General microscopic analysis
{banner_banstat0}
Examination of sputum under a microscope is carried out to differentiate diseases of an allergic and infectious nature. The analysis begins with an assessment of the appearance, quantity, presence of inclusions (blood, pus), smell and color. Next, the preparation is prepared for further examination using a microscope. Only after microscopy of a smear can conclusions be drawn about a particular disease. Most often you can see in sputum:
- unchanged red blood cells;
- leukocytes and its types (eosinophils, lymphocytes);
- epithelial cells of the bronchi and trachea;
- atypical cells;
- various fibers;
- mushroom mycelium;
- bacterial agents.
Microscopic analysis of sputum is a qualitative method for diagnosing diseases of the pulmonary system. But the result largely depends on the professionalism of the laboratory assistant and his skills.
What does it show?
{banner_banstat1}
Studying the qualitative composition of pulmonary discharge is the main reason why a sputum test is taken for examination through a microscope. Seeing the laboratory technician’s conclusion, the doctor can correlate these data with the clinic and accurately make a diagnosis. For each disease there are diagnostic criteria, including laboratory ones. Microscopic examination helps to more accurately determine the stage of the process, which facilitates the selection of the correct treatment regimen.
For microscopic examination, the sample is stained or viewed in an unstained state. The sputum is placed on a glass slide, covered with a coverslip and a finished preparation is formed. Smear microscopy shows specific formed elements or inflammatory agents, sometimes particles of the pathogen, which makes it possible to clarify the diagnosis.
For bronchitis
Bronchitis in adults has a mixed origin and can be caused by both viruses and bacteria. Hence the characteristics of sputum are different. Often the disease is caused by mixed flora, so the sputum is a mucopurulent, copious discharge. Under a microscope, an increased number of leukocytes, columnar and squamous epithelial cells are revealed.
For the purpose of diagnosis of bronchitis, sputum analysis is rarely used, but it helps to differentiate the erased forms of pneumonia or asthma in the initial stages.
For bronchial asthma
{banner_banstat2}
Bronchial asthma produces pronounced changes in sputum that are unique to it. Here the doctor will find a large number of leukocytes and eosinophils, as indicators of allergic inflammation.
In addition to them, Leiden-Charcot crystals and spirals are always present in the smear. These are specific breakdown products of inflammatory cells, formed only during muscle spasms.
The sputum itself is expectorated in a meager volume, mucous in nature, colorless, and of a dense consistency. This type of sputum is called “vitreous.” Some patients may cough up small, dense pieces of mucus that block the bronchi.
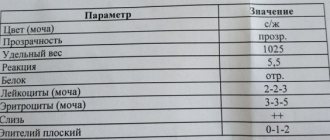
Decoding of indicators and norms
A healthy person does not normally produce sputum. There is only a mucous secretion from the bronchial tree, which is swallowed. Sputum is produced in increased volume during inflammation of the mucous membrane. The table below shows these norms, permissible deviations in general sputum analysis (for adults), as well as a more detailed explanation.
| Indicators | Norm | Decoding |
| Quantity | Up to 10 ml per day | 15-100 ml (for abscesses and bronchiectasis reaches 2 liters) per day |
| Color | colorless | Yellowish or green tint, the appearance of streaks of scarlet blood, brown or brownish color |
| Smell | — | Putrid, unpleasant |
| Consistency | mucous membrane | Dense, viscous |
| Red blood cells | — | Whole or broken |
| Leukocytes | — | Increased |
| Eosinophils | — | From single to many |
| Columnar epithelial cells | — | Present in tracheitis, asthma |
| Lymphocytes | — | Increased |
| Atypical cells | — | Available for neoplasms |
| Fibers | — | Found in tuberculosis or tumors |
| Crystals, spirals | — | Specific marker of bronchial asthma |
| Mushroom mycelium | — | Indicates mycosis of the lung |
The color and smell of sputum may indicate an acute or chronic phase of inflammation. If the sputum has a greenish tint, this indicates a bacterial infection.
The shade of red delineates the level of damage and age. If the sputum has red streaks, these are fresh red blood cells, possibly from damaged vessels in the upper respiratory tract. Brown color indicates congestion and breakdown of red blood cells. Normally, sputum usually has no odor, so the detection of a putrid odor during a general analysis immediately signals a purulent process.
