Hallux valgus is a common condition that is also known by several other names. Doctors talk about hallux valgus and hallux valgus. People not associated with medicine simply call it “ossicle” or hallux valgus.
The pathology is easy to determine. A thickening in the form of a callus appears on the inside of the foot. It hurts periodically and gradually increases in size. At the same time, the big toe begins to deviate towards the second toe and, in advanced cases, crosses with it. Along with aesthetic imperfections, a serious problem arises: the inability to use shoes, even everyday ones. The next stages in the development of the disease are arthritis and bursitis, the inability to move independently.
Most often, the first toe is deformed in women who prefer to wear high-heeled shoes (above 4 cm). In addition, this is an occupational disease of ballerinas. Excessive loads do not make themselves felt immediately, but after a while, when it is already difficult to correct the situation.
Surgical methods of treatment
Globally, all operations to remove hallux valgus are divided into minimally invasive and open. Minimally invasive ones are performed through small incisions in the skin. In most cases, there is no need for stitches. Recovery is quick and easy.
There are three categories of open surgical interventions:
Manipulation of soft tissues.
An example is the McBride operation. The muscles and ligaments of the foot are cut. Bones are not affected. The intervention is effective for minor deformities and can be performed in case of contraindications from the osteoarticular system.
Osteotomy.
An artificial fracture of the metatarsal bone is performed. The doctor selects the location of the fracture. Due to this, the position of the metatarsus is corrected
Arthrodesis.
The operation is used in advanced stages of hallux valgus deformity, when it is necessary to return the physiological shape of the joint.
The doctor, from all the methods of surgical intervention available to him, selects the one that best solves the problems of a particular patient.
The operation requires preliminary preparation. We need to get some test results. These include clinical and biochemical blood and urine tests, a blood test with a detailed coagulogram, and tests for blood-borne infections. Electrocardiography is prescribed, and x-rays of the foot are performed (necessarily in two projections).
If no contraindications to surgery to remove hallux valgus are identified, the method of anesthesia is agreed upon. Most often, local anesthesia is sufficient.
Causes
Many problems that arise in the legs are the result of abnormal pressure or friction. The easiest way to determine the presence of the consequences of pathological pressure is to examine the leg. The leg is a hard bone covered with skin. In most cases, symptoms develop gradually as the skin and soft tissues absorb the excess impact on the leg. Any protruding bone or injury aggravates the already existing consequences of the injury. The skin reacts to friction and pressure by forming a callus. The soft tissues located under the skin react to excess stress. Both the callus and the thickened soft tissue underneath the callus become painful and inflamed. Reducing pain helps to reduce pressure. Pressure can be reduced externally through looser shoes or internally through surgery and removal of excess tissue.
Distal osteotomy
The most common surgical method for correcting hallux valgus deformity is distal osteotomy. The operation takes place in several stages:
First stage
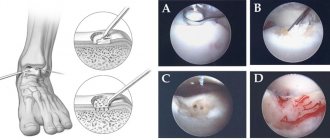
Exostoexotomy or removal of the “bone”. In untreated cases, this stage may be the only one. Through a small skin incision or even without an incision, endoscopically, the exostosis itself (bone) and the inflamed joint capsule are removed.
Second phase.
Remote osteotomy. Using an artificial fracture, the position of the first metatarsal bone is leveled. The fracture site is secured with titanium screws. They are removed a month later, after the bone has completely healed.
Third stage.
Dissection of the muscle responsible for abducting the thumb.
Fourth and final stage.
Securing the thumb in a physiological position.
Prevention of pathology
In order for the child’s leg to form correctly, parents should take the following actions:
- choose the right shoes for your baby, strictly in size;
- exclude any causes that may provoke the appearance of deformation;
- provide the child with adequate nutrition, a normal daily routine, and adequate physical activity including walking barefoot on any uneven surfaces;
- equip a wall bars or its equivalent in the children's room.
If parents notice that the baby’s leg is tilting to one side, or there are other signs of deformation, they should immediately consult with an orthopedic doctor.
