Author: Sozinova A.V., obstetrician-gynecologist, has been in continuous practice since 2001.
Weakness of labor is a pathological condition that is characterized by a decrease and weakening of contractions, as well as slow dilatation of the cervix. At the same time, the woman in labor becomes very tired and loses strength.
Weak labor can be primary or secondary.
Primary is a decrease in uterine activity that occurs at the very beginning of labor. The incidence is 5-7% of all births.
Secondary is a decrease in the duration, intensity and frequency of contractions after a favorable onset of labor. At the same time, the speed of dilation and effacement of the cervix also decreases, and the movement of the fetus along the birth canal slows down. Occurs in 2-3% of births.
Causes
Pregnant women who have a history of:
- childhood infections (rubella, chickenpox, measles);
- late onset of the first menstruation (menarche), after 15-16 years;
- menstrual irregularities;
- infantilism (small uterus);
- abnormalities of the uterus;
- inflammatory diseases of the reproductive system;
- a scar on the uterus (after a cesarean section, removal of fibroids, ectopic pregnancy, etc.);
- abortions;
- large fruit;
- a large number of births;
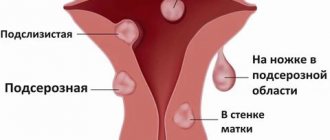
- uterine fibroids;
- diseases with metabolic disorders.
The reason for the weakness of the labor process can be mechanical obstacles (narrow pelvis, breech presentation of the fetus, inelasticity of the cervix). The age of the pregnant woman also plays a role - women under 17 and over 30 years of age are more susceptible to labor anomalies. Obstetric causes include:
- prenatal rupture of water;
- polyhydramnios,
- multiple births;
- post-term pregnancy or, conversely, premature birth;
- large size of the fruit;
- placenta previa;
- transverse or oblique position of the fetus;
- breech presentation of the fetus;
- fear of childbirth, great loss of strength.
The reasons may also be from the fetus:
- intrauterine infection;
- malformations and anomalies of development;
- Rhesus conflict;
- fetoplacental insufficiency.
Most often, the development of weak labor requires several reasons or a combination of them.
Preliminary stimulation of labor
If the family has already had cases of weak labor or there is reason to suspect that labor will be protracted, you can take care of a successful delivery in advance.
Pre-stimulation can be started at home from 34-36 weeks of pregnancy. It is based on the principle of doing what you couldn’t do in recent months: washing the floor while tilted, having sex, lifting heavy objects, taking hot baths.
You can also brew tea with raspberry leaves and drink 2-3 glasses a day. But in everything, of course, moderation is needed.
Signs of weak labor
Primary weakness of labor can be manifested by the following symptoms:
- contractions become less sensitive, rare or short;
- smoothing of the cervix and opening of the uterine pharynx slows down or stops (determined by the doctor during a vaginal examination);
- the presenting part of the fetus (head or pelvic end) remains mobile for a long time or pressed against the entrance to the pelvis;
- long duration of the first stage of labor (for primiparous women more than 12 hours, for multiparous women more than 10 hours) and, as a consequence, fatigue of the woman in labor;
- Possible untimely discharge of amniotic fluid.
Norms of dilation and contractions in the first stage of labor
Normally, in a primiparous woman, the cervix dilates by 1-1.2 cm per hour, in a multiparous woman - 1.5-2 cm per hour. If the cervix opens more slowly, this may indicate the development of primary weakness of labor.
In the first period, the normal duration of contractions is 20-30 seconds, and the interval between them is 7-10 minutes. With pathology of labor, their duration decreases, and the interval between them increases.
***
Secondary labor weakness is characterized by a longer period of fetal expulsion (more than 1–1.5 hours). This occurs due to the weakening or cessation of contractions, which at the beginning were intense, rhythmic and prolonged. At this moment, the progress of the fetus along the birth canal slows down or stops altogether.
Types of weakness of labor
In modern gynecology, primary and secondary weakness of labor are distinguished. The first type of weakness of labor is characterized by the fact that contractions from the very beginning are not strong enough, inactive, irregular and prolonged. In turn, secondary weakness of labor, the causes of which may be different, occurs when contractions weaken at the beginning of the 2nd or at the end of the 1st stage of labor, and initially labor is quite active and violent.
Convulsive and segmental contractions are also one of the types of weakness of labor. Convulsive contractions are protracted and last no more than 2 minutes. In turn, segmental contractions are characterized by contraction not of the entire uterus, but only of its individual parts. The effect of this kind of fight is almost zero.