The nature of the sputum depends on the causative agent of the disease. If it is a virus, the sputum will be mucous or serous. The addition of bacteria gives a purulent character and an increase in its number. Such sputum will occur in case of lung abscess, pneumonia, bronchiectasis, chronic obstructive disease.
How to submit it correctly?
{banner_banstat3}
Before donating sputum, no preparation is required; sample collection for general analysis is carried out in the morning, immediately after waking up, in accordance with the following algorithm:
- Brush your teeth.
- Rinse your mouth and throat.
- Cough up the mucus and spit it into a container.
If there is too little sputum, the doctor will prescribe plenty of fluids and expectorants the day before. To prevent excess microorganisms from getting into the sputum, it is better to purchase a collection container at a pharmacy. It is placed in a sterile package and has a tight-fitting lid.
“Methods for examining sputum for tuberculosis”
Date: 07/19/2018
Sputum is a secretion released during inflammation of the trachea, bronchi and lungs. Its appearance is noted not only with damage to the respiratory organs, but also with disorders of the heart and blood vessels. Methods for examining sputum involve macroscopic, chemical and microscopic determination of its characteristics.
What does the analysis reveal?
Examination of sputum makes it possible to detect microorganisms that cause the pathological process, identify the presence of mycobacteria in tuberculosis, identify cancer cells, blood and purulent impurities, and also determine bacterial resistance to antibiotics.
For what conditions is analysis indicated?
Sputum examination for general analysis is carried out in the following conditions:
- cough;
- pneumonia;
- inflammation of the bronchi;
- suppuration of the lung;
- tuberculosis;
- bronchiectasis;
- pulmonary gangrene;
- tumor in the lungs;
- acute bronchitis;
- chronic bronchitis;
- chronic tonsillitis;
- tuberculosis;
- whooping cough;
- silicosis;
- acute form of obstructive bronchitis;
- pneumonia;
- anthrax.
Preparing for the study
Mucus will be better released if you take an expectorant the day before the test or drink a large amount of warm drink. Before collection, it is recommended to clean your teeth and mouth by rinsing with warm boiled water.
Basic collection rules
It is advisable to collect sputum for bacteriological examination in the morning (it accumulates the night before meals) in a sterile container provided by the laboratory. An amount of 5 ml is sufficient for analysis. The secretion is analyzed no later than 2 hours after its collection. Until sent for testing, the container with the contents should be stored closed in the refrigerator.
The amount of sputum in various diseases
The amount of secretion released varies depending on the nature of the pathological process. Usually it varies from several spits to 1 liter per day. A small amount is released during inflammation of the bronchi, congestive processes in the lungs and at the onset of an attack of bronchial asthma. At the end of the attack the volume increases. It can be up to 0.5 l, and can also be released in large quantities if there is pulmonary edema.
A lot of mucus is released during a purulent process in the lungs when communicating with the bronchi, during suppuration, bronchiectasis and gangrene.
Examination of sputum for tuberculosis shows the breakdown of lung tissue. In particular, this process is provoked by the cavity, which communicates with the bronchi.
What is the reason for the decrease or increase in secretion secretion?
An increase in the amount of secretion secreted may be associated with a deterioration in the patient’s condition and may be observed during an exacerbation. An increase may also refer to positive dynamics in the development of the disease.
A decrease in the amount of mucus secreted may indicate regression of inflammation or a violation in the area of drainage of a cavity filled with pus. At the same time, there is a deterioration in the patient’s well-being.
Nature of the discharge
Mucous secretion is released during acute or chronic bronchitis, bronchial asthma, pneumonia, lung cancer, bronchiectasis, pulmonary echinococcosis accompanied by suppuration, actinomycosis.
Sputum mixed with pus is observed with lung abscess, echinococcosis and bronchiectasis.
Mucus mixed with blood or consisting entirely of blood is characteristic of tuberculosis. The appearance of blood may indicate the presence of oncology, bronchiectasis, or suppuration of the lung. This phenomenon is also observed in middle lobe syndrome, pulmonary infarction, trauma, actinomycosis and syphilitic lesions. Blood can also be released during lobar and focal pneumonia, congestive processes, cardiac asthma and pulmonary edema.
