Chronic rhinosinusitis is a common disease in which a long-term inflammatory process of the nasal mucosa continues (12 weeks or more).
Author:
- Galkin Alexey Vladimirovich
ENT pathology expert
3.25 (Votes: 4)
Chronic rhinosinusitis is a common disease in which a long-term inflammatory process of the mucous membrane of the paranasal sinuses continues (12 weeks or more).
Differences between chronic and acute rhinosinusitis
Chronic rhinosinusitis is characterized by a long course and usually occurs without a pronounced increase in temperature. An acute condition is always accompanied by high fever, begins unexpectedly and has more pronounced painful symptoms.
The main symptoms of chronic rhinosinusitis:
- runny nose;
- impaired nasal breathing, feeling of swelling in the nose;
- postnasal drip (accumulation or drainage of mucus in the throat, the need to cough up mucus);
- swelling and swelling of the soft tissues of the cheeks, eyelids, nose, forehead;
- deterioration (absence) of smell and taste.
Also, with chronic inflammation, a cough may appear with radiating (radiating) pain in the ear, upper jaw, and teeth.
Other symptoms of chronic rhinosinusitis:
- otalgia (ear pain);
- pain spreading to the upper jaw and teeth;
- sore throat;
- cough (may get worse at night);
- halitosis (putrid odor);
- fatigue;
- nausea.
Clinical observation
Patient T., 18 years old. Complaints of difficulty in nasal breathing, congestion and purulent discharge from the nasal cavity. According to the patient, complaints appeared against the background of ARVI on the 6th day of illness. It is treated with vasoconstrictor drops and antipyretic drugs with a short-term positive effect. During endoscopy of the nasal cavity with a Karl Storz 0 g endoscope (Germany), inflamed and edematous mucosa, viscous mucopurulent discharge in moderate quantities, mainly in the area of the middle nasal passage on the right, were visualized, the nasal septum deviates to the right, in the nasopharynx and oropharynx, discharge of discharge into the oropharynx was noted with symptoms of pharyngitis.
It must be taken into account that endoscopic examination of the nasal cavity is carried out by an otolaryngologist. General practitioners and pediatricians should follow the diagnostic criteria for ARS.
The patient was prescribed complex topical therapy, which included rinsing the nasal cavity with a normalized solution of sea salt, Sinuforte, 1 injection 1 time per day into each half of the nose for 7 days. During the therapy, regression of symptoms and significant positive dynamics were noted when examined after 7 days (Fig. 2).
The patient's recovery occurred with monotherapy, without the use of antibacterial drugs.
Causes of chronic inflammation
The main reason for the development of chronic inflammation of the maxillary sinuses is a violation of their normal drainage. This occurs due to prolonged infectious or non-infectious edema (allergy, drug-induced edema) in the area of the maxillary nasal anastomosis or impaired mucociliary clearance. Also, the background for the formation of chronic inflammation is anatomical obstacles in the nose that disrupt normal drainage (deviated septum, enlargement of the middle turbinates).
In summary, the main causes of chronic sinusitis are:
- prolonged allergic swelling of the nasal mucosa;
- frequent respiratory infections;
- septal deformation;
- hypertrophy of the middle turbinates;
- prolonged swelling of a non-allergic nature (medicinal rhinitis);
- chronic inflammatory process in the area of the upper teeth (periodontitis, odontogenic cysts);
- foreign bodies (filling material, sinus lift material, tooth roots, etc.);
- neoplasms in the nasal cavity or paranasal sinuses;
- other diseases: cystic fibrosis, gastroesophageal reflux, HIV infection, immunodeficiency conditions.
Features of the development of the disease
Allergic rhinosinusitis provokes inflammatory processes in the nasal mucosa and paranasal sinuses. As a rule, the disease develops against the background of problems with the reactivity of the body, incl. with a weakened immune system.
As the inflammatory processes develop, they spread to nearby skin, larynx, bronchi, lungs, and mucous membrane of the eyes. Very rarely it is isolated.
Based on the duration of the pathological condition, rhinosinusitis can be classified as follows:
- Episodic acute. Usually the pathological condition passes quickly. The exception is those cases when the allergens are inhalations, wool, and feathers.
- Seasonal. An outbreak of the disease occurs when plants are flowering.
- Year-round or persistent. Lasts at least 9 months a year.
For reference! According to statistics, allergic rhinosinusopathy occurs in 20% of people around the world.
