal wall. Complete remission after 3 days of treatment was achieved almost 2 times more often than in the comparison group.
- Strepfen in a therapeutic dose and subject to the terms recommended by the manufacturer for self-administration is well tolerated by patients. In the present study, there were no cases of systemic effect, as well as serious side effects and complications when taking the drug locally.
A. V. Bozhko , Candidate of Medical Sciences City Clinic No. 124, Moscow
Symptoms and first signs
The incubation period is quite short, amounting to 16 hours after infection enters the body.
Initial symptoms are mild fatigue, a feeling of cold, sneezing and a slight headache, they soon develop into nasopharyngitis with a stuffy nose, nasal discharge, sore throat and low-grade fever, peaking at 2-4 days.
During the incubation period, the first symptoms of nasopharyngitis appear, namely:
- unusual and unexplained fatigue occurs;
- fever appears, rarely exceeding 38.5 degrees;
- runny nose, first clear, then thick (yellowish to greenish);
- nasal congestion, which may be accompanied by shortness of breath;
- mild sore throat and redness;
- fairly dry cough;
- sneezing;
- ear pain;
- tearfulness;
- the body “aches”;
- headache and/or abdominal pain;
- loss of appetite.
Fever lasts two or three days in the case of nasopharyngitis. To reduce your fever, you can take paracetamol at recommended doses at least 6 hours apart.
Reasons for the development of the disease
According to the etiology of occurrence, the disease is divided into several types: chronic or acute, infectious or non-infectious (most often allergic). Accordingly, there are a number of reasons that can lead to the development of the disease. The main list includes:
- infection with various infections. In most cases, we are talking about viral infections (rhinoviruses, coronaviruses, adenoviruses, ECHO virus, influenza viruses, etc.). And only 20–30% are due to other infections - bacterial and fungal;
- the occurrence of allergic reactions to pollen, animal hair, mites, taking any medications, etc.;
- untreated rhinitis, against the background of which similar complications developed;
- neuroendocrine and autoimmune disorders, mechanical and chemical effects - such etymology is extremely rare, but also possible.
In practice, rhinopharyngitis most often occurs of a mixed nature (for example, polymicrobial or infectious-allergic).
In addition to the direct etymology, there is a set of factors that contribute to infection. These are weakened immunity, frequent hypothermia, stressful situations, the presence of chronic diseases of the respiratory system, anatomical features that make breathing difficult (deviated nasal septum, enlarged adenoids, etc.).
The transition of the disease to a chronic form can be caused by incorrect or untimely treatment, therefore, even with a mild form, it is important not to treat yourself, but to consult a specialist.
Diagnostics
When exactly should you go to the doctor?
- if the child is less than three months old;
- if the fever lasts more than 72 hours and does not decrease;
- if there is pain in the ear;
- if there are spots on the skin;
- if there is bleeding from the nose or urine with blood elements;
- if the child has breathing problems.
The diagnosis of nasopharyngitis is clinical, that is, it is established by examination and observation of symptoms. Does not require additional examination. A thorough clinical examination will eliminate the complication or associated pathology, such as otitis media, and evaluate possible risk factors.
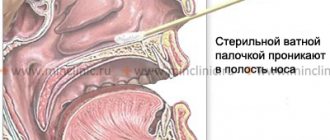
If you see an otolaryngologist (ENT), he or she may perform a rhinoscopy to examine the inside of the nose using a rhinoscope, a rigid or flexible optical device. In the case of nasopharyngitis, rhinoscopy shows a very red and congested mucous membrane of the nose and throat.
Symptoms of chronic rhinitis
Chronic rhinitis is accompanied by prolonged difficulty in nasal breathing. There is also a deterioration in the sense of smell, nasal discharge, the formation of mucus flowing down the back wall of the throat, and cough.
Vasomotor rhinitis is accompanied by episodes of sneezing with the release of copious liquid discharge and difficulty breathing through the nose.
With allergic rhinitis, itching and burning in the nose and eyes, severe runny nose, swelling, and sneezing appear.
In severe cases, the nasal mucosa becomes crusty and there is an unpleasant odor when breathing. Atrophic rhinitis is accompanied by dryness in the nasal cavity and pharynx, and nosebleeds.
Often, a patient with chronic rhinitis becomes dependent on decongestants - nasal drops and sprays that temporarily restore normal nasal breathing.
How to treat nasopharyngitis
Rhinopharyngitis usually goes away on its own. Treatment is aimed at limiting cold symptoms while keeping the patient comfortable and avoiding overexertion if necessary.
