IDIOPATHIC HEMOSIDEROSIS OF THE LUNG
(haemosiderosis idiopathica pulmonum
; Greek idios own, special + pathos suffering, disease; hemosiderosis; synonym:
idiopathic brown induration of the lungs, essential pulmonary hemosiderosis, pneumohemorrhagic remitting hypochromic anemia, Zelena-Gellerstedt syndrome
) - a disease characterized by repeated hemorrhages niyami into the lungs, the development of hemosiderosis and pulmonary sclerosis, anemia.
Idiopathic pulmonary hemosiderosis was first described by R. Virchow in 1864. The disease is rare, affecting mainly children aged 3-8 years; cases of familial disease have been reported.
Etiology and pathogenesis
The etiology and pathogenesis have not been sufficiently studied. It is believed that the cause of the disease is primary underdevelopment of the elastic framework of the pulmonary vessels, resulting in aneurysms, blood stasis and diapedetic hemorrhages in the lungs. The role of infections and intoxications cannot be ruled out (there are frequent cases of I. hepatitis after whooping cough, measles, acute respiratory diseases, pneumonia), although the role of microbes and viruses in the genesis of the disease has not been proven. Great importance in the development of the disease began to be attached to allergies and autoallergy (see), connections with the frequent combination of I. g. l. with Henoch-Schönlein disease, glomerulonephritis, myocarditis, as well as based on the characteristics of the course of the disease in the form of crises with an increase in the level of blood immunoglobulins, the effect of early extirpation of the spleen and the need for steroid therapy.
4.Treatment
Recently, corticosteroid hormonal drugs have become the standard of therapeutic support for patients with pulmonary hemosiderosis. Many authors believe that a combination of hormonal therapy with removal of the spleen is more effective. Drugs used in the treatment of iron deficiency anemia are also prescribed symptomatically; For the same purpose, blood transfusions are performed according to indications.
Although the results of this comprehensive approach are assessed in the literature as “encouraging”, the prognosis remains unfavorable. Only with a reliably and correctly established diagnosis, intensive adequate treatment and observation, the life expectancy of patients exceeds 10 years; on average, this indicator still remains at the level of 3-5 years.
Sign up for a consultation
Pathological anatomy
Changes in lung tissue during I. g. l. are similar to changes in secondary brown compaction of the lungs (see), however, hemosiderosis (see) is more pronounced and is more often combined with multiple hemorrhages. In the pulmonary alveoli, interalveolar septa, lymph, vessels and lymph nodes of the lungs, accumulations of macrophages loaded with hemosiderin and ferritin appear. The elastic framework of the lung and pulmonary vessels changes more sharply and peculiarly. Hyperplasia of elastic tissue is combined with its destruction, ruptures and twisting of fibers, elastolysis and giant cell macrophage reaction to fragments of elastic structures; often they become ferruginous and calcified.
Clinical picture
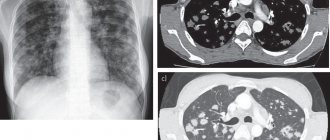
The disease is manifested by a triad of symptoms: hypochromic anemia, periodic hemoptysis and characteristic symmetrical damage to the lungs (diffuse, dense, spotty, network-like opacities in the lungs, the main pattern in the middle and lower sections - a “honeycomb” pattern), which is detected x-ray.
Characterized by periodically recurring attacks of fatigue, tachycardia, cyanosis, after which after 12-24 hours shortness of breath, pallor, and a painful cough develop, often accompanied by vomiting. In this case, blood is found in the sputum and vomit; in the sputum, in addition, the so-called. cells of heart defects (siderophages).
Acute attacks may be accompanied by abdominal pain, fever, and jaundice.
There is a significant increase in iron content in the blood. Anemia is pronounced (the number of red blood cells in some patients is up to 600-800 thousand in 1 μl). Hypochromia, aniso- and poikilocytosis of erythrocytes, the presence of normoblasts, a large number of reticulocytes, leukocytosis, a shift of the white blood count to the left, and eosinophilia are noted. The myelogram indicates an increase in the erythroid series of hematopoiesis - the leuko-erythroblastic ratio is 1: 2 (normally 3: 1) with the normal process of differentiation and maturation of cells of the myeloid series. Blood bilirubin is slightly increased during a crisis. Dysproteinemia is noted due to an increase in the amount of globulins (beta and gamma). Sometimes there is an enlargement of the liver and spleen. Hematuria, cylindruria, and albuminuria appear. Hypertension is very common.
Bronchoscopy often reveals endobronchitis, indicating inflammatory changes in the bronchi (see Bronchitis). There is a violation of bronchial obstruction.
Clinical manifestations
Post-traumatic hemosiderosis
The spots can be of any size and shape, ranging in color from yellow to brown or black. They occur in any area of the body (even around the eyes), but are more common on the lower extremities ( Fig. 1 ).