Complications of chronic rhinosinusitis
Prolonged inflammation carries many dangers, since the sinuses are close to such important structures as the eyes and brain:
- Meningitis (inflammation of the membranes of the brain and spinal cord);
- Sepsis. Generalized infection;
- Other infectious complications. Sometimes the inflammation spreads to the bones (osteomyelitis) or skin (cellulitis);
- Orbital complications. If the infection enters the eye socket, it can cause decreased vision or permanent blindness.
- Partial (or complete) loss of smell. The difficulty of odorants entering the olfactory cleft and inflammation of the olfactory nerve can lead to temporary or permanent loss of odor perception.
Diagnosis and recommended clinical studies
The diagnosis of rhinosinusitis is established on the basis of:
- Anamnestic data.
- Clinical manifestations.
- Laboratory test results.
- Results of instrumental examination methods.
Acute bacterial rhinosinusitis is characterized by a connection with an episode of acute respiratory viral infection suffered 5-10 days ago.
Patients with a history of odontogenic and fungal sinusitis often have previous complex fillings of the teeth of the upper jaw, as well as a long history of repeated visits to an otolaryngologist and repeated diagnostic punctures of the maxillary sinuses, during which no contents were obtained.
Polypous rhinosinusitis is characterized by gradual progression of the main symptoms: difficulty in nasal breathing and decreased sense of smell. Often patients are bothered by the painful sensation of constant flow of a very viscous secretion down the back wall of the nasopharynx. In many cases, polypous rhinosinusitis is combined with bronchial asthma, intolerance to non-steroidal anti-inflammatory drugs, and cystic fibrosis.
Diagnostics
To identify a chronic form of rhinosinusitis, the doctor will need to interview you, conduct a physical examination, and rhinoscopy (examination using a nasal speculum). But additional research will be required to determine treatment tactics.
Additional diagnostic methods:
- Endoscopy. A flexible, soft tube (endoscope) with fiberoptic light allows the doctor to see your nasal passages, the sinus area, and sometimes the inside of your sinuses.
- X-ray tomography. Images taken by a computed tomography (CT) scanner can show details of your maxillary sinuses and nasal area. The doctor will determine the volume and nature of the sinus lesions and assess the patency of sinus-nasal communications.
- Sowing from the mucous membrane for flora. Allows you to find out the infectious cause (if any) of sinus inflammation (fungi, bacteria) and prescribe the necessary treatment.
- Allergy testing. If your doctor suspects that the condition is caused by an allergy, you will need to undergo allergy testing (rhinocytogram, blood IgE, eosinophil cationic protein).
Establishing diagnosis
If you suspect rhinosinusitis, you should make an appointment with an otolaryngologist and an allergist or immunologist. After collecting a history of the disease, specialists will prescribe the following diagnostic methods:
- tests for allergic reactions;
- rhinoscopy;
- radiography.
The purpose of these research methods is to determine the characteristics of the washing fluid and study it for the presence of pus. In addition, during the diagnosis, the allergen-irritant is identified, the causes of the development of the disease are established (the origin may be bacterial or viral). Studies are also necessary to confirm or exclude vasomotor rhinitis.
Treatment of chronic rhinosinusitis
The goal of treatment is to reduce the number of exacerbations of sinusitis and reduce or disappear the symptoms of the disease. The main therapy is aimed at improving the drainage of the paranasal sinuses, as well as improving the functioning of the local immunity of the mucous membranes. To do this, it is necessary to eliminate the blockage of the sinus-nasal anastomosis, reduce the viscosity of the mucous secretion, and carry out immunotherapy. Sometimes surgery is required to clear the sinuses.
Drug therapy
The first stage of treatment for chronic rhinosinusitis is conservative therapy.
It includes:
- Regular cleansing of the nasal cavity and sinuses with isotonic sodium chloride solution (sterile saline solution).
- Nasal topical corticosteroids. These are nasal sprays that help reduce inflammation and swelling in the area of sinus anastomosis and improve drainage (mometasone, fluticasone, beclomethasone).
- Inhalation administration of a solution of antibiotics, corticosteroids, mucolytics into the sinuses. The use of sinus inhalers (Pari inhalers) allows medications to be administered precisely into the sinuses.
- Systemic administration of corticosteroids gives a strong anti-edematous, anti-inflammatory effect, reduces nasal polyps, improves drainage, but has serious side effects with long-term use of the drugs.