The following measures are prescribed:
- regular rinsing of the nasal sinuses (with saline, nasal spray, thermal or sea water);
- taking painkillers for pain and antipyretics for fever.
In the first days, a cough due to nasopharyngitis is often dry and painful, then people often wonder how to treat it. In this case, you can, on the doctor's recommendation, buy cough syrup. But be careful: as soon as the cough becomes wet and accompanied by mucus, syrups should be avoided. Because a wet cough helps evacuate germs. Cough is an excellent natural treatment for nasopharyngitis.
Also, keep in mind that a fever is just an expression of the body fighting an infection. In fact, viral infections of this type are often “self-limiting,” meaning that they will heal on their own. However, it is important to monitor your temperature and make sure it is not too high to prevent febrile seizures.
Contrary to what many parents believe, antibiotics do not help fight viral infections. Thus, treatment of nasopharyngitis consists of controlling symptoms. In some cases, antihistamines may be used to relieve allergies, antitussives to relieve coughing, or expectorants to help clear secretions. Antipyretics also help control fever.
Rhinopharyngitis usually lasts about 7-10 days. During this period, it is important to give the body sufficient rest. The healing process can be supported by keeping the mucous membrane moist, drinking enough fluids, or using inhalations and decongestants.
Treatment of chronic rhinitis in adults
Medical intervention is aimed at restoring nasal breathing. This significantly improves the quality of life of patients, although it may be impossible to completely get rid of chronic rhinitis.
Treatment at home
A person suffering from chronic rhinitis can lead a normal life and play sports. Often, regular physical activity leads to normalization of the functioning of vasoregulatory nerve centers, and the manifestations of vasomotor rhinitis recede.
If the inflammation of the nasal mucosa is of an allergic nature, elimination (removal) of the allergen from the external environment is necessary (fighting dust, avoiding contact with pollen or pets, and so on).
For chronic rhinitis, humidifying the air in the room is useful. The patient is advised to avoid spicy and hot foods, as well as sweets. Breathing exercises are shown.
Folk remedies against chronic rhinitis
For chronic rhinitis, the following alternative treatment methods may be useful:
- drinking decoctions of black and red currant branches, marshmallow and eucalyptus leaves;
- rinsing the nose with infusion of calendula mixed with chamomile flowers;
- compresses on the nasal area with grated raw onion;
- ingesting a mixture of grated lemon and honey;
- in the absence of allergies - instillation of eucalyptus, peach, rose, sea buckthorn, olive oils into the nostrils.
These simple remedies cannot rid the patient of the disease, but can enhance the effect of drug treatment for chronic rhinitis.
Drug therapy
Treatment of chronic rhinitis in adults and children depends on its form. For catarrhal cases, the following drugs are prescribed:
- antibacterial drops (Isofra) and ointments (Bactroban, 2% sulfanilamide ointment), antiseptics (2% salicylic ointment);
- silver preparations with an astringent effect (Protargol).
In the hypertrophic variant, sclerotherapy is prescribed. It includes the injection into the inferior nasal concha of the anti-inflammatory drug hydrocortisone (1 ml every 4 days, 10 injections in total) and the splenin biostimulator 0.5 - 1 ml every other day. Cauterization of thickened areas of the mucous membrane with chemicals is also used - silver nitrate, trichloroacetic, chromic acids. If such treatment is ineffective, surgery is performed.
For atrophic rhinitis, treatment is aimed at eliminating the symptoms:
- daily rinsing of the nose with saline solution with the addition of iodine, products based on sea water (Aqua Maris, Nazol Aqua, Sialor-Aqua, Aqua-rinosol and others);
- irrigation treatment - irrigation of the nasal cavity under pressure with mineral water, sodium chloride solution;
- irritants – 0.5% iodine-glycerol solution for application to the nasal mucosa.
For vasomotor rhinitis, the doctor may prescribe the following medications:
- antihistamines for oral administration (fexofenadine, desloratadine and others);
- antihistamines for topical use (Allergodil, Reactin, Tizin Alergy sprays);
- procaine in the form of endonasal blockades;
- glucocorticoid drugs for injection into the thickness of the mucous membrane.
Physiotherapy for the treatment of rhinitis
Treatment of chronic rhinitis in adults is complemented by physiotherapeutic techniques:
- endonasal UHF currents, microwave exposure, ultraviolet irradiation, helium-neon laser;
- endonasal electrophoresis of zinc sulfate, calcium chloride;
- insufflation (infusion) of fusafungin, rhinofluimucil, garlic juice, celandine, St. John's wort infusion, diluted solution of octenisept).