Pigmented progressive dermatosis of Schamberg
It appears in the form of points of a red-brown or yellow-brown hue with a diameter of several millimeters, which Shamberg himself compared to ground cayenne pepper grains. These points are most often located on the legs, but can also occur on other parts of the body ( Fig. 2 ). The rashes rise somewhat above the surface of the skin and over time can merge into larger irregularly shaped elements. Gradually they turn pale, and in their place foci of skin atrophy form. There are no subjective sensations; in rare cases, there may be slight itching in the affected area.
Annular telangiectatic purpura of Majocchi
Pinkish or reddish spots of irregular shape with a diameter of one to several centimeters appear on the skin. As they grow, the edges of the spots become darker, and the center, on the contrary, becomes lighter ( Fig. 3 ). Gradually, skin atrophy develops in the central part with loss of small hair. There are no subjective sensations.
Lichenoid purpuric pigmentary dermatitis Gougerot-Blum
It is characterized by the appearance of small lichen-like nodules with small rashes among them. There is a point dilatation of small subcutaneous vessels with local darkening of the skin due to hemosiderosis ( Fig. 4A ). Typical localization is in the lower legs, less often on the hips and torso.
Eczematid-like purpura of Doukas-Kapetanakis
Individual petechiae appear on the skin of the legs with a tendency to unite into large spots. At first they are red, but gradually become yellow or brown, fade and may disappear over time. Sometimes the lesions spread to the thighs, trunk and arms ( Fig. 4B,C ). Additionally, the phenomena of parakeratosis, itching and hyperpigmentation are noted.
In table 1 presents the most common hemosideroses and the main differences between them.
Table 1. Differential diagnosis of the most common hemosiderosis of the skin
| Characteristic | Post-traumatic hemosiderosis | Purpura Majocchi | Schamberg's dermatosis | Gougerot-Blum dermatitis | Doukas-Kapetanakis purpura |
| Floor | In both sexes | Usually in women | Usually in men | Usually in men | In both sexes |
| Frequency of occurrence | Often | Rarely | The most common type of hemosiderosis | Rarely | Moderately often |
| Peak incidence | At any age, but as the body ages, the likelihood increases | Children and youth | Teens and young adults | Middle aged people | Children and youth |
| Dynamics of lesions | Lesions arise at the site of previous injury. More often they occur on the legs due to endocrine pathologies, disorders of the venous system and other factors | Lesions first appear symmetrically on the legs, then can spread to the torso and arms | Lesions most often form symmetrically in the shin area, but can also occur on only one leg. The disease may affect the thighs, buttocks, torso or arms | Most often in the lower legs and very rarely in the thighs and torso | On the legs, gradually moving to the hips, torso and arms |
| Clinical manifestations | Spots of various sizes and shapes, colors ranging from yellow to brown or black | Variable numbers of ring-shaped, erythematous plaques and patches, often with central blanching and atrophy | Isolated red-brown spots that do not protrude above the skin and look like grains of ground cayenne pepper | Tiny lichenoid papules with a tendency to unite into large plaques of varying shades | The lesions are usually extensive. Patients complain of severe itching |
| Histology | Dilation of capillaries in the papillary layer of the dermis, diapedesis, proliferation of capillary endothelium with deposition of hemosiderin in the form of clumps in the interstitial substance, histiocytes, endothelial cells. Slight nonspecific perivascular infiltrate | Perivascular lymphocytic infiltration that extends to the epidermis. Vacuolar changes in the basal layer, spongiosis. Macrophages loaded with hemosiderin are detected, and extravasation of erythrocytes is noted within the lichenoid infiltrate | Perivascular mononuclear infiltration in the upper dermis, swelling of the vascular endothelium. Presence of extravasal erythrocytes and hemosiderin-loaded macrophages | Perivascular lymphocytic infiltration. Lichenoid tissue reaction. Edema of the endothelium and narrowing of the lumen of small vessels | Spongiosis (swelling of the spinous layer of the epidermis) with inflammatory changes |
| Probability of remission | Possible | Possible | Possible | The course is often chronic, but spontaneous remission is possible | Both spontaneous remission and sudden exacerbation of the disease are possible |
| Treatment | Topical corticosteroids, hardware techniques | The disease is congenital and goes away on its own. However, after some time the lesions may appear again | Systemic corticosteroids, antihistamines, vitamin C, PUVA therapy (see below) | Therapy is difficult. Topical and systemic corticosteroids, antihistamines and antipruritics are used. Wearing compression stockings is recommended. Possible use of PUVA therapy (see below), griseofulvin, cyclosporine A, vitamin C and bioflavonoids | Topical corticosteroids and antihistamines |
Rice. 1. Post-traumatic hemosiderosis on the legs (www.healthline.com; Photo: MavCure)
https://i0.wp.com/www.healthline.com
Rice . 2. Chatterjee S. Schamberg disease: uncommon reaction to a common drug. CMAJ 2009; 181(12): E275)
https://www.cmaj.ca
Rice. 3. Annular telangiectatic purpura of Majocchi - in the center of a large lesion, an area of skin lightening is noticeable (Hoesly FJ, et al. Purpura annularis telangiectodes of Majocchi: case report and review of the literature. Int J Dermato 2009; 48(10): 1129–1133)
Rice. 4. Gougerot-Blum dermatitis (A) and Doukas-Kapetanakis purpura (B, C) (Kim DH, et al. Characteristics and clinical manifestations of pigmented purpuric dermatosis. Ann Dermatol 2015; 27: 404–410)
Diagnosis
The diagnosis is made on the basis of a wedge, manifestations of the disease, blood counts, and X-ray data. research, bronchoscopy, detection of macrophages loaded with hemosiderin in sputum and gastric lavage (especially in young children who swallow sputum).