Diagnostics
Primary weakness of labor is diagnosed based on:
- decreased activity of the uterus (contractions weaken and become rare);
- reducing the rate of smoothing of the cervix and opening of the uterine pharynx;
- prolonged standing of the presenting part of the fetus at the entrance to the pelvis;
- increasing the time of birth.
The diagnosis is also made on the basis of partogram data if there is no dynamics of cervical dilatation within two hours.
Partogram is a description of childbirth in a graphical way, which displays data on cervical dilatation, fetal advancement, pulse, blood pressure, fetal heartbeat, state of amniotic fluid, contractions, etc.
Secondary labor weakness is diagnosed based on the clinical picture and partogram data. In addition, it is necessary to monitor the condition of the fetus (listen to the heartbeat, install a CTG sensor), as there is a risk of developing hypoxia. After making a diagnosis, obstetricians need to decide on the tactics of labor management.
Weakness of labor must be distinguished from the following pathologies:
- pathological preliminary period (random false contractions with an immature cervix);
- discoordinated labor activity (impaired contractile activity of the uterus, manifests itself extremely painfully; occurs very rarely);
- clinically narrow pelvis (discrepancy between the sizes of the pelvis and the fetal head).
Sources of oxytocin
It’s not just the environment that influences labor. This is where we come to knowing about the three sources of oxytocin:
- Mom's pituitary gland
- Child's pituitary gland
- Placenta
Placental oxytocin
Most oxytocin is produced in the placenta. That’s why its functionality is important to us until birth. By creating a “favorable environment” we influence the production of mother’s pituitary oxytocin. This is influenced by the woman’s nervous system. We cannot influence the child’s oxytocin at all.
Child's pituitary oxytocin
Baby pituitary oxytocin must pass through the umbilical cord into the placenta, with the help of blood flow running back and forth. If the pace of labor is bad for the child, the speed does not suit him, then the baby will stop labor and “take away” his oxytocin.
I can’t stand the contraction after three minutes, “a little slower horse, a little slower
And against this background, we see a weakening of contractions and a suspension of opening.
Treatment and delivery of weak labor
There are several methods of medical care. The doctor makes a decision depending on the causes of the pathology and the condition of the mother and fetus. If labor is prolonged and becomes life-threatening, labor is induced or an emergency caesarean section is performed. Methods of medical care:
1. Stimulation of labor without medications. Labor can be enhanced by the amniotomy procedure (opening of the amniotic sac), which eliminates the use of medications. Don't be scared; amniotomy is completely painless.
2. Drug stimulation. Performed in case of ineffective amniotomy. It can be carried out with the help of strong analgesics that induce medicated sleep to relax and rest the woman in labor. Stimulation with oxytocin and prostaglandins is performed intravenously.
3. Caesarean section. Emergency surgery is performed if stimulation is ineffective and if there is a threat to the life of the woman in labor or the fetus.
Medication-induced sleep
For therapeutic sleep, sodium hydroxybutyrate and glucose are administered and performed by an anesthesiologist. In its absence, the obstetrician administers promedol, relanium, atropine and diphenhydramine. Medication-induced sleep allows a woman in labor to rest for 2-3 hours and gain strength, and also helps to intensify contractions. If there are indications for an emergency cesarean section, then there is no need for therapeutic sleep.
After the woman has rested, the doctor needs to assess her condition and the fetus, as well as the degree of dilatation of the uterine pharynx. After which a hormonal-energy background is created with the help of:
- ATP, riboxin, cocarboxylase;
- 40% glucose solution;
- calcium supplements (to enhance uterine contractions);
- vitamins: B1, B6, E, ascorbic acid;
- piracetam (to improve uterine circulation).
Amniotomy
Opening the membranes promotes the production of prostaglandins, which stimulate contractions. It is performed when the cervix is dilated by 3-4 cm. 2-3 hours after the procedure, the doctor needs to assess the state of the dynamics of cervical dilatation, and also decide on the use of contraction drugs.
Drug stimulation
When stimulated with drugs, oxytocin and prostaglandins are used.
Oxytocin is administered intravenously through a drip. It provokes increased contractions and the production of prostaglandins. Oxytocin is administered when the uterine pharynx is dilated by 5–6 cm or more, only after amniotomy or spontaneous discharge of amniotic fluid.
Prostaglandin E2 contributes to the development of normal contractions. The drug also accelerates the ripening of the cervix and its dilatation, without disturbing the uteroplacental circulation. The drug is administered similarly to oxytocin. It is used until the uterine os is dilated by 2-3 cm in case of an insufficiently mature cervix.