- Local and systemic use of antibacterial and antifungal agents. The use of antimicrobial agents for infectious chronic rhinosinusitis allows one to cope with exacerbation of the disease.
- Immunotherapy - Your allergist-immunologist may add immune-boosting or allergy-regulating medications to your sinusitis treatment.
Surgery
With low effectiveness of conservative therapy, surgical treatment of chronic rhinosinusitis is indicated. It is aimed at eliminating the mechanical obstacle to sinus drainage (enlarged turbinate, deformed nasal septum, anatomical narrowing of the sinus anastomosis area, polyp in the anastomosis area, etc.), as well as cleansing the sinuses of foreign inclusions (fungal bodies, tooth roots, filling material, material for sinus lifting), cysts, polyps.
Endoscopic sinus surgery
For this procedure, the doctor uses an optical system consisting of a thin tube with magnifying lenses and a camera that transfers the image to a screen. Good visualization of the operated area, the ability to change the viewing angle ensures delicate and safe removal of obstacles at the exit from the sinus, and also allows you to clear it of foreign inclusions.
The surgical treatment performed only creates conditions for improving drainage and cleaning, so it is necessary to continue postoperative treatment to achieve a lasting effect.
Rhinosinusitis or a common cold in children
Acute respiratory viral infections (ARVI) usually occur in a mild form and end with the recovery of patients on days 5–10 of the disease. However, in a number of cases, complications of ARVI are observed in the form of rhinosinusitis, acute otitis media, and adenoiditis.
Acute rhinosinusitis is a disease that is encountered in everyday practice not only by otolaryngologists, but by pediatricians, internists and general practitioners. Thus, according to statistics, 2 cases of rhinosinusitis per 100 thousand people are registered annually in children under 4 years of age, and 18 cases per 100 thousand people in adolescents 12–17 years old [1]. Currently, it is believed that almost any acute respiratory viral infection is, to one degree or another, accompanied by inflammation of the paranasal sinuses and rhinological symptoms. Signs of rhinosinusitis, according to studies using computed tomography, are detected in 95% of cases of acute respiratory viral infection. The Russian Society of Rhinologists recommends using the broader term “rhinosinusitis”, since inflammation in the paranasal sinuses is always accompanied by inflammatory changes in the nasal mucosa [2].
According to the classification of the European consensus document EPOS-2012 (European Position Paper on Rhinosinusitis and Nasal Polyposis - European Consensus on Rhinosinusitis and Nasal Polyps), acute rhinosinusitis (ARS) is divided into viral ARS (common cold), post-viral ARS and bacterial (ABRS).
The main causative agents of ARS are respiratory viruses (rhinoviruses, respiratory syncytial viruses, adenoviruses, coronaviruses). As a result of exposure to viruses, the epithelium of the nasal cavity and paranasal sinuses becomes loose, the cilia of the ciliated epithelium die, and swelling of the mucous membrane and inflammation develop. As a consequence, there is a violation of the aeration of the sinuses, stagnation of the secretion of the mucous glands, a change in pH, a metabolic disorder in the mucous membrane, a violation of mucociliary clearance and the accumulation of serous exudate in the lumen of the paranasal sinuses. Due to a decrease in the rate of beating of cilia and disruption of mucociliary transport, the time of contact of pathogenic bacteria with the mucous membrane increases, which contributes to bacterial infection [3, 4].
The common cold or acute rhinosinusitis in children is defined as the sudden onset of two or more symptoms, such as nasal congestion/difficulty in nasal breathing, and/or colorless/light-colored nasal discharge, and/or cough (during the day or night). The presence of symptoms lasts no more than 12 weeks, and asymptomatic intervals may be observed during which there are no symptoms if the disease is recurrent. When collecting anamnesis, it is important to clarify the presence of allergy symptoms (such as sneezing, watery discharge from the nose, itching and watery eyes). Acute rhinosinusitis may occur one or more times over a period of time. It usually manifests as episodes of illness within one year, but there may be complete resolution of symptoms between episodes of illness, which is a criterion for recurrent acute rhinosinusitis. ARS is diagnosed when the symptoms of the disease persist for less than 10 days, post-viral ARS - if there is an increase in symptoms of the disease after the 5th day or persistence of symptoms for more than 10 days, but with a total duration of less than 12 weeks. If the patient experiences an increase in the severity of rhinological symptoms after 5 days from the onset of the disease or symptoms persist for more than 10 days (with complete resolution within 12 weeks), but in the absence of justification for stating the bacterial etiology of acute rhinosinusitis, the EPOS authors recommend a diagnosis of “acute post-viral rhinosinusitis” [12].
