What do deviations from the norm indicate?
Quite often it is necessary to take a test such as blood biochemistry, so for many it is important to decipher the data obtained and normal indicators for comparison with those obtained in the laboratory. At the same time, the presence of any deviations does not indicate the fact of certain health problems, so it is worth finding out all the nuances from the doctor. The numbers are considered in aggregate and separately; they can only indirectly indicate the presence of possible diseases or deviations from the ideal state. We suggest studying normal blood biochemistry indicators, the reasons for underestimated or excessively high data in women or men.
Interpretation:
- Renal dysfunction, decreased renal perfusion, congestive heart failure. Depletion of salts and water due to vomiting, diarrhea, increased diuresis or sweating. Shock in combination with increased protein catabolism (gastrointestinal bleeding, acute myocardial infarction, stress, burns). Acute or chronic interstitial kidney disease. Obstruction of the urinary tract. High protein diet.
- A diet low in protein and high in carbohydrates. Increased utilization of protein for synthesis (in late pregnancy, in children under 1 year of age, with acromegaly). Parenteral nutrition. Severe liver diseases. Drug poisoning. Malabsorption (celiac disease).
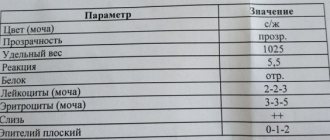
Sample result (PDF)
Data on nitrogen metabolic processes
A too slow metabolic process, fasting, polyuria or liver failure will be indicated by an underestimation of creatinine, urea, and uric acid in the blood. Normal blood biochemistry values increase the likelihood of problems with the diseases in question.
An overestimation of urea is also possible. If it is found during blood biochemistry, then arterial hypertension, poisoning or kidney disease will be suspected. Readings above normal for uric acid are a sign of poisoning, infectious diseases, skin pathologies, gout, leukemia or diabetes. One of the signs of abnormalities in kidney function is also high creatinine. The indicator also signals diabetes mellitus, muscular dystrophy or obstruction in the intestinal area.
Reduced blood urea levels
A decrease in urea levels is associated with liver diseases, when hepatocytes are affected and the energy for the synthesis of nitrogenous metabolites is reduced. These are, first of all, cirrhosis, hepatitis of various etiologies, occurring with liver failure. Also, urea may be slightly reduced due to hormonal changes (acromegaly, diabetes insipidus), impaired absorption processes in the intestine, and rare hereditary genetic pathologies (hyperammonemia).
A physiological decrease in urea includes flooding of the body, since the volume of circulating blood increases, and not the concentration of the metabolite itself. Ascorbic acid and anabolic agents can slightly reduce urea.
In children and pregnant women, urea levels may be reduced. Protein is actively synthesized, but is also quickly consumed as a building material during growth.
Amino acids and proteins
Protein often decreases during fasting or when following diets, but it can indicate a number of pathologies: chronic bleeding, problems with metabolic processes, anemia. Underestimated data is the norm during breastfeeding, during pregnancy (late pregnancy), for bedridden patients or in case of significant physical exertion.
The interpretation of the tests taken during blood biochemistry is considered carefully and normal values should not be exceeded. The protein is present in excessive amounts in individuals with autoimmune diseases, during infections, in cases of significant kidney pathologies or in the presence of malignant tumors.
Reduced levels of amino acids are a bad indicator, observed when there are problems in metabolic processes, often resulting in kidney or liver problems.
general characteristics
Blood urea nitrogen is considered to be the nitrogen contained in the end products of protein metabolism, and in particular in urea (one urea molecule contains 2 nitrogen molecules). Urea is formed in the liver from ammonia during its neutralization and is excreted through the kidneys, making up 40-50% of the non-protein nitrogen in the blood. Urea nitrogen in the blood reflects the state of protein metabolism (excretory function of the kidneys). An increase in blood levels indicates impaired renal function, and is therefore used to assess their function. Urea nitrogen also allows you to determine liver function, active inflammatory process, rheumatic process, as well as a violation of water-salt metabolism and an imbalance of microelements. Biochemical analysis helps to make a diagnosis, prescribe and adjust treatment.
Peptides in blood tests
One of the convenient options for checking blood biochemistry for normal values is the corresponding table. If the C-peptide is higher, then there is a suspicion of excessive insulin synthesis, the development of tumor formation or pancreatitis. A decrease compared to the standard may occur, this is possible during inflammation or diabetes (only the first type).
Content of glucose and carbohydrate metabolism metabolites
In diabetes mellitus, glucose increases, other reasons: problems with the central nervous system, pituitary gland, thyroid gland, brain injuries. If normal blood biochemistry levels for glucose in adults are underestimated, it is worth checking the endocrine system, liver and pancreas.
Increased blood urea
An increase in urea in the blood is called hyperazotemia or uremia.