Prostaglandin F2a (enzaprost or dinoprost) is used when the uterine pharynx is dilated by 5 cm or more. Effects of the drug: stimulation of contractions, constriction of blood vessels, increased blood clotting. Therefore, it is contraindicated for gestosis and blood diseases. Prostaglandin F2a is administered intravenously using a drip system.
With drug stimulation, it is mandatory to prevent fetal hypoxia every 3 hours. To do this, a 40% glucose solution + ascorbic acid + aminophylline, sigetin or cocarboxylase is injected intravenously. Inhalation of humidified air is also indicated.
C-section
If all of the above methods are ineffective or there are additional indications, then a cesarean section is performed.
Contraindications to labor stimulation
- narrow pelvis (anatomical and clinical);
- presence of a scar on the uterus;
- women with a history of more than 5-6 births;
- incorrect position and presentation of the fetus;
- life threatening for the mother and fetus.
Discoordination of labor - symptoms and treatment
Discoordination of labor is a violation of the contractile activity of the uterus, in which different parts of the uterus (its right and left halves, fundus, body and lower sections) contract chaotically, uncoordinatedly [1][12].
The main signs of normal labor are:
- the presence of regular contractions, at least two in 10 minutes;
- structural changes in the cervix (from softening and smoothing to opening of the uterine pharynx), which arise and develop in response to uterine contractions [32].
If incoordination of labor develops, contractions can be very frequent (6-10 in 10 minutes), varying in strength and duration. However, the cervix does not open, or it does so very slowly. The uterus does not have time to relax between strong contractions, which causes severe pain to the mother in labor [3][5][12]. Severe pain syndrome tires the woman and causes anxiety.
As a primary pathology, that is, occurring in a relatively healthy woman in labor, this anomaly of labor occurs infrequently - in only 1-3% of births [2][4][9].
Causes of discoordinated labor
Among the main reasons for discoordinated labor, practicing obstetricians highlight the body’s unpreparedness for childbirth, which is most likely indicated by an “immature” cervix. The degree of maturity of the uterus can be determined using the Bishop scale.
Table 1 - Scheme for assessing cervical maturity according to Bishop [33]
| Factors | Score (score) | |||
| 0 | 1 | 2 | 3 | |
| Opening (cm) | closed | 1-2 | 2-4 | more than 4 |
| Cervical length (cm) | more than 4 | 3-4 | 1-2 | less than 1 |
| Consistency of the cervix | dense | partially softened | soft | |
| Position of the cervix relative to the wire axis of the pelvis | posteriorly | average | along the wire axis | |
| Location of the presenting part relative to the ischial spines (cm) | 3 cm higher | 2 cm higher | 1 cm above or at the level of the spines | 1-2 cm lower |
Preparing a woman’s body for the upcoming birth includes a number of changes:
1. Changing the dominant of pregnancy to the dominant of childbirth. The term “maternal dominant” refers to a woman’s psychological readiness to bear, give birth and feed a child. At the same time, a focus of excitation is formed in the woman’s body at the level of the central nervous system (CNS), which is characterized by dominant (predominant) ideas of pregnancy and an acute desire to have a healthy child, which is also reflected in the hormonal balance. The term “maternal dominant” was proposed by the Russian physiologist I. A. Arshavsky in the 60s of the 20th century. This concept includes the dominants of pregnancy (gestational dominant), childbirth and feeding, which normally successively replace each other [23][24].
Observations by scientists prove that if a woman is ready to bear a child, but by the time of birth she has not developed a dominant of labor, then labor activity is inactive, or complications arise. In this case, it is necessary to revise the birth plan in favor of a cesarean section [23][24].
2. Hormonal fluctuations are another mechanism for the onset of labor. Hormonal fluctuations mean an increase in estrogen levels and a decrease in progesterone. Progesterone prevents the excitability of the uterus during pregnancy and thereby prevents the expulsion of the fetus. Estrogens, on the contrary, increase the contractile activity of the uterus.
3. Metabolic changes, such as an increase in the rate of oxygen consumption, also affect the onset of labor.
Thus, under the influence of specific changes in the excitability of the central nervous system, as well as as a result of hormonal fluctuations and metabolic changes in the mother’s body, structural changes occur in the uterus and cervix. Disturbances at any stage of the body’s preparation for the birth of a child increase the risk of complications during childbirth, in particular, the risk of discoordinated labor increases [5][14][17].
The exact causes of discoordination of labor have not been sufficiently studied, but the main factors are identified (Sidorova I. S., 2006) [33]:
1. Disruption of the autonomic nervous system , which regulates the activity of internal organs, endocrine and exocrine glands, blood and lymphatic vessels:
- Overexcitation of the hypothalamus.
- Weakening of the leading role of the central nervous system.
