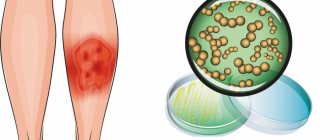
Erysipelas, or simply erysipelas, is an infectious-allergic disease that affects the skin and subcutaneous tissue. The disease is quite common and prone to relapse. It ranks fourth among all infectious diseases and is also becoming more common over time. Thus, over the past twenty years, the number of relapses of this disease has increased by 25%. Moreover, a severe form of the disease is becoming more common - now it is about 80% of cases, although 50-60 years ago only 30 percent of patients were diagnosed with a severe form.
Causes of erysipelas
Streptococcus can remain in the body for a long time in a “dormant” state, when its active reproduction is suppressed by the immune system. In this case, the disease will not develop. But simultaneous exposure to several unfavorable factors can lead to illness.
For an inflammatory process to occur, several circumstances must coincide:
- damage to the skin of any type: allergic, traumatic or burn;
- decreased immunity as a result of chronic diseases, fungal infections, vitamin deficiency or exhaustion of the body;
- infection of injured skin areas with beta-hemolytic streptococcus.
Body hygiene plays an important role - erysipelas occurs much more often in regions with poor sanitary and hygienic conditions.
There are observations that the disease is more typical for people of the white race.
How does infection occur?
The causative agent of this pathology is group A streptococcus. It mainly affects women over 50 years of age. With weakened immunity, hypothermia, stress, damage to the integrity of the dermal integument or chronic fatigue, the chance of developing erysipelas increases many times over.
Infection occurs through direct contact with an infected person or carrier, sometimes the introduction of streptococcus occurs through contact with infected blood.
The high-risk group includes people with the following diseases:
- Diabetes;
- Obesity;
- Mycoses;
- Chronic infections (otitis media, caries, tonsillitis);
- Varicose veins;
- Alcoholism.
Symptoms of erysipelas
The disease begins abruptly and is acute. Patients, as a rule, can even indicate the hour of its occurrence.
The onset is similar to a severe acute respiratory viral infection - the temperature rises quickly, and general intoxication of the body occurs. Chills (often shaking), headaches, nausea, vomiting, pain and aches in the back and joints are observed. In severe cases, convulsions and delirium may occur.
Skin lesions begin to develop 10-20 hours after the onset of general symptoms. It begins with itching of the skin, a feeling of tightness, and sweating. Then the skin at the site of infection begins to redden and swell, and severe erythema occurs.
A characteristic sign of erysipelas is very bright hyperemia (redness) of the affected area with clear, uneven boundaries, which are called “tongues of flame” or “geographic map.” The edges of the area are raised in the form of an infiltration ridge. The inflamed area is hot to the touch, swollen, thickened, and shiny. When pressing on it, slight pain occurs; after pressing, the redness under these areas disappears for a few seconds.
Lymphadenitis is also characteristic - hardening of the lymph nodes, decreased mobility and pain when pressed. In some patients, a pink stripe appears on the skin, which connects the inflamed area with the nearest group of lymph nodes.
Clinical symptoms
The duration of the incubation period for erysipelas ranges from 2-3 hours to 5 days. In case of relapses, exacerbation occurs against the background of stressful situations and general hypothermia. Most patients experience an acute onset of the disease.
At the initial stage of erysipelas, general signs of intoxication develop within 23-48 hours in 50% of patients. Clinical manifestations of the disease are presented:
- headache attacks;
- weakness, chills;
- muscle discomfort;
- nausea and vomiting – in 30% of patients;
- an increase in temperature from 38 to 40 degrees;
- the occurrence of unpleasant sensations, burning in the area of the future site of inflammation.
After the first signs of the development of the pathological process and until the middle phase of erysipelas, no more than 2 days pass. The febrile state and symptoms of intoxication of the body reach their peak, and local manifestations of the disease begin to form.
In most cases, erysipelas affects the lower extremities, less often it appears in the face and hands. Sometimes it can occur in the area of the torso, intimate area, and mammary glands.