Bacterial rhinosinusitis on average accounts for 5–7% of cases of all rhinosinusitis and is most often caused by the following pathogens: Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis (mainly in pediatric practice), Streptococcus pyogenes, Staphylococcus aureus (in young children), presented as a monoflora , and bacterial associations [5]. Signs of ABRS that require antibiotics are the diagnostic criteria for ABRS based on clinical data: symptoms do not stop or there is no positive dynamics within 10 days, or most of the symptoms present at the onset of the disease persist for more than 10 days; pronounced symptoms at the onset of the disease - high fever, the presence of purulent discharge from the nose, pain in the paranasal sinuses, a significant disturbance in the general condition, which bother for 3-4 days, there is a tendency to the development of purulent-septic orbital processes or intracranial complications; symptoms are completely or partially relieved within 3–4 days, but within 10 days from the onset of symptoms, a relapse is observed with the resumption of all symptoms [1, 2].
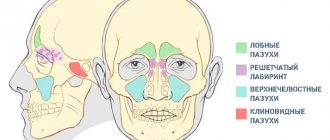
Any of the paranasal sinuses can be involved in the inflammatory process, but in first place in terms of frequency of damage is the maxillary (sinusitis), then the ethmoid (ethmoiditis), frontal (frontal sinusitis), and sphenoid (sphenoiditis). This sequence is typical for adults and children over 7 years of age. In children under 3 years of age, acute inflammation of the ethmoid sinuses predominates (up to 80–90%), and from 3 to 7 years of age, combined damage to the ethmoid and maxillary sinuses predominates [6].
The diagnosis of “acute rhinosinusitis” is usually made by a pediatrician or therapist at the initial visit based on a combination of clinical symptoms and objective examination data; later the patient can be referred to an otolaryngologist. General symptoms of ARVI and ARS include classic signs of inflammation of the nasal mucosa and, with the exception of pain, are limited to local manifestations (difficulty in nasal breathing, nasal discharge of mucous, less often mucopurulent in nature, impaired sense of smell). An important method is anterior rhinoscopy, which should be mastered not only by otolaryngologists, but also by general practitioners. During rhinoscopy against the background of diffuse congestive hyperemia and edema of the nasal mucosa, what is revealed? the presence of pathological discharge in the area of the outlet openings of the affected paranasal sinuses. A pathological secretion can also be detected on the back wall of the pharynx during pharyngoscopy.
Therapeutic measures for infectious MS include etiotropic, pathogenetic and symptomatic therapy. The main goals in the treatment of acute and relapsing MS are:
- pathogen eradication;
- reducing the duration of the disease;
- prevention of the development of orbital and intracranial complications.
Drug treatment, as a rule, consists of antibacterial drugs, “unloading” therapy with the prescription of vasoconstrictors, mucoactive agents, and anti-inflammatory therapy. Both systemic and local drugs are used.
Elimination therapy
One of the methods of treating ARS is irrigation procedures, in particular nasal douche, which involves rinsing and douching the nasal cavity. Rinsing the nasal cavity with saline solutions is carried out to eliminate viruses and bacteria. Preparations for rinsing the nasal cavity are usually prepared on the basis of sea water, sterilizing it and bringing the salt content to isotonic concentration. In case of acute respiratory syndrome, application of an isotonic solution to the mucous membrane helps to normalize the rheological properties of mucus and has a slight decongestive effect, improving nasal breathing, promotes the mechanical removal of pathological discharge and prepares the mucous membrane for the effects of topical drugs. Due to the absence of substances that can cause side effects, these drugs do not require precise dosing, and the frequency of their administration can vary widely according to need.
Antiviral and antibacterial therapy
The division of rhinosinusitis into viral and bacterial is directly related to approaches to therapy. Antiviral drugs are used for severe or moderate ARVI. The most effective are drugs whose leading mechanism of action is the stimulation of the formation of endogenous interferon, which in practice are used to treat most acute respiratory viral infections, regardless of the location of the inflammation. However, it must be taken into account that they are effective mainly in the first 48 hours from the onset of the disease.
