Nature gave blood a special property - to coagulate; without this, even minor tissue damage would be fatal - a person would simply die from blood loss. But in some pathologies this process is disrupted. By taking a blood clotting test and learning how the hemostasis system works, you can judge the presence of many diseases in the body.
APPOINTMENT WITH ANY DOCTOR BASED ON TEST RESULTS—RUB 500. CLICK TO SIGN UP
Determination of blood clotting ability is called a coagulogram (hemostasiogram). The study is prescribed to identify a number of pathologies (hemophilia, cancer, thrombosis, liver disease, kidney disease, etc.) and before surgery or childbirth.
Normally, hemocoagulation should take place only outside the body, otherwise the resulting clots will travel through the vessels to the heart, lungs or brain, forming blood clots and causing ischemia, heart attacks and strokes. By donating blood for clotting, you can determine its ability to coagulate (clotting). This helps the doctor assess the risk of bleeding or developing clots in the blood vessels.
Types of laboratory tests for clotting
The content of the article
The blood clotting test includes the following indicators:
- Fibrinogen levels
This substance is a protein produced by the liver. In a healthy person, fibrogen is 2-4 g/l. - Antithrombin III.
This is a hemocoagulation regulator. The antithrombin index is 75-125% in adults, 80-120% in children older than one month, and 30-80% in newborns. - Prothrombin index (PTI)
. The percentage ratio of hemocoagulation time in a particular person with a similar indicator in the control sample. Normally, PTI is 93-107%. - Thrombin time.
In healthy people it ranges from 14 to 20 seconds. During this period, prothrombin must be transformed into thrombin. The results may vary with the use of certain medications, such as aspirin or warfarin. The thrombin time (PT) test shows how well a person's blood clots. - Activated partial thromboplastin time (aPTT)
. The indicator is used to monitor the hemocoagulation process in patients prescribed heparin and in the diagnosis of DIC syndrome. Normally, this figure is 29-39 seconds. - Period (time) of bleeding.
Indicates how quickly the blood will stop if the integrity of small vessels is violated. To do this, a puncture is made on the patient's finger and the time is noted. Normally it is 2-3 minutes. - Clotting time.
Determined by the time interval between blood sampling and clot formation. In healthy people, this process takes from 2 to 5 minutes. - D-dimer
. This is a substance formed as a result of the decomposition of fibrin. Normally, this figure should be no more than 250 mcg/l (0.25 mcg/ml).
Definitive blood tests
These types of blood tests are very different from those listed above in that they do not diagnose any disease or health condition of a person, but simply indicate the peculiarity of his circulatory system. These include tests to determine blood type, Rh factor and coagulation. As a rule, these studies are mandatory for people in special professions, as well as for all pregnant women. Blood is taken for analysis from a vein and does not require special preparation of the patient.
How to donate blood for clotting
Determination of bleeding time is carried out using capillary blood; for other clotting tests, material must be taken from a vein.
The tests are carried out on an empty stomach; you can only drink water before the analysis. If you are taking any medications, you should tell your doctor about this, as some medications may affect the results obtained.
By regularly taking hemostasiogram tests, you can promptly diagnose many dangerous ailments.
Increased blood clotting and thrombus formation
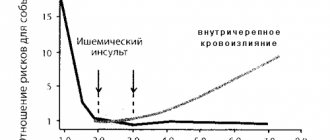
Many factors can lead to increased blood clotting, restriction or blockage of blood flow, and as a result, blood clots. Blood clots can travel through arteries and veins, causing serious consequences including sudden death from embolism.
Indications for examination
Normal blood clotting is 2-5 minutes (according to Sukharev). An analysis to determine this indicator (coagulogram, hemostasiogram) is prescribed for:
- diseases of internal organs;
- suspected hereditary hemostatic pathologies;
- pregnancy;
- varicose veins, thrombus formation;
- diabetes mellitus;
- prescribing coagulants;
- during the preoperative and postoperative period.
Risk factors
Increased hemocoagulation often occurs when:
- increased number of blood cells and hemoglobin, radiation, cancer;
- hyperfunction of the spleen, acidification and dehydration of the body, most often associated with poor bowel function;
- increased consumption of sugar and carbohydrates;
- overweight, pregnancy, prolonged bed rest, sedentary lifestyle and sedentary work;
- lack of specific hormones and enzymes, use of birth control pills or hormone replacement therapy.