Surgical treatment of hallux valgus: indications
It is possible to correct the position of the thumb using conservative methods in childhood, when the bone skeleton is still developing. In all other cases, only surgery will help. The main indications are:
- discomfort when walking due to unbearable pain;
- deviation of the joint by several tens of degrees;
- a significantly protruding bone, making it impossible to wear shoes;
- violation of the position of the foot, making it difficult to move;
- swelling of the thumb;
- inflammatory manifestations and other complications of hallux valgus.
The doctor determines the indications individually for each patient. Typically, surgical methods are used when conservative methods (conventional methods, without surgery) become ineffective.
Women over 30 years of age most often come to our Clinic with this problem. Main reasons:
- heredity
- wearing uncomfortable shoes
- excessive physical activity
- overweight
- hormonal changes (including after pregnancy)
- inflammatory processes in the joints
- consequences of injuries or unsuccessful surgical interventions.
At first, protruding bones seem to be a cosmetic defect; over time, pain appears, the motor ability of the foot is impaired, and as a result, arthrosis of the knee and hip joint, osteochondrosis and other pathologies associated with the musculoskeletal system develop. Depending on the severity of the deformity, various surgical techniques are used for treatment. At the initial stages of deformation, treatment must begin with conservative methods.
Establishing diagnosis
Before prescribing treatment, our specialists conduct a thorough diagnosis of the patient; during this diagnosis, the etiology (origin of the disease) and severity are identified. There are international standards by which all orthopedic traumatologists classify pathology according to the same principles, namely:
- Static.
The deformation occurred due to poor posture - Congenital.
The disorder is associated with a genetic feature of the position of one of the bones of the foot - Compensatory.
In this case, the deformation is a response to the anatomical feature of the tendon, as a result of which the tibia changes position and deforms the ankle joint; - Paralytic deformity.
Occurs after polio or other inflammatory processes in the central nervous system; - Spastic
. It is a complication of muscle spasms; - Hypercorrectional.
In case of improper treatment of foot pathologies; - Traumatic.
It is a complication of fractures and ligament injuries.
The significance of this classification is that treatment of pathology is impossible without addressing the cause. The operation will relieve the patient of deformity and lead to a normal lifestyle. And influencing the etiology of the disease will help avoid the reappearance of deformity.
Depending on the severity, hallux valgus deformity can be:
- Easy
- Average
- Heavy
The method of treating the patient depends on the severity of the disease.
Myths about surgery to remove hallux valgus
There are many myths among people regarding surgical removal of a bunion. Let's dispel some of them.
You cannot have surgery if you have arthritis or arthrosis. In fact, these diseases are considered relative contraindications. The operation is possible, the doctor will just treat you with more attention.
It is useless to operate: the bone will soon grow anyway. With a high-quality intervention, the probability of re-development of hallux valgus deformity tends to zero. Relapses occur, but are extremely rare.
You will have to sit for a long time without moving and wear a cast. Modern technologies make it possible to move independently within a few hours after the procedure. The bones are held together by special structures, so there is no need for plaster.
Severity and types of disease
Hallux valgus develops gradually, going through four stages of development:
- First degree. The deviation from the vertical axis is no more than 15 degrees. Timely correction leads to complete cure.
- Second degree. The lower part of the legs is turned out 15-20 degrees. Complex conservative treatment gives a good result, completely eliminating the defect.
- Third degree. The deviation from the axis is 20-30 degrees. Therapy includes a number of activities and lasts several months and even years.
- Fourth degree. The deformation angle exceeds 30 degrees. Conservative treatment does not always give a positive result, so in approximately 7% of cases surgical correction is performed.
Varus curvature has three degrees of severity:
| Degree of damage | Heel angle in degrees | Arch angle | Longitudinal arch height |
| 1 | up to 15 | up to 150 | 15-20 mm |
| 2 | up to 20 | 150-160 | 10 mm |
| 3 | more than 20 | 160-180 | less than 10 mm |
How to recover after surgery
The recovery period after surgery to remove hallux valgus is extremely important. It is 4-6 months. The doctor gives detailed instructions on how to behave during the recovery period.
There are also general aspects of rehabilitation that all patients need to know about.