The main controversial issue in the treatment of ARS is the prescription of antibacterial drugs. According to studies, more than 90% of general practitioners and otolaryngologists prescribe antibacterial drugs in the presence of symptoms of rhinosinusitis [19]. The widespread use of antibacterial drugs leads to an increase in antibiotic resistance. You should also remember about such often severe complications of antibiotic therapy as hepatotoxicity, allergic reactions, and dysbiosis. Recommendations for the treatment of rhinosinusitis EPOS outline a clear boundary for the use of systemic antibacterial therapy - only for ABRS! For mild ARS, symptomatic and etiopathogenetic drugs prescribed for ARVI are usually sufficient. Only if symptoms persist for 5 days or progress should one consider adding bacterial flora and prescribing systemic antibiotics. Moreover, due to certain difficulties in identifying the pathogen and the inability to wait for laboratory test results, the choice of antibiotics is most often empirical. The criteria for the effectiveness of empirical antibiotic therapy are the dynamics of the main symptoms of rhinosinusitis (headache, discharge, nasal congestion) and the general condition of the patient. Taking into account the spectrum of typical pathogens (Streptococcus pneumoniae and Haemophilus influenzae) and Russian data on their antibiotic resistance, the drug of first choice for acute rhinosinusitis is amoxicillin. However, more than 5% of Haemophilus influenzae strains in Russia are not sensitive to unprotected penicillins. Therefore, if there is no noticeable clinical effect after three days, amoxicillin should be replaced with an antibiotic active against penicillin-resistant pneumococci and β-lactamase-producing strains of Haemophilus influenzae: oral amoxicillin clavulanate, cephalosporins or macrolides (azithromycin and clarithromycin). In children and adolescents, the second-choice drugs prescribed if the first course of antibiotic therapy is ineffective are currently macrolides and clindamycin [2].
Antibacterial drugs for local action on the mucous membranes, if necessary, can be prescribed in combination with the systemic use of antibiotics, and in some cases as an alternative method of treating acute rhinosinusitis. But the issue of local antibiotic therapy for rhinosinusitis is controversial. The main contraindication is a violation of mucociliary clearance of the paranasal sinuses due to the adverse effect of large doses of antibiotic on the ciliated epithelium. There are special forms of antibiotics intended for endonasal administration in the form of a spray, which in the case of catarrhal rhinosinusitis can penetrate through the anastomosis of the paranasal sinuses and directly contact the pathogen at the site of inflammation. However, when filling the sinuses with mucous or mucopurulent exudate, you should first rinse the sinuses with saline solution or use decongestants [6].
"Unloading" therapy
Since the key link in the pathogenesis of acute rhinosinusitis is the blockade of the anastomosis of the paranasal sinuses due to swelling of the mucous membrane, one of the main directions of symptomatic and pathogenetic therapy is the restoration of the patency of these anastomoses - “unloading therapy” [6]. For this purpose, vasoconstrictors (decongestants) and mucolytic (secretolytic) agents are used.
Decongestants (oxymetazoline, xylometazoline, tetrizoline, phenylephrine, etc.), activating adrenergic receptors, cause vasospasm of the nasal mucosa, reducing its hyperemia and swelling, dilating the nasal passages and improving nasal breathing. Due to their rapid relief of nasal breathing, they are widely used to relieve symptoms such as rhinorrhea and nasal congestion and are very popular among patients. With strict adherence to the recommended dosage regimen, methods of application and duration of the course, side effects and adverse events when using topical vasoconstrictor drugs are rare. However, violations of the recommended dosage regimen (increasing single doses or frequency of use) can lead to an overdose with the development of serious pathological conditions. With prolonged and uncontrolled use of local decongestants, atrophy of the nasal mucosa may develop [5]. There is probably no doctor who does not remember that these drugs, when used for a long time, cause the development of “rebound” syndrome. However, unfortunately, patients or parents of patients do not always remember this. It should be noted that in children, especially young children, despite the local method of application, the use of decongestants may be accompanied by the development of systemic undesirable effects. An increased entry of local decongestants into the systemic circulation is also facilitated by trauma to the mucous membrane, which often occurs due to defects in the toileting of the nasal passages. Therefore, the use of topical decongestants should be limited. From the point of view of symptomatic therapy, the use of local drugs is more indicated, but from the point of view of the influence on pathogenesis, the use of systemic decongestants is indicated, since topical drugs cannot affect the swelling of the sinus mucosa. In this case, if possible, it is necessary to limit the use of decongestants to a short period (3-4 days) in minimal doses, since they can impair mucociliary transport.