When the glomeruli and tubules of the kidneys, that is, the renal filter, are damaged, the pressure in the renal vessels sharply decreases, the processes of filtration and excretion of metabolic products are disrupted. This leads to an increase in urea in the blood serum in acute or chronic pyelonephritis, glomerulonephritis, amyloidosis with renal failure of varying severity. Diabetes mellitus often occurs with kidney damage, which leads to impaired excretory function. The concentration of urea increases with dehydration, congestive heart failure, shock, and bleeding. An increase is also observed with increased protein breakdown during burns and cancer, fevers, and heavy power loads.
Data on microelements and vitamins
Often, normal blood biochemistry levels are checked when clarifying vitamin levels in men or women. Attention should be paid to sodium and potassium. If there is too much sodium, you may experience muscle cramps, irritability and excessive thirst. A minimal amount of the element leads to headaches, the desire to constantly sleep, vomiting, and coma.
If potassium is elevated, arrhythmia, underestimation of blood pressure, and confusion are possible. Vomiting and nausea are signs of low potassium, and sometimes the condition leads to involuntary bowel movements or urination.
In what cases is research usually prescribed?
Analysis for urea and creatinine is included in the basic biochemical screening and is required if kidney pathology is suspected.
It is also advisable to examine the level of urea and creatinine in the blood under the following conditions indicating possible kidney pathology:
- Fatigue, lack of concentration, poor appetite or sleep disturbances;
- swelling of the face, wrists, or ankles;
- Decreased urine output (oliguria);
- Pain in the lower back, side, under the ribs, near the location of the kidneys;
- High blood pressure.
Biochemical blood test: normal indicators
| Analysis: | Men: | Women: |
| Total protein | 64-84 g/l. | 64-84 g/l. |
| Hemoglobin | 130-160 g/l | 120-150 g/l. |
| Haptoglobin | 150-2000 mg/l | 150-2000 mg/l |
| Glucose | 3.30-5.50 mmol/l. | 3.30-5.50 mmol/l. |
| Urea | 2.5-8.3 mmol/l. | 2.5-8.3 mmol/l. |
| Creatinine | 62-115 µmol/l | 53-97 µmol/l. |
| Cholesterol | 3.5-6.5 mmol/l. | 3.5-6.5 mmol/l. |
| Bilirubin | 5-20 µmol/l. | 5-20 µmol/l. |
| AlAT (ALT) | up to 45 units/l. | up to 31 units/l. |
| ASAT (AST) | up to 45 units/l. | up to 31 units/l. |
| Lipase | 0-190 units/l. | 0-190 units/l. |
| Alpha amylase | 28-100 units/l. | 28-100 units/l. |
| Pancreatic amylase | 0-50 units/l. | 0-50 units/l. |
Blood urea measurement
All over the world, essentially the same method of measuring urea levels in the blood is used, but the result can be expressed in two completely different ways.
In the United States and some other countries, blood urea concentration is expressed as the amount of urea nitrogen. This test is called blood urea nitrogen (BUN), and the unit of measurement is milligrams per deciliter (mg/dL).
In all other parts of the world, urea is expressed as the whole molecule (not just the nitrogen part of the molecule) in the international SI units of millimoles per liter (mmol/L).
Since urea nitrogen only reflects the nitrogen content of urea (molecular weight 28) and the urea measurement reflects the entire molecule (molecular weight 60), then urea is approximately 2 times larger than urea nitrogen (60/28 = 2.14). Thus, 10 mg/dL urea nitrogen is equivalent to 21.4 mg/dL urea.
To convert urea nitrogen (mg/dL) to urea (mmol/l), the urea nitrogen value must be multiplied by 10 to convert deciliters to liters, and divided by 28 to convert milligrams to millimoles, that is, 10/28 = 0.357 . Therefore, the conversion factor is 0.357.
Blood urea nitrogen (BUN) in mg/dL * 0.357 = urea in mmol/L.
Urea (mmol/L) / 0.357 = urea nitrogen (mg/dL).
Wait. Add the book to the cart.
“There are plenty of races in the world - the whole color palette,
Each of us inhales two and a half liters at a time.”
Vysotsky
The nitrogen cycle in nature involves the conversion of the gaseous state by nitrogen-fixing bacteria into ammonia and nitrifying bacteria into nitric oxide, with the subsequent formation of amino acids in plant proteins. When animals eat plant proteins, the latter provide us with food and energy. In the human body, a product of protein breakdown, ammonia, is a highly toxic, but very scarce compound. Both the neutralization of ammonia and its use for the synthesis of nucleic acids (pyrimidine nucleotides) begin with the well-known reaction: NH3 + CO2+ 2 ATP = carbamyl phosphate (NH2 - CO - O - P) under the influence of the enzyme carbamyl phosphate synthetase. This starting reaction for both UREA SYNTHESIS and PYRIMIDINE NUCLEOTIDE SYNTHESIS occurs with the participation of two ATP molecules, which makes this biochemical reaction absolutely irreversible (!). This emphasizes the value of NITROGEN for the body.