First and second day. Bed rest. You can move around, but it’s better not to get active. It is recommended to keep your leg elevated and occasionally, if there is no pain, move your toes.
The third day. You can start moving slowly. It is important to choose a comfortable orthosis and shoes, which after surgery should be special, removing the load from the operated part of the foot. In most cases, Baruk shoes (the French surgeon who invented them) are used, which relieve the load on the forefoot when walking. At first, to get used to it, you can provide yourself with additional support in the form of a cane or crutches. After three to five days they will no longer be needed.
10-14 days. Period of doctoral supervision. In the case of a serious operation, the patient may spend all this time in the clinic. Physical therapy and physiotherapy sessions are recommended. It is not advisable to stand on your feet for a long time.
After 1-1.5 months, there is no need for an orthosis, but after surgery it is better to use shoes with suitable orthopedic insoles.
After 2 months, you can exercise on exercise bikes and swim in the pool.
Swelling of the foot and ankle may persist for up to three months. At this time, it is recommended to use cool compresses and wear compression stockings.
After 4-6 months, it is possible to move around without an orthosis, resume sports, and wear high-heeled shoes. High-quality recovery and quick rehabilitation require choosing comfortable wide shoes. Don’t forget to create comfortable conditions for your feet so that the unpleasant situation does not happen again.
Hallux Valgus - hallux valgus deformity (bone on the big toe)
Bunion on the big toe, hallux valgus, hallux valgus, hallux valgus, Hallux Valgus - all these names refer to the same pathology.
Hallux Valgus (Hallux Valgus) - medial (internal) deviation of the first metatarsal bone and lateral (external) deviation and internal rotation (rotation around its axis) of the first toe. In fact, it is not a simple deformity of the first metatarsophalangeal joint, but a complex deformation of the entire medial ray of the foot. Often accompanied by symptomatic deformities of the second toe. There are two forms: hallux valgus in adults and adolescent/juvenile hallux valgus.
The term hallux valgus was first introduced in 1871 by Carl Heuter, who referred to the outward deviation of the first toe from the central axis of the body. In the 19th century, it was widely believed that hallux valgus was a consequence of the overgrowth of the bone tissue of the first metatarsal and its soft tissue membrane due to poorly fitting shoes. Therefore, surgical treatment most often boiled down to excision of soft tissue and removal of exostosis. Surgeons for a long time considered this pathology uninteresting, which largely explains the slow development of understanding the causes of this disease. The first operation aimed at correcting the deformity was performed by Reverdin on May 4, 1881 in Genfer; after removing the exostosis, a wedge-shaped resection was performed on the opposite side, which became the prototype for subsequent operations to correct valgus deformity using osteotomy. Since this very first osteotomy, numerous modifications have been proposed, with the addition of lateral release, proximal osteotomy, Z-shaped osteotomy, distal osteotomy - about 150 different operations in total. Many modifications differed little from each other and might seem identical to an inexperienced specialist. But even now the search for the best osteotomy continues in order to achieve the most stable and reliable result.
Hallux valgus is a widespread pathology. According to the US Department of Health, it occurs in 1% of the population. In his study, Gould found an increase in frequency with age: according to his data, 3% of the population aged 15-30 years, 9% of those aged 31-60 years and 16% of people over 60 years old have hallux valgus. There is also a predominance of Hallux Valgus among women (according to various sources, 2-4 times more often than in men), although it is quite possible that this relates to the frequency of visits, which in turn may be associated with women’s desire to wear uncomfortable shoes and cosmetic requests, and not a pain syndrome. It has also been noted that there is a genetic predisposition to Hallux Valgus, with the disease spreading in families, but specific genes responsible for the development of the disease have not yet been identified.
Despite popular belief, high-heeled shoes and shoes with narrow toes do not cause Hallux Valgus. But, in the case when such a deformation already exists, these types of shoes lead to excessive trauma to the soft tissues on the inside of the first metatarsophalangeal joint, which provokes pain. In addition, tight shoes themselves can provoke medial pain and nerve compression. It is impossible to single out a single cause for Hallux Valgus; today experts agree that it is a multifactorial disease with a complex of biomechanical, traumatic and metabolic causes.
