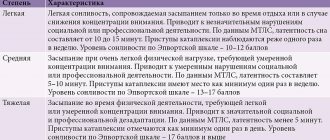
Types of hydrocephalus
There are several variants of the disease depending on the cause of occurrence and localization. By origin, there is a congenital form, which develops as a result of problems suffered by the baby in the prenatal state, and an acquired form, provoked after birth by external factors (injuries, infections).
According to the type of location, they are distinguished:
- external hydrocephalus, when in a child cerebrospinal fluid accumulates mainly in the space under the membranes of the brain;
- internal form, in which cerebrospinal fluid flows into the ventricles of the brain, causing them to expand;
- mixed or general hydrocephalus, which is characterized by a combination of external and internal forms of the disease.
There are also open (communicating) and closed (obstructive) types of pathology: in the first case, the communication between the ventricles and the subarachnoid space is not broken, in the second it is absent. According to the speed of flow, acute, subacute and chronic dropsy of the brain are distinguished.
When is it necessary to “bring down” a child’s high fever?
1. If a child does not feel well, you should not try with all your might to maintain a high temperature. When the baby is capricious, cannot sleep, complains of a headache, body aches, then the temperature can be brought down. Moreover, in different situations and in different children, this condition can occur with different indicators on the thermometer.
2. There is a conditional criterion that the temperature should not be lowered below 38.5°C, and the temperature above this value must be “brought down”. Actually this is not true. Some babies do not tolerate temperatures of 37.5°C. Others feel quite tolerable even at 39°C. It is not so rare that I meet small patients who play calmly at 38.5°C and above.
3. If the baby has chronic diseases. For example: heart disease, metabolic disorders, neurological diseases. In such cases, there is a risk that an increase in temperature will worsen the course of the chronic disease. It is recommended for such children to “bring down” the temperature above 38-38.5°C.
4. Babies under 3 months of age are not recommended to wait until the temperature rises above 38-38.5°C.
5. If the child has previously had febrile seizures (a seizure that occurs in a child only when the child has a high temperature). Meeting such a patient at a pediatrician’s appointment is not uncommon. Usually this condition is benign and goes away on its own with age, without any treatment. It is recommended for such children to reduce their temperature to 38°C. Numerous clinical studies have proven that taking antipyretics prophylactically for such children (i.e., before the temperature begins to rise), repeating them regularly, regardless of the numbers on the thermometer, is not effective. In the same way as treating such babies with antiepileptic drugs.
6. If the temperature is above 41°C. This is the temperature that is considered critical and dangerous for the baby’s internal organs. With common infections, such figures are rare.
Symptoms of hydrocephalus of the brain in a child
Classic signs of hydrocephalus in children over 1–3 years of age are symptoms of increased pressure on the brain, which include:
- intense headache;
- nausea and vomiting;
- spastic paresis, when muscles involuntarily tense and limb movements become sluggish;
- constant fatigue;
- urinary incontinence;
- gait disturbances;
- convulsions;
- strabismus;
- nystagmus;
- developmental delay.
Hydrocephalus, which occurs as a consequence of a brain injury or infection, can cause in an older child a deterioration in memory and attention, decreased visual acuity, irritability, dizziness and head pain that does not go away after taking painkillers.
The following symptoms help to suspect hydrocephalus in infants:
- bulging and pulsation of the fontanel;
- divergence of the sutures of the skull;
- deformation of the head with a predominance of the cerebral region over the facial region;
- rapid increase in head circumference with a significant deviation from the norm;
- increased excitability, moodiness;
- poor appetite;
- frequent volumetric regurgitation, similar to vomiting;
- exotropia;
- Graefe syndrome;
- a distinct pattern of saphenous veins on the head.
In some cases, an additional sign may be a slow heartbeat, tremor (trembling) of the chin and limbs, which persists for a long time.
Diagnostics
Ultrasound examination is a modern and fairly informative method for detecting hydrocephalus in children. Ultrasound is performed in the antenatal clinic to clarify the development of the brain in the fetus. Until the fontanel closes, the presence of hydrocephalus can be determined using neurosonography - ultrasound through the fontanel. The dynamics of head growth in centimeters in the first year of life, despite its simplicity, has not lost its diagnostic significance to this day. CT and MRI are used to diagnose hydrocephalus following an ultrasound scan of the brain. Additional methods to confirm the diagnosis include fundus examination and EEG in the presence of convulsive syndrome.
Reasons for the development of hydrocephalus in children
Factors that can lead to the internal form of the disease are:
- anomalies and malformations of the fetus during the period of intrauterine formation, associated with infections, injuries, and the influence of bad habits of the mother;
- various birth injuries;
- prematurity and premature birth with low body weight.
The causes of acquired hydrocephalus in a child can be infectious diseases of the brain and its structures: meningitis, malignant and benign neoplasms, encephalitis. In some cases, the starting mechanism is traumatic brain injuries and bruises resulting from falls, blows, accidents and other injuries.
Causes of hydrocephalus
Hydrocephalus in the fetus may be associated with problems with the development of the central nervous system, or with intrauterine infection. Therefore, it is so important to undergo a comprehensive examination for various infections - herpes, cytomegalovirus, before planning a pregnancy.
Acquired hydrocephalus in most cases is a consequence or complication of diseases such as:
- Meningitis - viral or bacterial etiology.
