A planned caesarean section (PCS) is an operation to remove the fetus from the uterus (delivery) with pre-known indications and a set date (usually 38-39 weeks). Prescribed for contraindications to normal childbirth, both from the mother (narrow pelvis, diseases) and the fetus (severe condition, large). Before the operation, it is necessary to undergo tests and an ultrasound, then the operation can take place on the day of admission.
During this procedure, an anesthetic is administered, the skin of the lower abdomen is cut, then the uterus is cut, the fetus is removed and the tissue is sutured in layers. In uncomplicated cases, this lasts no more than 1 hour. After a caesarean section, the first few days of feeding are gentle; you can get up after 6 hours, walk after 12 hours, and on the 4-6th day the woman is discharged home.
When is a caesarean section indicated?
Sometimes caesarean section
prescribed for medical reasons even before the onset of the first contractions.
Planned caesarean section
prescribed for an anatomically narrow pelvis in a pregnant woman, with complete placenta previa, or if the previous pregnancy was also resolved by cesarean section and a scar on the uterus with signs of thinning. Also among the reasons for which a planned cesarean section is prescribed: severe gestosis during pregnancy, the presence of chronic diseases in the mother such as heart disease, diabetes, hypertension, kidney disease, in which natural childbirth poses a risk, as well as exacerbation of genital infections at the time of birth (for example genital herpes).
Sometimes the mother herself chooses the option of a cesarean section, but, as a rule, in the absence of serious complications, doctors strongly recommend natural childbirth.
Relative readings
The section is also carried out in relative indications, when childbirth is possible naturally, but with rather high risks. To minimize the risk, a cesarean section is preferred. Such indications include:
- chronic pathologies in women, for example, due to kidney disease, eye disease, diabetes;
- the presence of cancerous tumors;
- diseases of the nervous system;
- conception occurred after infertility treatment;
- complication during pregnancy, for example, gestosis;
- childbirth proceeds with disturbances, weakly, despite intensive treatment;
- the fruit is too large;
- breech presentation of the fetus.
In what cases is an emergency caesarean section performed?
It happens that the mother was preparing for a natural birth, but an emergency caesarean section is prescribed. Sometimes this happens in the last weeks of pregnancy or even during childbirth. For example, in such situations: the mother develops preeclampsia or placental abruption has occurred, the cervix stops dilating during contractions, the uterus ruptures, Also, an emergency caesarean section is indicated if the fetus has an abnormal heartbeat or distress syndrome has developed, or if the baby is not moving along. birth canal.
Preparing for a planned caesarean section in the maternity hospital
When preparing for a planned caesarean section, a woman must undergo an examination and provide research results before hospitalization in the maternity hospital:
- blood and urine tests;
- ECG, ultrasound;
- cardiotocography (fetal heart function).
If you have had a previous cesarean section (before the current birth), removal of fibroids or similar interventions, a statement is required indicating the volume, suture material, and recovery after the procedure. All this examination can be carried out in a hospital if hospitalization is carried out 2 weeks before the expected delivery.
Fetal cardiotocography
If the preparation was completed in the clinic, then the woman is admitted to the hospital the night before or on the day of the operation. Upon admission, she is examined by a gynecologist, surgeon and anesthesiologist; they may also involve other specialists for concomitant diseases (for example, a cardiologist). The doctors' conclusion indicates the possibility of surgical delivery, the type of anesthesia, and the need to prevent complications with medications.
The gynecologist evaluates:
- fetal heartbeat;
- position of the baby in the uterus;
- what presentation (part of the body that is closer to the exit from the uterine cavity), since the surgical technique depends on this;
- condition of the uterus, vagina, cervix, discharge.
Normally, amniotic fluid should be clear or slightly yellowish.
The woman in labor fills out the form “Informed Consent for Caesarean Section.”
How is a caesarean section performed?
As with any operation, before a cesarean section, medical preparation is carried out, an IV with fluids is placed, and the skin is treated with an antiseptic. In some cases, anesthesia may be an epidural or spinal, in other cases, especially in the case of an emergency caesarean section, general anesthesia is performed.
The surgeon makes a horizontal incision 10-15 centimeters long along the pubic bone (along the bikini line). He then separates the abdominal muscles with a scalpel and makes a through incision into the uterus. You may experience a slight tugging sensation as you remove the baby. The doctor then cuts the umbilical cord and removes the baby.
Immediately after birth, you will be allowed to look at the baby, but not for very long, because doctors need to measure his pulse and temperature and evaluate the color of his skin. While the baby is being examined, the placenta is removed, the uterus is sutured, and an incision is made in the abdomen. You will also be given antibiotics to prevent infection.