- Absence of dominant genera.
Such disorders can arise due to vegetative neuroses, stress and severe overwork. As a result of nervous agitation, unwillingness to cooperate with the doctor and listen to the advice of the obstetric team, a woman’s breathing becomes impaired during labor, which prevents the uterus from relaxing outside of contractions in order to maintain the productivity of labor.
2. Pathology of the myometrium and cervix:
- Malformations and hypoplasia (underdevelopment) of the uterus. Anomalies in the development of the uterus mean its irregular structure: bicornuate/unicornuate, saddle-shaped, double uterus or intrauterine septum. If a woman has a similar pathology, complications may arise both during pregnancy planning and during pregnancy and childbirth, since abnormalities in the development of the uterus predispose to abnormal position of the fetus during childbirth.
- Inflammatory and cicatricial deformation of the lower part of the uterus, for example as a result of endomyometritis - inflammation of the inner mucous layer of the uterus (endometrium) and muscle layer (myometrium).
- “Hard” cervix due to the replacement of muscle and collagen fibers with connective tissue. The reason for such replacement may be treatment of cervical pathology (for example, cauterization for cervical dysplasia), birth trauma during previous births (cervical rupture), non-treatment of inflammatory diseases of the cervix and vagina (cervicitis, colpitis, etc.).
3. Presence of mechanical obstacles during childbirth:
- Changes in pelvic anatomy. They can be congenital or acquired, for example, as a result of injuries, tumors, polio or rickets suffered in childhood, etc. Changes in the structure of the pelvis imply different types of the so-called narrow pelvis: a transversely narrowed pelvis, a simple flat pelvis, a uniformly narrowed pelvis. There are also more rare forms, including an oblique pelvis or a pelvis narrowed by exostoses (bone protrusions or tumors) due to fractures and injuries to the pelvis or sacral region of the spine. The main difference between a normal pelvis and an anatomically narrow one is a decrease in at least one of the dimensions of the pelvis compared to the norm by 1.5-2 cm.
- Asynclitic insertions of the fetus. Asynclitism is a pathological insertion of the fetal head into the plane of the small pelvis, in which the sagittal suture on the baby’s head is deviated towards the sacrum or pubic symphysis, which impedes movement along the birth canal. However, such pathology is rare: 0.1-0.3% of all births [1].
- Dense amnion (inner membrane of the fetus), which creates functional inferiority of the fetal bladder.
- The presence of myomatous nodes in the lower segment of the uterus, including on the cervix.
To overcome these obstacles, the uterus works more intensely (i.e., it is in hypertonicity) and sometimes this leads to disruption of the synchrony of contractions.
4. Fetoplacental insufficiency (impaired function and structure of the placenta). It is believed that it is the relationship between the fetoplacental system and the maternal body that determines how pregnancy and childbirth will proceed.
5. Non-synchronous preparation of the organisms of the woman and the fetus for the process of childbirth.
6. Reduced protective effect of the anti-stress system of the mother's brain: decreased production of neurohormones - endorphins, enkephalins, dynorphins. This situation is possible when the mother is psychologically unprepared for childbirth, which is expressed by fear for herself due to an increased threshold of pain sensitivity, fear of the hospital, a white coat or injections, and fear for the child. Anxiety of this kind may appear after stories from friends/acquaintances or watching videos on the Internet. As a result, low awareness of expectant mothers about the process of childbirth and postpartum recovery prevents the body from adjusting to childbirth [22].
7. Iatrogenic factors, i.e. provoked by the actions of medical workers :
- Hyperstimulation of labor with oxytocin in the absence of indications or without taking into account contraindications. Oxytocin remains the main means of artificially inducing labor. However, there are strict indications for its use; in addition, the technique and the dosage of the drug are important. Existing regimens for inducing labor differ in dose and interval of its increase. In this regard, low-dose and high-dose regimens are distinguished. In practical obstetrics, the technique of sequential use of amniotomy (opening the amniotic sac) and the administration of oxytocin to artificially stimulate the labor process is widespread, although there is no evidence regarding the technology and effectiveness of this technique. At the same time, modern data, namely the clinical protocol for preparation of the cervix for labor and induction of labor from 2012, the basic protocol for the management of labor, as amended in 2021, as well as the Royal College of Obstetricians and Gynecologists' guidelines for induction of labor (RCOG, 2008) The simultaneous use of amniotomy and the administration of oxytocin is not recommended. The sequential choice of amniotomy and oxytocin infusion as the main method of induction of labor is also not recommended due to the high likelihood of developing uterine hyperstimulation and discoordinated labor [6][20][21].