Serous sputum is observed with pulmonary edema.
Sputum color
Examination of sputum reveals its different colors. Mucous and serous discharge has no color or has a whitish tint.
The addition of pus gives the secretion a greenish tint, which characterizes such pathological processes as lung abscess, gangrene, bronchiectasis, and actinomycosis of the lung.
Discharge with a rusty or brown color indicates that it does not contain fresh blood, but a product of its breakdown - hematin. Such a secretion can be released during lobar pneumonia, anthrax, or pulmonary infarction.
A greenish color mixed with dirt or a yellow secretion indicates a pathology of the respiratory system in combination with jaundice.
Sputum turns bright yellow in eosinophilic pneumonia.
Ocher-colored mucus occurs with siderosis of the lung.
A blackish or grayish secretion is noted when there is an admixture of coal dust. With pulmonary edema, serous sputum is observed in large quantities. As a rule, it is colored uniformly pinkish, which is explained by the presence of red blood cells. Such discharge is similar to liquid cranberry juice.
The secretion may also become colored due to some medications. For example, the antibiotic Rifampicin can give it a red color.
Smell
The nature of the pathological process in the respiratory organs can also be indicated by the smell of the secretion. Sputum gives off the smell of rot in cases of gangrene of the lung or putrefactive lesions of the bronchi, oncological neoplasms, complicated by necrosis of bronchiectasis.
Availability of layers
Often, examination of secretions reveals the presence of layers. With a stagnant nature, sputum mixed with pus is observed with suppuration of the lung and bronchiectasis.
The secretion, mixed with rot, contains three layers. The top layer is foam-like, the middle layer is serous, and the bottom layer is mixed with pus. This composition characterizes lung gangrene.
Impurities
An admixture of food can be observed in the presence of a malignant tumor in the esophagus when it communicates with the bronchi and trachea. When echinococcus enters the bronchi, hooks or scolex of the parasite can be found in the sputum. Very rarely, adult roundworms are found that penetrate the respiratory system of weakened people.
Pulmonary fluke eggs appear when a cyst ruptures, which forms in the lungs in the presence of parasites.
Gangrene and suppuration of the lungs cause the appearance of pieces of pulmonary necrosis. If there is a tumor, fragments may be present in the discharge.
Convolutions containing fibrin are found in patients with fibrinous bronchitis, tuberculosis and pneumonia.
Rice bodies, or Koch lenses, are characteristic of tuberculosis.
Dietrich's plugs, which include decay products of bacteria and fatty acid tissue cells of the lungs, are found in putrefactive bronchitis or gangrene of the lung.
The chronic form of tonsillitis involves the release of plugs from the tonsils, similar to Dietrich's plugs.
Chemical method
Chemical examination of sputum involves determining:
- A protein indicator that can help in the differential diagnosis of chronic bronchitis and tuberculosis. With chronic bronchitis, traces of protein are noted in the secretion, and with tuberculosis, the amount of protein in the sputum will be much higher, and it can be indicated by numbers (up to 100-120 g/l).
- Bile pigments. They are found in sputum when the respiratory system is affected in combination with hepatitis. In this case, the liver communicates with the lungs. Bile pigments are inherent in pneumonia, which is caused by the breakdown of red blood cells inside the lungs and the subsequent change in hemoglobin.
Cytological method for studying secretions
For the differential diagnosis of tuberculosis and many other lung lesions, the cytological method is widely used, which includes two stages: clinical and microscopic examination of sputum.
A clinical study helps determine which method should be used to collect material to obtain the correct test result.
There are two main types of material required by microscopic examination of sputum: spontaneous and reduced. The second type of secretion is obtained by exposure to various irritants (expectorants, inhalations, etc.).
Material obtained from needle biopsy
Cytological examination of sputum involves the study of macroscopic and microscopic analysis of its cells.
The most information for cytological analysis is provided by sputum taken in the morning on an empty stomach. Before testing, it should be stored for no more than 4 hours.
- Sputum contains squamous epithelial cells, which are examined microscopically. But they have no significance for making a diagnosis. Columnar epithelial cells - both individually and in groups - can be observed in diseases such as bronchial asthma, bronchitis and lung cancer. It should be noted that columnar epithelium can also appear due to the penetration of mucus from the nasopharynx.