Classification
Erysipelas is usually classified according to several parameters.
According to the frequency of occurrence of erysipelas, they are divided into 3 types:
- Primary – the first occurrence of the disease.
- Repeated – usually occurs after a certain period (a year or more).
- Recurrent - occurs periodically at indefinite intervals from several weeks to several years, with the same localization as the previous one, and is usually associated with immunodeficiency states of the body.
Particular attention should be paid to recurrent erysipelas and treatment should be directed not only to suppressing the infection, but also to the general strengthening of the body.
Classification by distribution on the body:
- Localized - has a clear focus of localization within the anatomical region of the body (face, legs, back).
- Widespread - manifested in several nearby areas of the body (for example, simultaneously on the thigh and lower leg).
- Migratory (creeping) - after healing in one part of the body, a relapse occurs in another.
- Metastatic - foci of localization are located on parts of the body remote from each other (for example, the face and lower leg).
Mixed forms may also occur. Particularly unpleasant is erysipelas of the facial skin. It causes not only physical, but also moral suffering due to the deterioration of the patient’s appearance.
According to the nature of manifestation on the skin:
- Erythematous - there is redness of the skin, itching, burning and swelling.
- Erythematous-bullous - to the previous symptoms is added the appearance of bubbles with a clear liquid, which then crack, and the disease progresses to the next form.
- Erythematous-hemorrhagic - spots of subcutaneous hemorrhage appear on the inflamed area, which cause more discomfort and require more time to heal.
- Erythematous - bullous-hemorrhagic is the most severe form, in which the skin area is affected as deeply as possible.
The last form of the disease poses the greatest danger to the patient.
According to the severity of the disease, it is divided into 3 forms:
- Mild - the temperature rises slightly, resembling a common cold, does not last long (1-3 days), and a small area of skin is affected, most often without deep structural changes (erythematous manifestation).
- Moderate severity - fever lasts more than 3 days, the temperature rises significantly, headaches, joint pain and other flu-like symptoms are possible, large areas of the skin are affected.
- Severe - fever is manifested by very high temperatures, lasts more than 5 days, large areas of the body are affected with hemorrhagic and bullous manifestations.
Negligence towards the mild stage and lack of adequate treatment leads to the progression of the disease and the occurrence of severe forms of the disease.
Therefore, if you suspect erysipelas, you should immediately consult a doctor.
Prevention
Since the disease can affect anyone, prevention of erysipelas is important both for those who have already had the disease once, and for those who have only heard about such a disease.
Prevention consists of following the following tips:
- Treat any inflammation on the skin or mucous membranes in a timely manner.
- Maintain personal hygiene. In the event that work or lifestyle is associated with additional pollution, hygiene should be even more thorough, but not excessive, so that the skin does not suffer - otherwise the effect will be the opposite.
- Use special products (gels and oils) for washing that do not dry out the skin. Regular soap is not suitable for regular use.
- Carefully monitor the condition of your skin in hot weather or if you have folds that constantly sweat. In this case, it is necessary to use special powders.
- Pay close attention to your health if you have problems with blood vessels or lymph stagnation. Such people are recommended for massages and various procedures that disperse fluids in the body.
- Treat your skin immediately if you have frostbite, chapping, or sunburn.
- Wear comfortable, breathable, natural clothing if possible that fits loosely on the body.
- Carefully monitor your immunity and eliminate all factors that can weaken it.
Remember that you cannot insure against this disease, but you can do everything to reduce the risks of its occurrence.
Which parts of the body are most often affected by erysipelas?
Let's look at which areas of the body the inflammatory process most often occurs:
- Legs in the shin area. Due to poor circulation or insufficient lymphatic drainage, stagnation occurs in this part of the body, and infection accumulates. Therefore, erysipelas of the leg is one of its most common types.
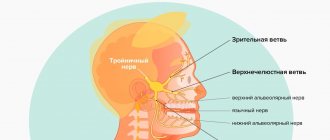
- Skin of the face and head. This localization is facilitated by congestion caused by ENT diseases.