Sometimes the tendency to hyperclotting is congenital. This pathology is called thrombophilia. It is caused by a congenital decrease in the level of anticoagulants C and S, antithrombin III, coagulation factor VII, heparin cofactor II, dysfibrinogenemia, sickle cell anemia, hyperlipoproteinemia, increased activity of Hageman factors, Rosenthal factors and antihemophilic globulin. With this pathology, patients report similar cases among close relatives. Sometimes hereditary thrombophilias cause miscarriages in women.
Blood thickening in old age threatens to disrupt brain activity, and in pregnant women it can negatively affect the condition of the mother and fetus. Poor rheology leads to ischemia of organs and tissues, which negatively affects the condition of the entire organism.
How to suspect increased coagulability
- A sign indicating increased hemocoagulation is thrombus formation. If you notice painful bluish “vessels” or nodules on the limbs, this is a reason to consult a doctor and be examined for blood clotting indicators.
- Another symptom that should alert you is problems with the functioning of the heart. They should encourage you to get tested.
If the coagulogram indicators do not correspond to the norm, treatment must be started urgently to prevent thromboembolism.
Blood chemistry
It is carried out to assess the functional state of the body, the functioning of its internal organs, as well as metabolism. This blood test can check your blood levels of protein, sugar, iron, cholesterol, bilirubin, triglycerides, various enzymes, calcium, magnesium, sodium, phosphorus and various gases. Any deviation from the norm may signal that some processes may be going on in the body that are invisible from the outside (parasitic infections, tumors, allergies). Patients with poor results of biochemical analysis may have diseases of the thyroid gland, liver, and possible diabetes mellitus and atherosclerosis. Depending on the type of biochemical analysis, preparation for blood sampling may vary, including following a diet for several days.
How to prepare for a biochemical blood test?
One day before taking blood for biochemistry, it is necessary to avoid drinking alcohol, and 1 hour before taking smoking. It is advisable to take blood samples on an empty stomach in the morning. There should be at least 12 hours between the last meal and the blood draw. Juice, tea, coffee, chewing gum are not allowed. You can drink water. It is necessary to exclude increased psycho-emotional and physical stress.
How are the results of a biochemical blood test evaluated?
The use of different diagnostic methods by different clinics leads to different results, and the units of measurement may also differ. Therefore, to correctly decipher the result of a biochemical blood test, a consultation with the attending physician is required.
What indicators are included in a standard biochemical blood test?
1) Glucose (in blood) is the main test in the diagnosis of diabetes mellitus. This analysis is very important when selecting therapy and assessing the effectiveness of diabetes treatment. A decrease in glucose levels is observed in some endocrine diseases and liver dysfunction.
Normal blood glucose levels:
| Age | Glucose level, mmol/l |
| < 14 years | 3,33 — 5,55 |
| 14 – 60 years | 3,89 — 5,83 |
| 60 - 70 years | 4,44 — 6,38 |
| > 70 years | 4,61 — 6,10 |
2) Common bilirubin is a yellow blood pigment that is formed as a result of the breakdown of hemoglobin, myoglobin and cytochromes. The main reasons for the increase in the amount of total bilirubin in the blood: damage to liver cells (hepatitis, cirrhosis), increased breakdown of red blood cells (hemolytic anemia), impaired outflow of bile (for example, cholelithiasis).
Normal values of total bilirubin: 3.4 - 17.1 µmol/l.
3) Direct bilirubin (conjugated, bound bilirubin) - a fraction of total blood bilirubin. Direct bilirubin increases with jaundice, which develops due to a violation of the outflow of bile from the liver.
Normal values of direct bilirubin: 0 - 7.9 µmol/l.
4) Indirect bilirubin (unconjugated, free bilirubin) - the difference between the indicators of total and direct bilirubin. This indicator increases with increased breakdown of red blood cells - with hemolytic anemia, malaria, massive hemorrhages in tissue, etc.
Normal values for indirect bilirubin: < 19 µmol/l.
5) AST (AST, aspartate aminotransferase) is one of the main enzymes synthesized in the liver. Normally, the content of this enzyme in the blood serum is low, since most of it is found in hepatocytes (liver cells). An increase is observed with liver and heart diseases, as well as with long-term use of aspirin and hormonal contraceptives.