The complementary purine-pyrimidine pair uses three ammonia molecules. The number of such pairs in the human genome is in the billions, and the importance of nitrogen in the formation of the entire pool of nucleic acids is certainly a priority. The irreversibility of the above reaction not only protects us from the possible toxic effects of ammonia, but also preserves for us a complete fund of nucleic acids.
Carbamyl phosphate enters the Krebs cycle 2 (not to be confused with the tricarboxylic acid cycle) for the synthesis of urea. Krebs cycle 2 is also called the arginine-succinate shunt, which emphasizes the relationship between protein and energy metabolism.
Urea, as a normal component of biological media, is needed for “resuscitation”, i.e. restoration of the properties of slightly damaged proteins when their biological properties deteriorate, primarily SOLUBILITY. Along with total protein and albumin, urea is a constant benchmark for the health of protein metabolism and the level of urea strictly follows the level of total protein. Therefore, a decrease in total blood protein below 75 g/l should automatically lead to a decrease in blood urea levels below 5 mmol/l. It becomes clear why, when the total protein level is below 60-65 g/l, the urea level does not exceed 4-4.5 mmol/l. This is the level of adaptive biochemical patterns. In the model of endogenous protein burning (chronic alcoholism) and in severe resuscitation situations, there are cases with a COMPLETE ABSENCE of urea in the blood. This is a deep catastrophe at the genomic level, in which cells, as unnecessary, “throw away” the nucleoli on which ribosomal nucleic acid (rRNA) is synthesized, because the processes of synthesis of proteins and nucleic acids in the body stop. This is one extreme of urea metabolism in the body.
When overeating meat, it is difficult to achieve a state of “nitrogen poisoning”. To do this, you need to eat at least a kilogram of meat every day (400 grams of protein is the limit) per day. With such “abuse” of meat, the urea level can increase to 8-10 mmol/l (exogenous azotemic syndrome). The optimal intake of proteins, fats and carbohydrates in food hygiene is determined by the ratio 1:1:4. This is the other extreme of urea metabolism in the body.
In infectious practice, hypoproteinemia often develops in a short time (3-7 days) and is accompanied by a synchronous drop in the level of urea in the blood below 5 mmol/l. Doctors need to monitor this indicator not only in the infectious diseases clinic, but also in real life: it characterizes the “sufficiency of the protein pool” and the efficiency of the biochemical circulation of the body’s proteins (there are more than a hundred types of them in one blood!). There are seven pools of amino acids in the body for all occasions in the categories of “urgent” and “delayed” consumption.
In practice, doctors do not pay attention to low urea levels. Their attention is drawn only to an increase in the level of urea in the blood as an early sign of kidney failure. In such situations, the synchronicity of the dynamics of urea and creatinine is very important. When urea increases, creatinine levels also increase and vice versa. In real life and practice, on the contrary, the situation of “urea-creatinine dissociation” is often encountered. When urea increases and the level of creatinine decreases, one should first look for the cause not in the kidneys, but in the intensification of protein breakdown processes (increased thermogenesis, feverish-intoxication syndrome, hepatic decompensation).
Another important factor that doctors don’t even think about is why urea is measured in mmol/L, and CREATININE in μMOL/L, i.e. the difference in values differs by a THOUSAND. This is explained by the physiological role of creatinine in the blood not as a product of protein breakdown, but as a deficient biologically active compound of a hormone-like type. Hence the minimal amounts of creatinine levels in the blood and another reason for “urea-creatinine dissociation” in the practice of infectious febrile conditions. For both urea and creatinine, there is an age-related physiological type of dynamics. The values fluctuate: 80, 70, 60, 50 µmol/l. Creatinine reaches its ideal value of 80 µmol/l only at the time of puberty. Prior to this, it belongs to the category of deficient metabolites and is in demand in energy processes - the extraction of ATP from mitochondria. The energy currency in the cell is creatine phosphate.
We would like to draw the attention of doctors. Do not look only for renal failure in every patient (especially when there is no organ predisposition to this)! Try to appreciate protein and urea as the interconnected life potential of protein wellness. In a state of health, the body strives to maintain protein levels in the range of 75-85 g/l, and urea levels at least 5 mmol/l. When urea decreases below 4 mmol/l, think about what could cause this condition: protein starvation (vegetarianism)?, lifestyle (alcoholism)?, chronic febrile conditions: previous acute infectious diseases with a temperature of 39 ° C, tuberculosis, oncological processes. Urea is one of the most important adaptation parameters of any organism.