- Insufficient pain relief during labor, which leads to general muscle tension.
- Untimely removal of flat membranes.
- Rough research and manipulation.
In addition to those mentioned, other factors of anomalies of generic forces are identified (Aylamazyan E.K., Kulakov V.I., 2009) [1][40]:
1. Obstetric factors:
- Premature rupture of water.
- Pelvic cephalic disproportion (clinical narrow pelvis). This is a condition in which there is a discrepancy between the sizes of the fetus and the woman's pelvis, regardless of the size of the latter. This situation can be expressed at the beginning of labor by excessive, discoordinated uterine contractions that do not respond to conservative therapy.
- Overdistension of the uterus , which occurs as a result of the development of multiple pregnancies, polyhydramnios, changes in the position of the fetus, or post-term pregnancy (more than 42 weeks).
- Placenta previa (the placenta is located in the lower parts of the uterus and completely or partially covers the internal os of the uterus).
- Gestosis (late toxicosis of pregnancy).
- Anemia of pregnant women.
2. Factors that are associated with pathology of the reproductive system:
- Infantilism (lag in physical development).
- The woman's age is over 30 and under 18 years. Research by O. R. Baev (2005) [8] indicates a high incidence of discoordination of uterine contractions in young primigravidas [22].
- Menstrual irregularities and low stress resistance, according to the study of Bologova M. A. and Penzhoyan G. A. (2018) [7], are also included in the group of possible causes of this pathology.
- Neuroendocrine disorders: premenstrual syndrome (PMS), polycystic ovary syndrome (PCOS), hyperprolactinemia syndrome, etc.
- History of induced abortions.
- Miscarriage.
- Operations on the uterus.
- Inflammatory diseases of the cervix and vagina.
3. General somatic diseases : obesity, metabolic syndrome, as well as hypertensive complications of pregnancy (increased blood pressure), which develop against the background of chronic arterial hypertension or first appear after the 20th week of pregnancy (gestational) [1][12][13].
4. Fetal factors:
- Fetal growth retardation is a discrepancy between the physiological parameters of the fetus and the norms that are typical for a certain period of pregnancy.
- Intrauterine infections of the fetus: rubella, cytomegalovirus infection, viral hepatitis, etc.
- Developmental defects, such as anencephaly, in which the structures of the cerebral hemispheres are completely absent.
- Overripe fruit.
- Immunological conflict during pregnancy, for example due to the Rh factor.
Poor physical development associated with unfavorable social factors, malnutrition, or a combination of both, can also cause the development of incoordination during childbirth [3].
Possible complications
In case of incorrect choice of delivery strategy during weak labor, the following complications are possible:
- abuse of stimulant drugs can lead to discoordinated labor and fetal hypoxia.
- prolonged standing of the presenting part of the fetus in one plane of the small pelvis can lead to compression of the soft tissues, which leads to the risk of genitourinary fistulas. On the part of the fetus, this can lead to impaired cerebral circulation and cerebral hemorrhage.
- Women with weak labor in the postpartum period have a risk of hypo- and atonic bleeding and infectious diseases.
What it is?
Childbirth is the final and most anticipated stage of the entire pregnancy period. But childbirth does not always go smoothly. One of the forms of dysfunction of the contractile function of the uterus is weakness of labor. This pathology is characterized by the fact that contractions are rare and irregular, the myometrial tone is clearly low, and the amplitude of contractions is weak. The diastole of contractions (the period of relaxation) significantly exceeds the systole (the period of contraction), which negatively affects the opening of the uterus, and the fetus cannot advance normally. The uterus stops performing its functions properly, which poses a threat to the baby.
In gynecology and obstetrics, labor weakness is called one of the most common disorders and complications of the childbirth process. It is the weakness of labor that most often leads to the occurrence of pathologies in the fetus and mother. Among all birth pathologies, according to statistics, weakness of labor accounts for about 7% of cases. It is worth noting that this anomaly is more common in women giving birth for the first time than in those women who are not having their first birth.
Forecast
With adequate medical care, the prognosis for the woman and fetus is favorable. Much depends on the psychological state of the woman; there is no need to panic or be afraid; it is better to listen to the recommendations of the obstetrician. Serious complications are quite rare.
Some studies during pregnancy
- Smears during pregnancy
- Pregnancy tests by trimester
- Ultrasound during pregnancy
- General urine test during pregnancy
- Coagulogram
- Installation of a pessary
- Glucose tolerance test
- Homocysteine during pregnancy
- Amniocentesis
- Anesthesia during childbirth
- Fetal CTG (cardiotocography)
- Cordocentesis
- Epidural anesthesia during childbirth