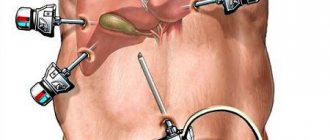
Surgical treatment of chronic rhinitis
Surgery is offered to patients with vasomotor or hypertrophic rhinitis that is not amenable to other types of therapy.
For vasomotor rhinitis, gentle techniques are used to reduce the volume of the mucous membrane in the area of the inferior turbinate: submucosal vasotomy, ultrasonic disintegration, submucosal laser destruction. If they are ineffective, a gentle conchotomy is performed - physical removal of part of the lower concha.
For hypertrophic rhinitis, vasotomy, submucosal disintegration by ultrasound, and gentle lower conchotomy are also used. Endoscopic osteoconchotomy and lateroconchopexy are also performed.
The choice of operation depends on the characteristics of the patient, the experience of the surgeon, and the available equipment. In modern clinics, such interventions are performed quickly, cause virtually no discomfort and are not accompanied by complications.
Complications of nasopharyngitis
The risk of complications increases without treatment or when the body cannot heal itself. On the one hand, viruses in the respiratory tract will multiply, infecting areas that are still healthy, and on the other hand, nasopharyngitis can pave the way for bacterial superinfections. Superinfection is when a viral infection sets the stage for a subsequent bacterial infection due to a weakened immune system. If your general health does not improve or your symptoms worsen, you should see your doctor as soon as possible.
Rhinopharyngitis rarely causes complications, but some people with weakened immune systems may experience a secondary bacterial infection in the form of:
- tonsillitis (inflammation of the tonsils of viral or bacterial origin);
- laryngopharyngitis;
- tracheitis (inflammation of the trachea, causing an irritating cough);
- bronchitis (inflammation of the bronchi, which usually manifests itself in the form of cough and difficulty breathing);
- sinusitis (inflammation of the sinuses associated with an infection of viral or bacterial origin);
- otitis (inflammation or infection of the ear);
In this case, consultation is necessary, as well as treatment with antibiotics if a bacterial infection is proven.
In children under 3 months of age, complications occur more often due to insufficient maturation of the immune system. Therefore, in this case, as in pregnant women, with constant fever, careful monitoring of the condition is necessary.
Diagnosis of chronic rhinitis
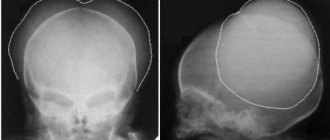
To recognize chronic rhinitis, basic and additional research methods are used. The main ones include collecting complaints, medical histories, as well as rhinoscopy, blood tests and radiography of the paranasal sinuses. Characteristic signs of chronic rhinitis identified during such studies:
- anterior rhinoscopy: thickening and redness of the surface of the nasal turbinates is determined, pathological discharge or crusts are visible, the mucous membrane may be pale, cyanotic, swollen; sometimes polyps or thinning of the bone structures of the nose are detected;
- blood test: with allergic rhinitis, an increased level of eosinophils is often found; with a long course of the disease, anemia cannot be ruled out; the cause of nosebleeds may be a pathology of platelets or blood clotting, which is also determined by this analysis;
- X-ray of the nasal sinuses: a narrowing of the nasal passage, thickening of the inferior turbinate, signs of ethmoiditis are determined, and symptoms of damage to the paranasal sinuses are often added.
If necessary, the ENT doctor will refer the patient for additional examinations, which may be necessary for differential diagnosis and proper selection of therapy:
- video endoscopic examination of the nasal cavity, allowing for a detailed examination of pathological areas of the mucous membrane;
- rhinopneumometry, during which air is supplied and pumped out into the nasal cavity, and the amount of pressure that can overcome difficult nasal breathing is determined;
- cytological examination of smears from the surface of the mucosa to study the cellular composition;
- bacteriological analysis of discharge and determination of the sensitivity of detected microorganisms to antibacterial drugs;
- Computed tomography provides a detailed image of the structures of the nose and surrounding tissues and is necessary when a tumor is suspected, a deformation of the nasal septum, and in other cases that are difficult to diagnose.
If necessary, the patient is referred for additional consultation with an allergist, pulmonologist, neurologist and other specialists.