Mucolytic therapy
The use of mucolytics refers to pathogenetic therapy. As already noted, an imbalance between the production of secretions in goblet cells and serous-mucosal glands and the evacuation of secretions by ciliated epithelial cells is one of the most important links in the pathogenesis of rhinosinusitis. Therefore, diluting viscous, thick secretions is important in the treatment of ARS. Taking medications with a differentiated effect on secretion production, reducing the viscosity of mucus and the function of cilia can restore impaired mucociliary transport. Mucolytic drugs change the physicochemical properties of the secretion by reducing its viscosity [6]. The international recommendations EPOS-2012 do not include mucolytic therapy, presumably due to the lack of a reliable method of experimental confirmation of their effectiveness. However, the use of mucolytics in acute rhinosinusitis is justified from a physiological point of view and is confirmed by long-term observations indicating the beneficial effect of mucolytic drugs on the course of acute rhinosinusitis, therefore mucolytic therapy, namely acetylcysteine and carbocysteine, are included in domestic standards of therapy and clinical recommendations [2, 6–9 ].
In the practice of a local doctor, a group of mucoactive drugs is most often routinely used for diseases of the lower respiratory tract. Of course, one should not extrapolate to the upper respiratory tract the effect of all mucolytics (ambroxol, bromhexine, etc.), widely used for bronchial pathology. Of the mucolytic agents in the treatment of rhinosinusitis, due to their mechanism of action and the presence of application points in the upper respiratory tract, only cysteine derivatives (acetylcysteine, carbocysteine) are used. Acetylcysteine is able to break disulfide bridges in acidic mucopolysaccharides and thus reduce the viscosity of mucus, the mucus loses its ability to be viscous and is gently removed by blowing the nose and sneezing, resulting in the restoration of normal drainage and aeration of the paranasal sinuses.
It should be noted that in addition to the direct mucolytic effect, acetylcysteine also has antioxidant and anti-inflammatory effects, which is extremely important in the treatment of rhinosinusitis. The effect on antioxidant systems helps protect cells from free radical damage, which leads to a decrease in inflammation on the mucous membranes of the respiratory tract and an improvement in clinical symptoms [10].
There is another important point: acetylcysteine reduces the adhesion of pathogenic bacteria to the epithelial cells of the mucous membrane of the respiratory tract and therefore reduces the colonization of the respiratory tract by pathogenic microbes [11, 12]. As discussed above, the prescription of antibiotics for viral ARS is not indicated. All the more valuable is the fact that the use of acetylcysteine reduces the likelihood of bacterial colonization and thereby reduces the likelihood of bacterial complications of rhinosinusitis. In addition, acetylcysteine leads to a decrease in the formation of biofilms by gram-positive and gram-negative bacteria and fungi; reduces the production of extracellular polysaccharide matrix, which contributes to the destruction of mature biofilms [13–15]. It is likely that acetylcysteine can destroy the disulfide bonds of bacterial enzymes, affecting the main component of the biofilm matrix (exopolysaccharides) involved in their formation or excretion. And due to its antioxidant properties and influence on the metabolism of bacterial cells, acetylcysteine can disrupt the functioning of bacterial adhesive proteins [16], which is confirmed by the culture method and electron microscopy [17]. Thus, the use of acetylcysteine in acute rhinosinusitis helps prevent the development of bacterial complications and chronicity of the process. It should be noted that, according to in vitro studies published in 2021, acetylcysteine is not an antagonist for most antibiotics used to treat respiratory infections [18], which means it can safely be prescribed simultaneously with antibiotics in the case of bacterial rhinosinusitis.
There are forms for using acetylcysteine both internally and topically. However, if there are symptoms of rhinosinusitis accompanied by a cough, with simultaneous damage to the upper and lower respiratory tract, it would be advisable to prescribe acetylcysteine orally, since in this case it simultaneously thins both viscous bronchial and nasal secretions, and in addition, has a systemic antioxidant and anti-inflammatory effect. action.