The most common and most difficult to understand theory is biomechanical instability. It is provoked by gastrocnemius and gastrocnemius-soleus equinus, dynamic or rigid planovalgus deformity of the foot, dynamic or rigid varus deformity of the metatarsus, dorsiflexion of the first ray, hypermobility of the sphenometatarsal joint, or a short first metatarsal bone. Most often, excessive pronation (internal rotation) in the tarsal and subtalar joints compensate for the above deformities during the gait cycle. Moderate pronation of the foot is necessary to absorb the impact of the foot on the ground when walking. However, excessive pronation creates excessive hypermobility of the tarsus, which in turn disrupts stability and prevents the reverse process of resupination in the gait cycle. This leads to the formation of a persistent lever, which makes pushing with the foot difficult.
For normal foot propulsion, 65° of dorsiflexion (dorsiflexion) is required in the first tarsometatarsal joint, only 20-30° of which occurs due to the big toe itself. The remaining 40° occurs due to plantar displacement of the first metatarsal in the sesamoid complex. For this reason, to push, you have to increase the plantar flexion of the first ray of the foot at the level of the first metatarsophalangeal joint, in the sesamoid complex. This leads to significant overload of the first metatarsophalangeal joint and provokes the development of valgus deformity of the first toe. If, due to hyperpronation of the tarsus, the joints of the foot acquire excessive mobility, a transverse spreading of the foot occurs, the 2-4 metatarsal bones begin to shift outward, and the first metatarsal bone, on the contrary, inward, the overloaded sesamoid complex continues to pull on the base of the main phalanx of the first toe, which in turn leads to outward deviation of the first toe. In the absence of such hypermobility, Hallux Rigidus is formed.
Metabolic disorders that lead to hallux valgus include gout, rheumatoid arthritis, psoriatic arthritis, and connective tissue diseases such as Ehlers-Danlos syndrome, Marfan syndrome, Down syndrome, and laxity syndrome. Neuromuscular causes include multiple sclerosis, Charcot-Marie-Tooth disease, and cerebral palsy. Also, traumatic causes can lead to hallux valgus deformity: fractures of the bones of the medial ray, post-traumatic arthrosis, dislocations of the first toe, turf toe, etc. Also provoking factors can be anomalies in the length of the metatarsal bones, varus and valgus deformity of the knee joint, retrotorsion of the hip.
Normally, during walking, the hallux and the remaining toes remain parallel to the longitudinal axis of the foot, regardless of adduction and internal rotation of the foot. This is due to the strength simultaneously transmitted through the tendon of the adductor pollicis, extensor hallucis, and flexor hallucis muscles. In case of increased mobility of the joint, the extensor of the thumb, passing more laterally (outward) from the central axis, begins to shift the first finger in its direction. In this case, the tendons, stretching while walking, work like a bowstring, leading to the arching of the entire first ray in the inward direction. The head of the first metatarsal bone, moving inwards, leaves the sesamoid bones on the outside. The sesamoid bones, located in the thickness of the flexor pollicis brevis and longus, normally act as a block that enhances muscle strength by changing the load vector, and also bear a significant proportion of body weight. When they are displaced laterally, the load falls on the heads of the first and second metatarsal bones, which leads to metatarsalgia. The medial portions of the capsule of the first metatarsophalangeal joint are tense, while the lateral portions are contracted. Next, the adductor pollicis muscle becomes the main deforming force. Continued outward deviation of the thumb causes the attachment of the adductor pollicis muscle to shift outward and plantar. From this moment, instead of adduction, this muscle begins to flex and internally rotate the main phalanx of the thumb.
Changing the direction of force vectors during valgus deformation of the first toe.
Most often, patients present with gradually increasing deep or acute pain in the area of the first metatarsophalangeal joint when walking, which indicates degenerative changes in the articular cartilage. The patient may also complain of pain in the area of the head of the first metatarsal bone when wearing shoes, while the pain goes away when walking barefoot, which is associated with irritation of the soft tissues along the inner surface of the first metatarsophalangeal joint. Often both types of pain occur. The pain gradually progresses and at the time of treatment, many years may have passed since its onset. Along with the pain, the deformity also progresses. At this stage, it is important to eliminate the metabolic causes of pain that require drug treatment. Another possible symptom may be burning pain or tingling in the area of the dorsum of the big toe and the first metatarsophalangeal joint, which occurs when the medial cutaneous nerve is involved in the scarring process. In addition, patients often complain directly about deformation, changes in the second finger, callus formation, skin damage, sometimes without characteristic complaints of pain.