An ENT doctor must differentiate chronic rhinitis from acute, as well as from specific forms of the disease (tuberculous and syphilitic), Wegener's granulomatosis and scleroma. Diseases of the paranasal sinuses are also excluded, since their joint damage is often noted - rhinosinusitis.
Traditional treatment
Treatment with folk remedies will help improve your condition and maintain your health.
- Using a humidifier. To thin out secretions, it is recommended to humidify the surrounding air and maintain the room temperature to 19 degrees.
- Inhalation of eucalyptus essential oils.
It is necessary to do inhalations so that it has a decongestant effect, helping to clear a stuffy nose. Essential oils can also be used in chest massage. But remember that treating colds with essential oils is contraindicated for children, pregnant or lactating women, patients with asthma or epilepsy. Consult your doctor before use. - Elder. Has antipyretic and anti-edematous effects. This plant can be used as an herbal tea (let steep for at least 10 minutes) or as a gargle (with cooled herbal tea) several times a day.
- Chamomile. For children, a runny nose can be very uncomfortable because it prevents them from breathing, causing them to be irritable and may lose their appetite. In these cases, it is best to resort to homemade solutions prepared with the addition of salt or chamomile.
Rhinopharyngitis can be treated well with folk remedies if you follow the above steps and know how to treat it.
How is diagnosis carried out?
The first rule of any disease is not to self-medicate, but to consult a doctor. For nasopharyngitis, as a rule, a visit to a therapist is sufficient. He listens to the patient, conducts a clinical examination and immediately makes a diagnosis. When the disease occurs, a fairly clear picture of the mucous membranes appears, which allows for an accurate diagnosis without additional examinations.
If the disease is advanced, there are risks of complications, chronic diseases and similar reasons, the therapist will refer you to an ENT specialist for a comprehensive diagnosis, prescribing specialized treatment and physiotherapeutic procedures.
Bacteriological studies are most often not carried out due to the sufficiency of clinical examination and symptoms, but can be prescribed if the etymology of the disease and the identification of its causative agent plays a decisive role in the choice of therapy.
Prevention
There are several rules to strengthen your immune system and prevent disease.
- Wash your hands often and teach your children to do it correctly, especially after blowing their nose.
- Do not share personal items such as glasses, dishes, or a sick person's towel.
- Protect your mouth when you cough or sneeze with a disposable tissue. If you don’t have a disposable tissue, cough into the crease of your elbow rather than into your palm.
- Don't overheat the house, keep the room temperature between 18 C and 20 C to keep the air humid. Too dry air makes symptoms worse.
- Ventilate the room regularly, even when it’s cold.
- Get enough sleep and avoid stressful situations.
- Consume vitamin C and honey daily in preventative doses.
Good to know! Rhinopharyngitis remains contagious for a long time, in some cases up to 21 days.
Treatment of the disease: physiotherapy and medication
In the majority of cases, nasopharyngitis goes away on its own, that is, the body overcomes it on its own. Therapy in this situation is aimed more at helping him, mitigating the symptoms and preventing the development of complications.
The main thing that is prescribed to the patient is bed rest or home rest, plenty of fluids and a fortified diet. You should avoid contact with other people, because the infectious disease is transmitted by airborne droplets.
Depending on the severity of symptoms, the following measures may be prescribed:
- rinsing the nose (nasal spray, sea or thermal water, saline);
- antiseptic gargling (with physiotherapeutic infusions and herbal decoctions), inhalations;
- use of vasoconstrictors and decongestants;
- taking antihistamines (if the disease is allergic);
- taking painkillers (for severe pain) and antipyretics (for fever);
- the use of dry cough syrups, which facilitate expectoration and help remove pathogens (if the cough is already wet, such drugs are not prescribed);
- lozenges to relieve sore throat;
- taking antimicrobial or antiviral drugs.
In mild cases, the last group of medications is not used at all, but if treatment requires more stringent measures, most likely, the specialist will prescribe antiviral drugs, because the most common pathogen is viruses. Antibiotics are prescribed when bacterial etiology is confirmed. Using them on your own will not only not help therapy, but can also harm it.
Complications
If acute nasopharyngitis is not treated, it can become chronic.
There is also a risk of developing the following complications:
- addition of a bacterial infection;
- laryngitis;
- sinusitis;
- sinusitis;
- tracheitis;
- inflammation of the middle ear (which can lead to hearing loss);
- bronchitis;
- pneumonia.
Respiratory infections can cause exacerbation of existing chronic diseases, such as bronchial asthma.