Changes in the lungs with I. g. l. should be differentiated with changes in miliary tuberculosis (see. Respiratory tuberculosis), histoplasmosis (see), pneumomycosis (see), Besnier-Beck-Schaumann disease (see Sarcoidosis).
Hypertension observed with I. g.l. should be distinguished from hypertension with congenital heart defects - patent ductus arteriosus, patent interatrial and interventricular septa with or without the Eisenmenger complex and acquired - mitral stenosis (see Congenital heart defects, Heart defects purchased).
Characteristic for I. g. l. anemia must be differentiated from hemolytic anemia (see), leukemia (see) and other lesions of the hematopoietic system.
Forecast
Sometimes, under the influence of treatment or spontaneously, the condition of patients may improve; remission lasts from several weeks to 5-6 years, then a crisis develops again. With a long course of the disease (2-3 years) and often recurring crises in children, there is a lag in weight and height, deformation of the chest, fingers (“drumsticks”), right ventricular failure develops, the boundaries of the heart expand, chronic pain appears, and pulmonary insufficiency. Most patients die in childhood.
See also Hemosiderosis.
Bibliography:
Hamburg R.L. et al. On the issue of pathogenesis and treatment of idiopathic pulmonary hemosiderosis in children, Vopr. mat. and det., vol. 8, No. I, p. 81, 1963; Dolgoplosk N. A. and Skaldina A. S. A case of essential hemosiderosis of the lungs, Vestn, rentgenol, and radiol., Mb 1, p. 88, 1971, bibliogr.; Kassirsky I. A. and Alekseev G. A. Clinical hematology, M., 1970; Turbina N. S. The use of desferal in the treatment of siderosis of various origins, Problems, hematol, and blood overflow, vol. 13, no. 7, p. 47, 1968, bibliogr.; Fadeeva M. A. et al. Idiopathic hemosiderosis of the lungs in children, Vopr. ocher mat. and children, vol. 21, no. 4, p. 37, 1976, bibliogr.; Khutsishvili G. E. Desferal test in the diagnosis of hemosiderosis in patients with hemoglobinopathies, Laboratory, case, No. 11, p. 660, 1971, bibliogr.; aka, Treatment of hemosiderosis with hemoglobinopathies with desferal, Ter. arkh., t. 43, v. 10, p. 98, 1971, bibliogr.; Blood and its disorders, ed. by R. M. Hardisty a. DJ Weatherall, Oxford, 1974; Mac Donald RA Hemochromatosis and hemosiderosis, Springfield, 1964, bibliogr.; Roberts LN, Montessori G. a. Patterson JG Idiopathic pulmonary hemosiderosis, Amer. Rev. resp. Dis., v. 106, p. 904, 1972.
A. V. Mazurin; V.V. Serov (etiol., pathog., path. an.).
1.General information
In the long list of diagnoses denoting the serious disease considered here, one more is missing - the shortest and, perhaps, the most accurate: “iron lung”. Hemosiderin is a product of hemoglobin breakdown and denaturation of the ferritin protein.
Note that the Greek "sideros" means the same as the Latin "ferrum", that is, iron. Ferritin is a complex protein complex that serves as a “storehouse” for iron in the body. Hemosiderin is a pigment that in large volumes gives the tissues depositing it a characteristic rusty-brown hue, since it contains iron oxide.
The term “hemosiderosis,” according to the canons of word formation in medicine, should mean a clear, pathological excess of hemosiderin; in this case we are talking about its accumulation in the pulmonary parenchymal tissue.
This condition was first described by the outstanding German encyclopedist Rudolf Virchow in 1864, and he also coined the definition of “brown induration of the lungs.” More than a century and a half has passed since then, but researchers still have many questions in connection with this disease. Finding answers and simply establishing the correct diagnosis in this case is very difficult: pulmonary hemosiderosis occurs approximately once per million people, which makes it extremely difficult to develop diagnostic criteria and study pathogenesis, and only in recent years has it begun to be conclusively diagnosed intravitally ( Previously, it was possible to establish an accurate diagnosis mainly through pathological examination).
Hemosiderosis occurs in both sexes and at any age. However, the statistics accumulated to date reveal, according to some sources, a twofold predominance of men among those affected. It is also reported that the disease manifests mainly in childhood and adolescence.
Sign up for a consultation
A must read! Help with hospitalization and treatment!