You will then be moved to the recovery room for observation for a few hours. During this time, you can hold your baby, try breastfeeding, and hold him close to your skin.
Progress of the operation
First, drugs for general or regional anesthesia are administered, the skin and uterus are cut, the baby and placenta are removed, the tissue is sutured, and the patient is transferred to the recovery room.
What kind of anesthesia will it be?
The vast majority of women (about 90%) use spinal or epidural anesthesia. It is carried out in this way: a solution of the drug is injected between the lumbar vertebrae with a thin spinal needle or a set (needle + catheter) for epidural anesthesia.
There is a complete loss of sensitivity from the lower back to the feet, which allows you to perform all the necessary manipulations without pain and discomfort. The woman in labor is conscious all the time, she is separated from the surgical field by a screen, but can maintain contact with the surgeon. After the baby is born, you can immediately put it to the breast.
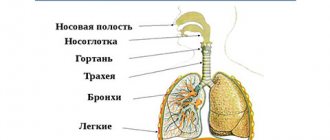
If such regional anesthesia is contraindicated, or there is a need for a long operation, then general anesthesia is prescribed. The drugs are first injected into a vein, then, after the onset of drug-induced sleep, a tube is installed into the trachea through which the gas mixture is supplied. With the help of these medications, complete relaxation of the muscular system and loss of consciousness occurs.
How is a second planned caesarean section performed?
The second cesarean section differs from the first in that the incision is made close to an existing scar.
All other stages of the operation are similar:
- The incision in the skin of the subcutaneous layer (for most women with a planned cesarean section, it is horizontal above the pubis, no more than 10 cm, this protects against hernias and heals faster).
- Dissection of the uterus in the lower part.
- Opening the membranes, removing amniotic fluid.
- Removing the child.
- Crossing the umbilical cord.
- Removal of the placenta.
- Layer-by-layer suturing of tissues.
- Fixing a protective bandage on the skin and placing an ice pack on top.
After the second, and especially the third, caesarean section, the woman is offered tubal ligation surgery. This is a fairly reliable way to prevent unwanted pregnancy in the future, since carrying a fetus with scars on the uterus is very dangerous.
Possible complications and their prevention
With a caesarean section, especially a repeat one, there are risks of complications:
- blood loss exceeding the norm (up to 500-750 ml is allowed) - the uterine cavity, due to strong muscle relaxation during anesthesia, can be difficult to contract; to prevent severe anemia, blood or its components are injected, and if the bleeding cannot be stopped, then removal of the uterus is necessary ;
- adhesive disease - any operation in the abdominal cavity during healing causes the formation of adhesions, that is, fibers that connect the organs of the adhesive disease (for example, intestinal loops, bladder with the body of the uterus), which later lead to the appearance of chronic pain in the abdominal area, and if they affect the patency of the fallopian tubes, they become the cause of ectopic pregnancy and infertility; treatment – physiotherapy, therapeutic exercises;
- inflammation of the inner layer of the uterus (endometritis) - occurs due to the penetration of bacteria into the uterine cavity; for prevention, antibiotics are mandatory before surgery;
- infection of the suture - accompanied by redness, pain, discharge, fever, to prevent this, the woman is prescribed treatment with antiseptic solutions, and at home must be lubricated with wound-healing ointments (Levomekol, Bepanten plus);
- the formation of a rough scar at the site of skin stitching - Contractubex and Dermatix are used to soften and form a thin seam;
- divergence of the edges of the wound - occurs when there is an understanding of the severity, strong straining during bowel movements, hacking cough in the first days, as well as when an infection is attached; medications are prescribed for treatment; surgical debridement of the wound and re-application of suture material may be necessary.
How long does it take to recover after a caesarean section?
Recovery is an individual process, but in general it takes longer to recover from a cesarean section than from a vaginal birth. As a rule, after a cesarean section, the mother remains in the hospital for several more days, and doctors monitor her health and the healing of the postoperative wound.
Try to get plenty of rest, although it’s not easy with a newborn baby. Do not lift anything heavier than the baby, regularly wipe the post-operative scar with an antiseptic to prevent infection. Choose loose clothing to prevent chafing and irritation in the scar area. Don't drive or exercise until your doctor tells you to (usually two to four weeks after giving birth). Recovery after a caesarean section without complications takes 4-6 weeks.
How long will it take for full recovery?
The same amount as required after a normal birth: that is, about 2 months.