Normal AST values:
- Women – up to 31 U/l;
- Men - up to 37 U/l.
6) ALT (ALT, alanine aminotransferase) is an enzyme synthesized in the liver. Most of it is located and works in liver cells, so normally the concentration of ALT in the blood is low. An increase is observed with massive death of liver cells (for example, with hepatitis, cirrhosis), severe heart failure and blood diseases.
Normal ALT values:
- women – up to 34 U/l;
- men – up to 45 U/l.
7) Gamma-GT (gamma-glutamyltransferase) is an enzyme found primarily in the cells of the liver and pancreas. An increase in its amount in the blood is observed with diseases of these organs, as well as with prolonged use of alcohol.
Normal gamma-GT values:
Men < 55 U/l
Women < 38 U/l
 Alkaline phosphatase is an enzyme widely distributed in human tissues. The hepatic and bone forms of alkaline phosphatase are of greatest clinical importance, the activity of which is determined in the blood serum.
Alkaline phosphatase is an enzyme widely distributed in human tissues. The hepatic and bone forms of alkaline phosphatase are of greatest clinical importance, the activity of which is determined in the blood serum.
Normal alkaline phosphatase values: 30-120 U/l.
9) Cholesterol (total cholesterol) is the main blood lipid that enters the body with food and is also synthesized by liver cells.
Normal cholesterol levels: 3.2-5.6 mmol/l.
10) Low-density lipoproteins (LDL) are one of the most atherogenic, “harmful” lipid fractions. LDL is very rich in cholesterol and, transporting it to vascular cells, lingers in them, forming atherosclerotic plaques.
Normal LDL levels: 1.71-3.5 mmol/l.
11) Triglycerides are neutral fats found in the blood plasma, an important indicator of lipid metabolism.
Normal triglyceride levels: 0.41-1.8 mmol/l.
12) Total protein - an indicator reflecting the total amount of proteins in the blood. Its decrease is observed in some diseases of the liver and kidneys, accompanied by increased excretion of protein in the urine. Increased in blood diseases and infectious and inflammatory processes.
Normal values for total protein: 66-83 g/l.
13) Albumin is the most important blood protein, making up approximately half of all serum proteins. A decrease in albumin content can also be a manifestation of certain diseases of the kidneys, liver, and intestines. Elevated albumin is usually associated with dehydration.
Normal albumin values: 35-52 g/l
14) Potassium (K+) is an electrolyte found primarily inside cells. An increase in the level of potassium in the blood is most often observed in acute and chronic renal failure, a sharp decrease in the amount of urine excreted or its complete absence, most often associated with severe kidney disease.
Normal potassium values: 3.5-5.5 mmol/l.
15) Sodium (Na+) is an electrolyte found primarily in extracellular fluid and in smaller quantities inside cells. It is responsible for the functioning of nervous and muscle tissue, digestive enzymes, blood pressure, and water metabolism.
Normal sodium values: 136-145 mmol/l.
16) Chlorine (Cl-) is one of the main electrolytes, which is in the blood in an ionized state and plays an important role in maintaining water-electrolyte and acid-base balances in the body.
Normal chlorine values: 98-107 mmol/l.
17) Creatinine is a substance that plays an important role in the energy metabolism of muscle and other tissues. Creatinine is completely excreted by the kidneys, so determining its concentration in the blood is of greatest clinical importance for diagnosing kidney diseases.
Normal creatinine values:
- men - 62 – 115 µmol/l;
- women - 53 - 97 µmol/l.
18) Urea is a substance that is the end product of protein metabolism in the body. Urea is excreted by the kidneys, so determining its concentration in the blood gives an idea of the functional abilities of the kidneys and is most widely used for diagnosing renal pathology.
Normal urea values: 2.8-7.2 mmol/l
19) Uric acid is one of the end products of protein metabolism in the body. Uric acid is completely excreted by the kidneys. An increase in the concentration of uric acid occurs in kidney stones and other kidney diseases that occur with renal failure.
Normal uric acid values:
- men - 210 - 420 µmol/l;
- women - 150 - 350 µmol/l.