Anti-inflammatory therapy
In the EPOS-2012 recommendations, the main direction in the treatment of rhinosinusitis is topical endonasal corticosteroid therapy. Topical corticosteroids (mometasone furoate, fluticasone dipropionate, budesonide) have relatively recently entered the main arsenal of drugs for the treatment of ARS. Due to the pronounced anti-inflammatory effect of these drugs, which reduces swelling, the prescription of any other unloading therapy is considered unnecessary abroad. In Russian standards in the treatment of rhinosinusitis, unloading therapy retains its rather significant share, although in recent years it has been used more and more widely [6]. Glucocorticosteroids primarily suppress the development of edema by influencing the inflammation of the lamina propria of the mucous membrane. The functional ability of the anastomosis is restored - a key link in the pathogenesis of sinusitis and rhinosinusitis. In addition, corticosteroids actively suppress the release of fluid from the vascular bed and the production of mucus, which is an important factor in the pathogenetic therapy of acute rhinosinusitis. It must be remembered that the use of topical glucocorticosteroids is not indicated for children under 12 years of age.
The drugs of choice from the group of antipyretic and anti-inflammatory drugs are paracetamol and ibuprofen and their combinations at the height of acute manifestations of ARVI [6].
In conclusion, I would like to note that children with acute rhinosinusitis first of all go to pediatricians, and only then, if necessary, to an otolaryngologist. Since acute rhinosinusitis in the practice of a local doctor most often occurs not as an independent disease, but as part of an acute respiratory viral infection, the doctor is faced with the need to eliminate several symptoms at once. It is quite understandable that the doctor wants to influence all stages of etiopathogenesis at once, but most often this leads to the prescription of 4–5, and often more, drugs. At the same time, it is worth remembering that polypharmacy leads not only to higher treatment costs, but to an increased drug burden on the body, which is often accompanied by drug-drug interactions and the development of adverse drug reactions. In this regard, preference should be given to well-studied drugs with a complex effect, which makes it possible to simultaneously influence the main links of pathogenesis or several symptoms at once.
Literature
- Fokkens W., Lund V., Mullol J. et al. European position paper on rhinosinusitis and nasal polyps 2012 (EP3 OS) // Rhinology. 2012. Vol. 50 (23). P. 1–299.
- Lopatin A. S., Svistushkin A. M. Acute rhinosinusitis: etiology, pathogenesis, diagnosis and principles of treatment. Clinical recommendations. M., 2009. 25 p.
- Lopatin A. S. Rhinitis. M.: Litterra, 2010. P. 122, 126–127.
- Ryazantsev S.V., Kocherovets V.I. Etiopathogenetic therapy of diseases of the upper respiratory tract and ear. Guidelines. St. Petersburg, 2008. 120 p.
- Karpova E. P., Vagina E. E. The role of nasal decongestants in the complex treatment of acute rhinosinusitis in children // Medical Council. 2013, no. 1, p. 46–48.
- Abdulkerimov Kh. T., Garashchenko T. I., Koshel V. I., Ryazantsev S. V., Svistushkin V. M. Principles of etiopathogenetic therapy of acute sinusitis: methodological recommendations / Ed. S. V. Ryazantseva. St. Petersburg: Polyforum Group, 2014. 40 p.
- Order of the Ministry of Health of Russia dated December 20, 2012 N 1201n “On approval of the standard of primary health care for acute sinusitis” (registered with the Ministry of Justice of Russia on March 15, 2013 N 27696).
- Order of the Ministry of Health of Russia dated November 9, 2012 N798n “On approval of the standard of specialized medical care for children with acute respiratory diseases of moderate severity” (registered with the Ministry of Justice of Russia on March 12, 2013 N 27623).
- Order of the Ministry of Health of Russia dated December 24, 2012 N1395n “On approval of the standard of primary health care for chronic sinusitis” (registered with the Ministry of Justice of Russia on February 26, 2013 N 27331).
- Geppe N. A., Snegotskaya M. N., Penkina M. V. Algorithm for the treatment of cough in children // Farmateka. 2014. No. 1. P. 71–75.
- Singh M., Singh M. Heated, humidified air for the common cold. Cochrane Database of Systematic Reviews 2013, Issue 6. Art. No.: CD001728. DOI: 10.1002/14651858. CD001728.pub5.
- Smith SM, Schroeder K., Fahey T. Over-the-counter (OTC) medications for acute cough in children and adults in community settings // Cochrane Database Syst Rev. 2014, Nov 24; 11: CD001831. DOI: 10.1002/14651858. CD001831.pub5.
- Riise G., Qvarfordt I., Larsson S. et al. Inhibitory effect of N-acetylcysteine on adherence of Streptococcus pneumoniae and Haemophilus influenzae to human oropharyngeal epithelial cells in vitro // Respiration. 2000; 67:552–558.