- Torso. The risk of erysipelas increases in areas of excessive sweating and abrasions, as well as on the surface of scars.
- Hands. The most rare lesion, since it is the most mobile part of the human body, which prevents the occurrence of stagnation.
Consequences of the disease
The infectious disease is dangerous due to stagnation of lymph and blood in the extremities. Because of this, the nutrition of the inflamed tissues is disrupted. Hemorrhagic skin lesions are fraught with purulent complications:
- ulcers;
- phlegmon;
- an abscess.
In some patients, pneumonia and thrombophlebitis occur against the background of erysipelas. Increasing swelling of the extremities leads to elephantiasis. With severe lymphedema, eczematous rashes, papillomas, and hyperkeratosis form in the affected areas. After bullous-hemorrhagic erysipelas, persistent pigmentation remains on the body in places of ulceration.
Diagnostics
Since the symptoms of erysipelas are clearly manifested and specific, the doctor can make a diagnosis even during the initial examination based on the following symptoms:
- sudden manifestation of the disease in the form of a feverish state with signs of acute intoxication of the body;
- characteristic skin manifestations;
- enlarged lymph nodes;
- muffled heart sounds, rapid heartbeat;
- decrease in pressure.
Special laboratory diagnostics are not needed. But to confirm the diagnosis, you should pay attention to the following parameters of a general blood test:
- ESR, as in any acute inflammatory process, is more than 20 mm/hour;
- increased number of leukocytes;
- decreased number of red blood cells;
- decreased hemoglobin, especially with hemorrhagic manifestations.
It is also recommended to determine the strain of streptococcus in a laboratory to select the most effective treatment regimen.
Erysipelas of the skin - treatment
The main method of treatment for this disease is medication.
The following drugs are used:
- Antibacterial (antibiotics) are the main element of therapy. Accepted for about 2 weeks.
- Anti-inflammatory and antipyretic - necessary to reduce fever.
- Painkillers – used both locally and orally.
- Antihistamines - needed to relieve allergy-like reactions at the site of inflammation.
- Non-steroidal anti-inflammatory drugs - to reduce the intensity of inflammation and relieve pain.
- Ointments and creams directly in areas of severe skin damage.
- Antiseptic dressings - necessary for deep skin lesions;
- Steroid or immunomodulatory drugs are prescribed for severe disease.
Most often, several classes of drugs are prescribed at once, since a complete cure requires an integrated approach.
It takes up to 2 weeks to relieve the acute phase. But even after this you should not stop treatment.
The skin in areas that have been inflamed is very vulnerable in the next few weeks and may peel. In no case should the affected areas be exposed to intense sunlight for at least a month after the acute phase has ended. Additional moisturizing with special ointments and creams is also necessary to completely restore the skin structure.
After the acute phase has passed, physical therapy is recommended.
Physiotherapeutic methods:
- ultraviolet radiation - to inhibit the growth of streptococci;
- electrophoresis - for more effective administration of drugs;
- UHF – to improve lymph flow, blood circulation and local immunity.
Occasionally it is necessary to resort to surgical treatment. It becomes necessary for deep lesions of the skin.
Particular attention should be paid to recurrent erysipelas. Treatment of its acute phase does not differ from treatment for the primary disease. After acute symptoms are relieved, an additional course is required to restore immunity and get rid of streptococcal infection.
Treatment of uncomplicated forms of the disease is carried out on an outpatient basis, under the supervision of the attending physician. Severe cases may require hospitalization of the patient.
Self-medication can be deadly due to the potential for severe complications.
Treatment
If erysipelas develops on a leg, arm or other part of the body, the approach will always be comprehensive - local treatment alone is simply not enough. Moreover, the emphasis is largely on increasing immunity, otherwise the risks that the disease will recur are very high. Special medications are used to work with the immune system, but it is important for the patient to change their lifestyle: rest well, carefully monitor their health, eat right, and eliminate negative factors.