20) C-reactive protein (CRP) is a sensitive element in the blood that reacts faster than others to tissue damage. The presence of reactive protein in blood serum is a sign of an inflammatory process, injury, or penetration of foreign microorganisms into the body - bacteria, parasites, fungi. The more acute the inflammatory process, the more active the disease, the higher the C-reactive protein in the blood serum.
Normal values for C-reactive protein: 0 - 5 mg/l.
21) Iron (serum iron) is a vital microelement that is part of hemoglobin, is involved in the transport and deposition of oxygen and plays an important role in hematopoiesis.
Normal serum iron values:
- women - 8.95 - 30.43 µmol/l;
- men - 11.64 - 30.43 µmol/l.
Diseases accompanied by increased blood clotting
- Atherosclerosis. With atherosclerosis, plaque forms inside the arteries. Over time, the plaque can rupture and platelets form clots at the site of injury.
- Vasculitis causes inflammation of blood vessels, platelet aggregation and, as a result, an increase in coagulogram parameters.
- Diabetes causes plaque to form in the arteries, which is why nearly 80 percent of people with the disease eventually die from causes related to blood clots and ischemia.
- In heart failure, this organ cannot pump enough blood to meet the body's needs, its circulation slows down, it thickens and blood clots appear.
- High blood clotting is often observed in patients with varicose veins. In this case, blood clots have to be “liquefied” with the help of special drugs to prevent gangrene and necrosis associated with poor blood flow.
- This figure also increases in some infectious diseases, especially those accompanied by fever. In this case, the blood becomes viscous, so patients are prescribed plenty of fluids and intravenous infusions of solutions.
Elevated coagulogram values are very dangerous, as this condition can lead to serious complications and serious consequences.
Fibrinogen is increased: what does this mean?
Elevated levels of fibrinogen in the blood may mean activation of the blood clotting system, the possibility of excessive thrombus formation, or the occurrence of an acute inflammatory process in the body.
Thus, high fibrinogen protein is observed in severe, abnormal conditions that affect vital organs and the entire body as a whole. Among these diseases are:
- inflammatory-immune damage to connective tissue;
- death of the heart muscle as a result of acute lack of blood supply;
- kidney diseases;
- infectious diseases;
- endocrine diseases (diabetes mellitus);
- pneumonia;
- mild forms of inflammatory process in the liver;
- initial stage of thrombohemorrhagic syndrome;
- tuberculosis;
- oncological diseases.
Also, an increase in fibrinogen levels occurs during pregnancy, which is due to the natural physiology of the female body. Increased rates are observed with oral contraception and taking steroid female sex hormones.
How to suspect deterioration of coagulation hemostasis
The first signs indicating poor blood clotting
Prolonged bleeding occurs with minor skin injuries or after injections. Normally, cuts or injections should not bleed for more than 3-5 minutes, but if there is pathology, this time can increase significantly. Sometimes such people have hemorrhages under the skin.
Another symptom that indicates this condition is prolonged nosebleeds that are difficult to stop. Women with hemocoagulation disorders may experience menorrhagia and metrorrhagia. Sometimes traces of blood may even be present in urine and feces.
If these symptoms appear, it is recommended to donate blood for a coagulogram. Research conducted by our specialists will help identify disorders of coagulation hemostasis. All analyzes are carried out using modern equipment and reagents.
Reasons causing deterioration of hemocoagulation
Medications
- Coumarin group drugs reduce coagulation because they are vitamin K antagonists. These drugs are used to protect against thrombosis after major operations, but if prescribed incorrectly, these substances can significantly worsen blood clotting.
- Aspirin, often used for colds and heart pathologies, taken in high doses, can also cause a decrease in clotting rates.
- In some cases, this effect is achieved by a combination of several drugs that are not recommended to be taken together.
In such cases, after determining the clotting time and duration of bleeding, the patient is prescribed vitamin K, which plays an important role in the process of hemostasis. Patients are recommended to eat green vegetables (cabbage and spinach), eggs, milk and cereals, which eliminate the deficiency of this vitamin.
Hereditary diseases
- Hemophilia . This disease is hereditary and affects only boys. In patients, symptoms of decreased blood clotting appear in early childhood. With this disease, various coagulation factors may be absent, so the disease may be more or less severe. Patients are treated by a hematologist for life. Replacement therapy, blood transfusions and restriction of physical activity are carried out.
- Von Willebrand syndrome is also characterized by decreased clotting, but it affects both men and women. To treat patients, tranexamic acid, desmopressin are used, and blood transfusions are performed.