Inspection. During examination, it is important to identify the main cause and leading deformity, which affects further treatment tactics. It is necessary to examine the entire lower limb: internal and external rotation of the hip, valgus and varus deformity of the knee joint, tibial torsion, dorsiflexion in the ankle joint, range of motion in the subtalar joint, range of motion in the tarsal joints, neutral position of the calcaneus, valgus/varus deviation of the posterior and forefoot. It is also necessary to assess the degree of elasticity/rigidity, assess the severity of deformation without load and under load. The position of the hallux is assessed relative to the second toe, the degree of valgus displacement, internal rotation, and subluxation in the first metatarsophalangeal joint is assessed.
Next, the range of motion of the first metatarsophalangeal joint is measured; the norm is dorsiflexion up to 65° and plantar flexion up to 15°. During the assessment of range of motion, the presence of crepitus and the severity of pain during movement are also checked. Such findings indicate dystrophic changes in the articular cartilage of the first metatarsophalangeal joint; pain without crepitus indicates its synovitis. The next step is to measure the amplitude of active movements, and it is necessary to pay special attention to whether the deviation of the hallux to the outside increases during movements, as this indicates an adhesive process in the area of the outer part of the joint capsule. Subsequently, the range of movements in the first wedge-metatarsal joint is assessed, the total amplitude in the plantar-dorsal direction does not normally exceed 10 mm, the amplitude of movements in the transverse plane is normally close to zero.
The next step is to evaluate the skin for pressure zones. A callus in the area of the first interdigital space indicates excessive overpronation of the first toe during walking.
A callus in the area of the head of the first metatarsal bone signals equinus position of the foot, rigid plantar flexion of the first metatarsal bone, hypertrophic growths of the sesamoid bones, rigid valgus deformation of the tarsus or cavus foot. A callus in the area of the head of the second metatarsal indicates a shortened first or elongated second metatarsal, dorsiflexion of the first metatarsal, retrograde plantarversion of the second toe due to the formation of a hammertoe deformity of the second toe, or hypermobility of the first metatarsal.
Extensor hallucis longus contracture occurs only with long-term lateral subluxation of the first metatarsophalangeal joint or neuromuscular lesions.
Competing deformities such as hammertoe deformity of the second toe, hypermobile or rigid planovalgus foot are often found. Instability and deformation of the second toe often aggravates and accelerates hallux deformity as the natural obstacle to its further displacement disappears.
A very important element of the examination is the assessment of the foot under load: an increase in the degree of abduction of the first toe, adduction of the first metatarsal bone, the appearance of dorsiflexion indicating contracture of the extensor pollicis longus.
Instrumental diagnostic methods. To confirm the diagnosis of hallux valgus and preoperative planning, radiographs are used in direct, lateral, and sometimes oblique and sesamoid projections. The main parameters that are assessed radiographically are:
1. hallux valgus angle (normally less than 15°)
2. intermetatarsal angle (normally less than 9°)
3. Distal metatarsal articular angle (normally less than 15°)
4. Interphalangeal angle hallux valgus - the angle between the proximal phalanges of the first and second fingers (normally less than 10°)
X-ray determination of angles for hallux valgus deformity of the first toe.
The first stage of treatment is shoe correction, making insoles, and using special inserts and devices. If conservative treatment is ineffective (pain persists when walking), as well as in the presence of overlapping fingers, hammer-shaped deformity of the second finger, neuritis of the digital nerves, sesamoiditis, inflammatory changes in the area of the deformity, surgical treatment is indicated.