- Aslam S., Darouiche R. Role of antibiofilm-antimicrobial agents in controlling device-related infections // Int. J. Artif. Organs. 2011; 34(9):752–758.
- Rubin B. Mucolytics, expectorants, and mucokinetic medications // Respir. Care. 2007; 52:859–865.
- Schwandt L., Weissenbruch R., Stokroos I. et al. Prevention of biofilm formation by dairy products and N-acetylcysteine on voice prostheses in an artificial throat // Acta Otolaryngol. 2004; 124:726–731.
- Zhao T., Liu Y. N-Acetylcysteine inhibit biofilms produced by Pseudomonas aeruginosa // BMC Microbiol. 2010; 10:140.
- Landini G. et al. Effect of N-acetylcysteine on the activity of antibiotics against relevant respiratory pathogens, ERS Congress, 2016.
- Little DR, Mann BL, Godbout CJ How family Phisitians distinguish acute sinusitis from upperrespirator tract infrctions: a retrospective analysis // J Am Board Fam Pract. 2000. Vol. 13. R. 101–106.
RU1611561073
E. P. Karpova, Doctor of Medical Sciences, Professor
Federal State Budgetary Educational Institution of Further Professional Education RMAPO Ministry of Health of the Russian Federation, Moscow
Contact Information
Prevention
Follow these steps to reduce your risk of chronic rhinosinusitis:
- avoid upper respiratory tract infections;
- reduce contact with people suffering from respiratory diseases (colds, ARVI);
- if cold symptoms persist (7 days or more), do not delay going to the doctor;
- manage your allergies. Work with your doctor to keep your symptoms under control;
- avoid tobacco smoke and polluted air, replace filters in your car on time, and clean the air conditioner in a timely manner;
- humidify the air in the house at low humidity;
- avoid hypothermia.
Pathogenesis of development
The main reason for the development of the pathological condition is considered to be a hereditary predisposition to it. The disease also manifests itself under the influence of the following factors:
- a high level of immune reactivity to the allergen that provoked rhinosinusopathy;
- allergies to medications;
- IgE-dependent allergic reaction;
- food allergies;
- bronchial asthma in close relatives;
- allergies to plants;
- penetration of pathogenic microorganisms into the nasopharynx;
- allergies to household chemicals and chemicals;
- frequent contact with paints and varnishes;
- allergy to dust;
- enlarged adenoids.
Any allergy, even in mild form, can develop into rhinosinusitis. This occurs under the influence of any irritant.
Types of sinusitis
There are several types of sinusitis:
- sinusitis;
- frontal sinusitis;
- ethmoiditis;
- sphenoiditis, but the latter type of sinusitis is extremely rare and almost always together with ethmoiditis.
1 Examination of the nasal cavity in MedicCity
2 Examination of the nasal cavity in MedicCity
3 ENT unit Atmos S 31
Exacerbations without treatment
A person suffering from vasomotor rhinitis increases the likelihood of developing rhinosinusitis. The mucous membrane swells greatly, which leads to periodic repetition of the inflammatory process. When the disease is not combated, the infection will quickly spread throughout the body, leading to:
- otitis;
- acute bronchitis;
- pneumonia;
- meningitis;
- tonsillitis;
- sore throat;
- subdural or epidural brain abscess;
- blood poisoning;
- optic neuritis;
- conjunctivitis;
- the appearance of blood clots in the blood vessels of the head.
Summary for parents
A child’s runny nose does not always indicate a common cold, which parents can easily cope with with basic therapeutic measures. It may be a manifestation of inflammation of the paranasal cavities.
It is impossible to make a correct diagnosis on your own, much less cure sinusitis. Attempts at self-medication can result in serious complications. Traditional medicine methods and recipes will not help without drug treatment.
At the slightest suspicion of sinusitis, you should consult a doctor and strictly follow all his instructions. Only in this way can you count on a cure and prevent sinusitis from becoming chronic.
Diagnosis of sinusitis using modern techniques
To confirm the diagnosis of sinusitis, the following types of examination are used:
- Video endoscopy of the nasal cavity and nasopharynx to identify features of the anatomical structure and determine predisposing factors for the development of sinusitis;
- radiography of the paranasal sinuses;
- Ultrasound examination of the paranasal sinuses is a safe method with no contraindications, used to diagnose sinusitis and monitor the treatment process;
- CT, MRI - according to indications;
- laboratory diagnostics according to indications in full.