During the first days of recovery, mom may experience:
- painful contractions of the uterus (especially while feeding the baby);
- bloody discharge will gradually decrease, turning into bloody and then serous;
- pain in the suture area, sensitive in the first days, will decrease within 3-5 days.
As after childbirth, in the first 2 months a woman is not recommended to take a bath or be sexually active.
Is it possible to feel contractions and other labor symptoms during a cesarean section?
If you have a planned caesarean section, it is usually done before contractions start, so you won't feel them. But sometimes, after contractions begin, the mother may need an emergency caesarean section. So whether you're preparing for a C-section or not, it's worth familiarizing yourself with the signs of labor you can expect in the third trimester, typically between 38 and 42 weeks.
And remember, doctors and other hospital staff will be able to take care of you, regardless of whether you have a cesarean section or a vaginal birth.
Preparing for surgery in the maternity hospital
In the maternity hospital, before the operation, the necessary preparation is required: blood tests are taken, an enema is performed in the morning, a catheter is inserted, stockings are put on or an elastic bandage is applied to the legs, and the surgical field is treated.
What tests are taken?
The scope of tests that are performed in a hospital depends on how fully the preparation has been carried out in the clinic. Typically, women are already admitted with the following blood test results:
- clotting;
- general;
- biochemical tests - sugar, cholesterol, kidney and liver tests;
- for HIV, viral hepatitis, syphilis;
- group and Rh factor.
The last analysis, regardless of its availability, is always carried out in the hospital. Since doctors should always be prepared for the need for transfusion of blood or its components due to bleeding.
Watch the video on how to prepare for a caesarean section:
Is an enema done before surgery and how?
An enema before a cesarean section is not considered strictly necessary, especially if a complete bowel movement occurs in the morning. However, in most cases it is still better to carry out additional cleansing. To do this, use ordinary cool water; it is injected into the rectum in such a volume that does not cause severe pain.
When the urge to defecate appears, the procedure stops and the woman must visit the toilet. The time of the enema should not be later than 1.5 hours before the cesarean section.
Catheter before CS
Since during anesthesia the reflex to urinate will be lost for some time, a thin catheter is installed to remove urine into the lumen of the urethra. It is placed on the operating table and removed after the woman enters the ward.
What else is done on the day of surgery?
In the morning, the pregnant woman takes a shower, shaves her pubic hair and puts on elastic stockings or bandages on her legs in order to prevent blood clots and congestion of the veins of the lower extremities.
What can be unplanned situations during repeated births after a CS?
If labor has not started after 40 weeks, the doctor and woman discuss three options:
- wait for labor to begin;
- stimulate labor - and then the risk of suture divergence on the uterus increases;
- repeat caesarean section.
You should always be prepared to change your birth plan. After all, events may occur that increase the risks and require an emergency cesarean section according to indications - for example, a large fetus or the occurrence of preeclampsia, or stimulation of labor will be required.
If a woman has contractions as scheduled after a previous planned caesarean section, she should come to the hospital so that an emergency caesarean section can be performed if necessary. If labor progresses quickly and without complications, and provided the baby is healthy, a natural birth may be an appropriate choice.
When to plan a new pregnancy after a CS?
You need to wait about a year (any woman who has given birth needs this interval).
Usually, the suture after a cesarean section heals within three months after the birth of the child. However, if more time passes, it will heal better. A poorly healed scar can cause problems in the future, because in this case there may be a risk of uterine rupture along the existing scar. And although the risk is low, it increases if the interval between pregnancies is short (less than 1-1.5 years). Also, the rapid occurrence of a new pregnancy after a CS is accompanied by an increased risk of low placental attachment or placental abruption.
Many women experience postpartum depression, emotional stress or simply fatigue after pregnancy and surgery - in such situations the body also needs rest. Of course, a woman may have reasons to plan a new pregnancy soon after the CS (age or the desired small difference in the ages of the children). In such cases, it is necessary to consult a doctor and make sure that the suture on the uterus has healed and the body is ready to bear a new pregnancy.
Antibiotic prophylaxis during cesarean section: is it really necessary?
If a woman is at high risk of developing an infection, the prescription of antibiotics is not in doubt.
Regarding the prescription of antibiotics in other cases:
- There are studies that show that antibiotic prophylaxis in all women reduces the incidence of endometritis, wound infection and fever after CS;
- other experts argue that antibiotics can only be used in women at risk of infectious complications (and only those antibiotics are prescribed for which breastfeeding is allowed);
- Most studies show that there are more benefits than risks to using antibiotics before surgery or immediately after cutting the umbilical cord.