Surgical treatment methods can be divided into the following groups:
1) operations on soft tissues
2) distal osteotomy (for mild cases, intermetatarsal angle less than 13°)
3) proximal or combined osteotomy (for more severe degrees, intermetatarsal angle more than 13 °)
4) arthrodesis of the first wedge-metatarsal joint (if it is unstable or arthritis)
5) other arthrodeses (for severe deformity, spasticity, arthrosis)
6) resection arthroplasty (in the group of elderly patients with low functional demands)
In the case of juvenile Hallux Valgus, it is advisable to delay the operation as much as possible. If this is not possible, it is better to use operations that do not affect the proximal part of the metatarsal bone.
Degrees of hallux valgus . The severity of the deformity is assessed using radiography; each degree corresponds to a specific surgical tactic. The need for surgical intervention is largely determined by the severity of the pain syndrome and limitations in the patient’s daily activity, rather than by a cosmetic defect.
| Deformation degree | Valgus angle | Intermetatarsal angle | Additionally | Operation |
| Light | <25° | <13° | Distal osteotomies | Chevron osteotomy + McBride operation, + Akin for interphalangeal hallux valgus |
| Average | 26-40° | 13-15° | Proximal ± distal osteotomy | Chevron osteotomy + McBride operation, + Akin |
| Proximal osteotomy + McBride operation | ||||
| Heavy | 41-50° | 16-20° | Double osteotomy | Proximal osteotomy + Chevron osteotomy + McBride operation |
| Lapidus operation + Akin osteotomy | ||||
| Elderly\with low demands | Keller osteotomy | |||
| Juvenile hallux valgus | Osteotomy of the sphenoid bone (young age), double osteotomy (if skeletal maturity allows) |
Soft tissue operations. Modified McBride operation
Most often used for moderate deformity (hallux valgus angle less than 25°, intermetatarsal angle less than 15°), often performed simultaneously with resection of the internal tuberosity, osteotomy of the first metatarsal bone, arthrodesis of the first wedge-metatarsal joint (Lapidus). The essence of the McBride operation is to cut off the adductor pollicis muscle from the fibular sesamoid bone, lateral capsulotomy, and tension the medial capsule due to its duplication. The operation can be supplemented by suturing the tendon of the adductor pollicis muscle to the outer part of the joint capsule, or directly to the head of the first metatarsal bone.
Modified McBride operation for hallux valgus.
Distal metatarsal osteotomies.
Suitable for moderate deformity (hallux-valgus angle less than 40°, intermetatarsal angle less than 13°)
The most common is the Chevron osteotomy. It is possible to use more proximal and more distal options, followed by installation of the screw in an oblique longitudinal or transverse plane. (https://www.youtube.com/watch?v=pcXjb-ghohM).
Chevron osteotomy for hallux valgus
Below are other options for distal osteotomies for hallux valgus.
Mitchell osteotomy for hallux valgus.
Austin osteotomy for hallux valgus
Proximal osteotomies. Indicated for moderate severity of the disease (hallux-valgus angle more than 40°, intermetatarsal angle more than 13°). The most common are cross osteotomy, scarf osteotomy, wedge osteotomy, and Ludloff osteotomy.
Cross osteotomy - provides high stability and large room for maneuver in correcting both the medial deviation of the metatarsal bone and its length.
Ludloff osteotomy for hallux valgus
Scarf osteotomy is one of the most popular treatments for Hallux Valgus, along with chevron osteotomy. (https://www.youtube.com/watch?v=8wmvARFjZVM&index=3&list=PLYUX9ZYOBxWzyRTn_HqBMKqMynuvXp1sV)
Scarf osteotomy for hallux valgus.
Double (proximal + distal) osteotomies are used in cases of severe deformities (hallux-valgus angle more than 40°, intermetatarsal angle 16-20°).
Wedge-shaped osteotomy of the base of the first metatarsal bone. It is used in cases where it is desirable to increase the length of the first metatarsal bone. Can be performed without the use of any metal fixators. Indicated for young patients with moderate deformity.
Wedge-shaped osteotomy of the base of the first metatarsal bone.
Osteotomy of the first cuneiform is used in cases of juvenile hallux valgus when osteotomy of the first metatarsal cannot be performed due to unclosed growth plates.
Osteotomy of the first sphenoid bone.