Other pathologies
A decrease in the number of platelets (thrombocytopenia) occurs in various anemic conditions, leukemia, after radiation therapy, viral infections, taking antibiotics and some other drugs. This condition can be caused by diseases of the liver, kidneys and spleen. This condition is treated by administering special blood products.
Another reason for impaired hemocoagulation is liver disease, which disrupts the synthesis of substances responsible for proper hemostasis. A decrease in PTI and an increase in blood clotting time are considered as an indirect sign of hepatitis.
A decrease in coagulogram parameters may be observed after operations accompanied by heavy blood loss. This condition does not pose a threat to human health and goes away on its own.
Properly selected treatment to reduce hemocoagulation will help avoid severe blood loss and serious complications.
Blood clotting indicators during pregnancy
Every pregnant woman registered at the antenatal clinic is necessarily referred by a gynecologist for an analysis called a hemostasiogram. The results of a hemostasiogram make it possible to determine the presence of disorders in the blood coagulation system, if any.
The role of hemostasis during pregnancy
Hemostasis acts as a “thickener” of blood; thanks to this system, a person avoids significant blood loss in cases of vascular damage. In tandem with the coagulation system, an anticoagulant acts in the body - a “thinner” of the blood. When the balance is disturbed, the systems malfunction, as a result, the blood can become too viscous, which leads to the formation of blood clots, or too liquid, in both cases the blood clotting time changes.
What are the dangers of impaired hemostasis for pregnant women?
Increased blood clotting during pregnancy can provoke disseminated intravascular coagulation syndrome, in which thickening blood in the vessels causes disruption of placental blood flow. The condition is dangerous for the baby, as he cannot receive adequate nutrition, which immediately affects his development. In severe cases, pregnancy may stall, and ultimately the fetus dies. Timely testing for hemostasis gives a great chance to avoid such complications.
Disorders of the coagulation system can cause premature separation of the placenta, even if it is in a normal location.
When is it necessary to take a blood clotting test?
It is recommended to perform a hemostasiogram before the expected pregnancy. In case of poor performance, you can undergo a course of therapy, which the doctor will select individually. The risk group that requires mandatory preliminary screening for coagulation includes women:
- having relatives who have suffered a stroke, heart attack, thrombosis, varicose veins;
- suffered a miscarriage or frozen pregnancy;
- athletes and those working in heavy work.
During pregnancy, it is also necessary to undergo diagnostics, especially if the doctor diagnoses:
- recurrent miscarriage - the presence of two or more unsuccessful pregnancies (miscarriage, fading);
- gestosis - swelling of the extremities, protein in the urine, high blood pressure;
- threat of miscarriage.
If there is gestosis during pregnancy, blood clotting increases in 70% of cases, which aggravates treatment. You can also prevent the situation by taking a timely test and undergoing therapy.
Methods for treating hemostasis disorders in pregnant women
With timely diagnosis of hemostasis disorders, many complications of pregnancy can be avoided. In European medical practice, DIC syndrome is treated with low molecular weight heparins, which are absolutely safe for the fetus. Treatment can be done at home with the permission of a gynecologist, subject to control tests (every 2 weeks). At the same time, doctors prescribe antioxidants, aspirin-containing drugs, folic acid, and vitamin B.
If the patient does not have the opportunity to buy expensive low molecular weight heparins, the specialist can replace them with regular heparin. In this case, strict monitoring of the results and condition of the pregnant woman is necessary, since the dose of an unfractionated drug is very difficult to select immediately; you will have to visit the clinic twice a week. For control, you need to periodically take a blood clotting test.
If you find an error, please select a piece of text and press Ctrl+Enter
Who needs to determine blood clotting?
To reduce the risk of developing vascular accidents and unexpected bleeding, it is necessary to periodically monitor the state of the blood coagulation system using a laboratory method. This is especially important for:
- people over 40 years old;
- women during and after menopause;
- women during pregnancy;
- people who regularly take blood thinners (aspirin);
- patients suffering from varicose veins;
- those preparing for surgery, etc.
The doctor must prescribe blood clotting tests if hemophilia is suspected (usually this disease is detected in early childhood and young adulthood) or when treating an existing thrombosis with fibrinolytic therapy and anticoagulants.