- Alveolar macrophages are reticuloendothelial cells. Macrophages, which are contained in the protoplasm (phagocytic particles or dust cells), can be found in patients who have inhaled dust for a long time.
- Protoplasmic macrophages (formed during the breakdown of hemoglobin) are called cardiac defect cells. They can occur during congestive processes in the lungs, mitral valve stenosis, and pulmonary infarction.
- A small number of leukocytes are found in any sputum. Their increased content is observed in secretions mixed with pus.
- Eosinophils. The sputum of asthmatics is rich in such cells. Cells can be observed in the eosinophilic form of pneumonia, helminth damage to the body, tuberculosis and pulmonary infarction.
- Red blood cells. Single red blood cells do not reflect the picture of the disease. The appearance of an increased amount indicates the presence of bleeding in the lungs. In fresh blood, unchanged red blood cells are detected. If there is an admixture of blood that has stagnated in the lungs for a long time, then leached red blood cells are detected.
- Cancer cells. They can be found in secret groups. They indicate the presence of a tumor. When single cells are found, diagnostic difficulties often arise. In such cases, a repeat sputum analysis is performed.
- Elastic fibers, the appearance of which is caused by the breakdown of lung tissue, provoked by tuberculosis, abscess, gangrene, tumor. Such cells are not always characterized by gangrene, since due to the action of secreted enzymes, they can be dissolved.
- Kurshman spirals. These are special bodies that look like tubes. They are detected when examined under a microscope. Sometimes visible to the eye. Typically, spirals are associated with diseases such as bronchial asthma, pulmonary tuberculosis and pneumonia.
- Charcot-Leyden crystals are found in sputum with an increased content of eosinophils in diseases such as bronchial asthma, eosinophilic pneumonia. Opening a focus of tuberculosis in the lumen of the bronchi can be characterized by the presence in the secretion of elastic fiber-crystals of cholesterol, MBT and amorphous lime (the so-called Ehrlich tetralogy) - 100%.
Application of bacterioscopy
Collecting sputum for examination by the bacterioscopic method involves analyzing the secretion to detect mycobacteria characteristic of tuberculosis. They look like thin curved sticks of different lengths, thickened on the sides or in the middle, which are located both individually and in groups.
The detection of Mycobacterium tuberculosis is not a dominant sign for diagnosis and requires confirmation by bacteriological methods. Tuberculous mycobacteria are not detected in secretions under normal conditions.
The basis for the analysis is purulent particles, which are taken from forty-six different areas and thoroughly ground to a homogeneous mass using two glasses. Next, they are dried in air and fixed with a burner flame.
Bacteriological examination of sputum using the Ziehl-Neelsen method suggests that it is stained red. In this case, all secretion particles, with the exception of mycobacteria, acquire a blue tint, and mycobacteria acquire a red color.
If the body is suspected of being affected by tuberculosis, after testing three times for the presence of mycobacteria with a negative response, the flotation method (Pottenger analysis) is used.
The usual method of examining a stained smear for MTB gives a positive result only when the amount of MTB is at least 50,000 units in 1 ml of sputum. The presence of tuberculosis cannot be judged by the number of mycobacteria.
Bacterioscopy of patients with nonspecific lung diseases
Laboratory tests of sputum in the presence of nonspecific lung diseases during bacterioscopy can reveal the following bacteria:
- For pneumonia - pneumococci, Frenkel diplococci, Friedlander bacteria, streptococci, staphylococci (100%).
- With gangrene of the lungs, a spindle-shaped rod can be found in combination with Vincent's spirochete (80%).
- Yeast-like fungi (70%), to determine the type of which requires culture of the secretion.
Author: Seytimova Moldir
Regional anti-tuberculosis dispensary
Bachelor laboratory assistant
07/17/2018
Bacteriological research
{banner_banstat4}
Bacteriological research is carried out to determine the exact causative agent of a particular disease. Most often, it is pneumonia or tuberculosis.
The resulting sputum sample is added to nutrient media and optimal conditions for growth are created. Pathogenic organisms begin to divide and actively grow. A few days later, a laboratory assistant examines the result, identifies the pathogen and gives a conclusion. The attending physician, based on this data, can either prescribe treatment or refer for additional diagnostic methods. Typically found in sputum:
- staphylococci and streptococci;
- Koch's stick;
- Pseudomonas aeruginosa and Klebsiella;
- various types of mushrooms;
- chlamydia and other protozoa.