The Akin osteotomy often complements the Chevron and other osteotomies in cases where correction of the medial deviation of the first metatarsal is not sufficient to bring the big toe into its normal position.
Lapidus operation for hallux valgus.
Arthrodesis of the first metatarsophalangeal joint. Used in the treatment of hallux valgus in cases of cerebral palsy, Down syndrome, rheumatoid arthritis, gout, severe arthritis, Ehlers-Danlos syndrome.
Arthrodesis of the first metatarsophalangeal joint.
Resection arthroplasty (Keller operation). Practically not used. Sometimes indicated for elderly patients with low functional demands.
Keller's operation for hallux valgus.
After surgical treatment of hallux valgus of 1 finger, a 6-month rehabilitation period follows. It can be divided into 3 stages: acute postoperative period (0-6 weeks), recovery rehabilitation period (6-12 weeks), long-term rehabilitation period (12 weeks - 6 months).
The first day after surgery - bed rest, elevated position of the lower extremities, local cold - 20 minutes 5-6 times a day, analgesics.
The second day after surgery - dressing, moderate walking in special shoes,
Shoes for unloading the forefoot.
elevated position of the lower extremities, local cold - 20 minutes 5-6 times a day, analgesics.
As the pain subsides, the range of passive movements in the foot joints gradually begins to develop.
Two weeks after surgery - removal of sutures, continuing to increase the range of passive movements. Walking in special shoes. For pain - elevated position of the lower extremities, local cold, analgesics.
Six weeks after the operation - control radiography, if the picture is satisfactory - a gradual transition to regular shoes, development of the range of active movements.
12 weeks after surgery - complete transition to regular shoes, the beginning of light sports activity.
Six months after surgery - complete recovery, no restrictions.
The most common complication is the recurrence of deformity (from 2 to 16%). The reason may be an underestimation of the degree of deformity, insufficient correction of the intermetatarsal angle, or inadequate ligamentous balance. It can also be triggered by the patient’s failure to comply with the rehabilitation protocol.
Infectious complications occur in 1-2% of cases after surgical treatment of hallux valgus.
Avascular necrosis. A medial capsulotomy may result in disruption of the blood supply to the first metatarsal head in a small percentage of cases.
Nonunion with metatarsalgia is more often observed after Lapidus and cross osteotomy with excessive shortening of the first ray of the foot and is associated with overload of the remaining metatarsal bones.
Hallux Varus is associated with overcorrection of hallux valgus, excessive lateral release, and lateral sesamoidectomy.
Hook-shaped deformity of the first finger - associated with damage to the flexor pollicis, more common after Keller surgery.
Metatarsalgia of the 2nd metatarsal bone - often accompanies hallux valgus, can manifest itself according to the principle of pain dominance; Weil osteotomy is used for treatment.
Numbness of the first limb, paresthesia, pain in the projection of the postoperative scar, neuromas can form in the area of the medial incision as a result of trauma to the medial branch of the dorsal cutaneous nerve.
Progression of arthrosis of the first metatarsophalangeal joint, decreased range of motion, and worsening pain may be a consequence of excessive trauma to the articular cartilage during surgery or the presence of concomitant metabolic pathology.
The article is intended to inform about the disease and treatment tactics. Self-medication poses a danger to your health.
Cost of surgery to remove hallux valgus
The doctor calculates the exact cost of the operation. It is very difficult to name a specific figure - it varies from twenty to eighty thousand rubles. This depends on the type of surgical intervention chosen by the attending physician (in accordance with the stage of the disease and physiological characteristics of the patient), the type of anesthesia, outpatient or inpatient stay, materials and instruments used. To keep the price low, come get rid of hallux valgus in a timely manner, on an outpatient basis, using minimally invasive intervention.
Symptoms
Symptoms of hallux valgus are mainly caused by bunions. Bunion is quite painful. With severe hallux valgus, a cosmetic problem also appears. Moreover, choosing shoes becomes difficult, especially for women who want to be fashionable and for them, wearing fashionable shoes becomes a real challenge. Finally, increasing deformity begins to move the second toe and may create conditions for the second toe to rub against the shoe.