In the treatment of erysipelas, antibiotics are used, as well as antibacterial drugs from other groups. Drug therapy is selected individually - you should not prescribe medications yourself under any circumstances.
Along with taking medications, it is necessary to treat the affected skin: with special solutions, powders, aerosols. And the ointments that people love to prescribe for themselves - synthomycin, ichthyol, Vishnevsky - are strictly prohibited in this case, since they can provoke complications and cause the development of an abscess. The use of traditional medicine in any form is not allowed - in the treatment of erysipelas it is extremely dangerous!
Patients must have a preventive conversation regarding the nuances of hygiene during treatment. So, you need to change bed linen every day, take care of air access to the affected area, and regularly take a shower in warm, very comfortable water. Do not wipe the skin - only soak it with paper towels.
Physiotherapeutic methods are also used for erysipelas: ultraviolet irradiation, magnetic therapy, UHF, electrophoresis, certain types of laser therapy, applications with warm paraffin. At each stage of treatment, specific procedures are prescribed, and they are selected individually - for each patient and his condition. Any amateur activity is also inappropriate here, otherwise you can harm your health.
Very serious complications require surgical treatment.
If you encounter such a problem, we recommend immediately contacting the JSC Medicine clinic. We are located in Moscow and have a large staff of professional dermatologists, therapists and other specialists who can help you. And modern conditions for diagnosis and treatment will help achieve results much faster.
If doctors begin treatment in a timely manner and the patient follows all recommendations, the disease can be cured within 10-14 days.
Complications
Erysipelas is a treatable disease, but without adequate treatment and with concomitant diseases, it can lead to serious complications.
Typical types of complications with erysipelas:
- Necrosis is the death of the skin in the affected area. If the necrotic areas are extensive, surgery may be necessary.
- An abscess is a purulent inflammation. It occurs in the bullous form and manifests itself in the appearance of subcutaneous purulent foci. Their prompt removal is mandatory.
- Phlegmon is a large purulent focus. Also requires surgery.
- Purulent phlebitis is the formation of purulent foci around the vessels of the limb. As a result of pressure on the vessel, blood flow decreases, which leads to oxygen starvation of surrounding tissues. May cause extensive necrosis.
- Sepsis is the entry of a large number of streptococci into the bloodstream. Deadly condition.
- Damage to the heart muscle - occurs when streptococci enter the myocardium.
- Purulent meningitis - if the area of inflammation is located on the head and has entered the purulent stage, streptococci can enter the spinal cord and cause meningitis.
- Deterioration of vision - when erysipelas are localized in the eye area, due to edematous phenomena, the hydration and blood supply to the eyeball is disrupted. May lead to irreversible loss of visual acuity.
The following factors significantly increase the risk of complications:
- fungal infections;
- diabetes;
- lymphostasis;
- phlebeurysm;
- swelling of various origins;
- hypovitaminosis or exhaustion of the body;
- immunodeficiency;
- severe intoxication of the body.
If there is at least one of the risk factors, a more serious attitude to treatment and more careful monitoring by the attending physician is required.
At-risk groups
Most often, women over 50 years of age are affected by this disease, but it can also occur in infants. In their case, infection occurs after streptococcus enters the wound of the umbilical region. There is no explanation for this fact, but people with blood group III suffer from erysipelas more often. There is also a connection with the place of residence. In South Asia, as well as in Africa, this disease is very rare.
People with a low level of immunity, weakened by illness, stress, treatment and other factors are at risk.
Prevention of complications and relapses
The disease has clearly defined symptoms. If two or more symptoms are detected, you must immediately consult a doctor and begin treatment immediately. Strict adherence to recommendations and implementation of all necessary procedures will avoid complications.
It is important to complete treatment even after the acute manifestations of the disease have been eliminated. It is especially important not to stop the course of antibiotics before the prescribed time, as this leads to chronicity of the disease and the development of addiction to this type of antibacterial drugs - next time they may be useless to you.
To prevent a relapse, it is important to maintain good blood and lymph flow in areas of inflammation, and to monitor the cleanliness and dryness of the skin.