Since bacteriological examination is quite complex and time-consuming to perform, it is prescribed only if the results of instrumental studies of the lungs are unclear. However, in some cases it is necessary to identify the causative agent of pneumonia, especially with an atypical course of the disease.
Why do they take it?
{banner_banstat5}
Bacteriological examination of sputum is a high-quality analysis, with a diagnosis accuracy of 100%. This is why they take sputum and grow bacteria on nutrient media:
- for testing for species specificity;
- to determine class membership;
- to detect sensitivity to antibiotics.
If a doctor is caring for a seriously ill patient in whom minimal examinations do not reveal the cause of lung disease, sputum helps verify the diagnosis. An important point is proper collection of sputum. The quality of the analysis and the correct result of the entire procedure depend on this.
For tuberculosis
{banner_banstat6}
If a doctor suspects a tuberculosis process, the primary step is to test sputum for Koch bacilli. They can be determined in several ways, including bacteriological (cultural). Before culture, a sputum sample is treated with special solutions to stop the growth of opportunistic bacteria. The growth of flora occurs over a fairly long period of time - from 14 to 90 days. An experienced laboratory technician will be able to differentiate a colony of Koch bacilli within 2-3 weeks. It has a gray-silver color and crumbles easily when touched. The growth rate depends on the number of bacteria in the sputum. The more there are, the faster the growth rate.
For pneumonia
In case of pneumonia, bacteriological examination of sputum is carried out quite rarely; a general analysis is usually indicated. The most common causative agent of the disease is Streptococcus pneumoniae. It causes up to 80% of community-acquired pneumonia, so treatment is based on the use of broad-spectrum antibiotics.
In some cases, the pathogen may be of a different nature, for example, fungal. Then the sputum must be examined by culture on a nutrient medium.
Fungi, chlamydia, listeria, E. coli, Staphylococcus viridans and many others can cause an atypical form of pneumonia, with the development of complications (abscess, pleurisy).
Collection algorithm
{banner_banstat7}
You can collect sputum for analysis both at home and in the clinic. In order to correctly submit sputum for analysis, it is recommended to follow a simple algorithm of actions:
- The procedure is carried out on an empty stomach, after brushing your teeth, rinsing your mouth and throat (to remove food debris and excess saliva).
- Wait for a good coughing attack.
- Keep the container as close to your lips as possible.
- With a deep cough, cough up the contents of the bronchi, avoiding strong expectoration.
- Close the container with a tight lid and transport to the laboratory within 2 hours.
More accurate results will be obtained if the collection is carried out directly in the clinic. For this purpose, there are sputum collection rooms with trained staff. Nurses will help you correctly collect a sample for research and deliver it to the laboratory as soon as possible.
Collection of biomaterial
Sputum for culture is collected in the morning before the first meal in a special sterile container with a tight-fitting lid. To ensure that impurities of saliva and mucus do not get into the biomaterial, the oral cavity and nasopharynx are thoroughly cleaned before collecting a sample for research.
Only fresh sputum isolated as a result of prolonged coughing can be analyzed.
Collecting sputum for culture and determining sensitivity to antibiotics is carried out before starting treatment with antibacterial drugs. Otherwise, the result may be false negative.
How much phlegm should you cough up?
The nurse will always tell you how much sputum is needed for bacteriological or microscopic examination in a particular case.
Usually it is enough to cough up 3-5 ml, which corresponds to completely filling the funnel at the bottom of the container.
If the discharge of secretions is difficult, you should increase the amount of fluid consumed the day before collection and take expectorants. If the volume is too large (for example, with bronchiectasis), it is recommended to cough up the first portion into a container and spit out the rest.
How long does the research take?
{banner_banstat8}
Sputum culture takes a long time because the bacteria need time to grow. After a few weeks, you can accurately determine their identity and sensitivity to the drugs. Thus, how long the analysis is done depends on the purpose and method of the study: the procedure takes from 1.5 to 3 months.
Sputum microscopy is a faster analysis. The speed of research depends on the order of the queue and the number of samples. On average, waiting for results takes from 1 to 2 days.