- Meningoencephalitis is an inflammatory process that affects the membrane and medulla.
- Subarachnoid hemorrhage is a common consequence of skull trauma or occurs as a consequence of rupture of an arterial aneurysm.
- Sarcoidosis is a granulomatous lesion of the meninges.
- Intraventricular hemorrhage is a consequence of difficult and traumatic obstetric care.
Diagnosis of dropsy of the brain
In infancy, a visual examination is sometimes sufficient to determine the nature of the pathology: the doctor, by examining the baby’s physiological parameters and listening to the parents’ complaints, can make a preliminary diagnosis at the initial appointment.
To clarify the disease in children with an open fontanel, including to identify pathology during intrauterine development, ultrasound is used to assess the degree of enlargement of the ventricles. Additional methods are:
- fluoroscopy;
- computed and magnetic resonance imaging;
- lumbar puncture, necessary for a detailed analysis of the cerebrospinal fluid.
A child with suspected hydrocephalus must be examined by an ophthalmologist or pediatrician; if necessary, concomitant diseases may require consultation with a cardiologist, surgeon, oncologist and other specialists.
Which thermometer is best to use to measure temperature?
There are three types of thermometers used to measure a child's body temperature:
- mercury is the most common thermometer. Its advantage is that such a device measures temperature more accurately than others. The downside is fragility. This is the least preferred way to measure temperature in children. A mercury thermometer is easy to break. The baby may be injured by shrapnel. And mercury is dangerous to health;
- electronic - a simple, modern and convenient thermometer. It is the one that is preferable for children. The downside may be its accuracy. Before using the device for its intended purpose, you should compare its readings with the readings of a mercury thermometer. Take several measurements with both devices on a healthy, adult family member. If the readings differ by no more than 0.1°C, then such a thermometer can be placed in a home medicine cabinet;
- infrared - the advantage of such a thermometer is that it is more accurate than an electronic one. Measures temperature quickly. You don’t need to hold it for a long time, you just need to apply it to the skin for a few seconds. It is very convenient for kids. And also for older children, when you need to measure their temperature while they sleep. The downside is the price - this is the most expensive option. There are different types of infrared thermometers. Some need to be pressed against the skin, others measure temperature at a certain distance from the surface. These thermometers have attachments for measuring temperature in the ear, mouth, and rectum.
For accurate measurements, it is important to use the thermometer correctly. The mercury thermometer must be pressed firmly against the skin. It must be held until the mercury stops rising. Electronic thermometers usually have an audible signal at the end of the measurement. You definitely need to wait for him.
Treatment of hydrocephalus in children
Depending on the type and nature of the pathology, treatment for hydrocele can be conservative or surgical. Conservative tactics are used only in cases with a non-progressive open form of the disease, which is caused by external factors. It involves medication to relieve symptoms and eliminate the cause.
In all other situations, it is rational to use surgical treatment methods, which are aimed primarily at eliminating the obstacle that impedes the outflow of cerebrospinal fluid (tumor, abscess, intracranial hematoma, developmental anomalies). In cases where it is not possible to eliminate the cause of the pathology, a special operation is performed - bypass surgery. The technique involves introducing a system of tubes and valves into the brain, which will drain excess cerebrospinal fluid to other parts of the body.
In situations that threaten the child’s life, when immediate assistance is required, external ventricular drainage is performed - an operation during which excess cerebrospinal fluid is quickly pumped out of the ventricles of the brain using the drainage system.
With timely diagnosis and adequate treatment, a child after hydrocephalus grows and develops in accordance with the norms; the disease does not affect the mental or mental state in any way.
Classification of hydrocephalus
Hydrocephalus can be congenital or acquired. It is generally accepted that the disease is diagnosed in children, but there is an increasing increase in cases of dropsy in adult patients.
According to the nature of the course, hydrocephalus can be:
- Acute - this form of the disease is characterized by a rapid course, the signs become obvious literally within three days.
- Subacute – symptoms increase and develop within one month.
- Chronic – the pathology develops for more than one month.
Disease prevention
The list of measures that can prevent the development of pathology includes:
- pregnancy planning;
- prevention of birth injuries;
- giving up bad habits before conceiving a baby and during pregnancy;
- vaccine prevention of infectious diseases of the brain (meningitis, encephalitis);
- early perinatal diagnosis;
- regular monitoring of children at risk by a pediatrician and neurologist;
- timely completion of preventive examinations up to a year;
- providing the child with safe living conditions to prevent household traumatic brain injuries.
Parents need to closely monitor the development and condition of young children, promptly contacting doctors in case of infectious diseases, falls and injuries affecting the head and neck area.
Specialists at the SM-Doctor clinic will conduct a detailed diagnosis if hydrocephalus is suspected, plan treatment and monitor the child throughout therapy and rehabilitation.
Diagnosis of hydrocephalus
- The main method of examination is an x-ray, the results of which will confirm the dehiscence of the sutures of the skull.
- It is also recommended to do a craniogram - an X-ray examination of the skull in different projections without contrast. Such a diagnosis will not only identify hydrocephalus, but also determine its type in order to prescribe effective therapy as soon as possible.
- Fundoscopy may be required to identify optic disc congestion.
- For differential diagnosis, angiography of cerebral vessels is prescribed.
Get diagnosed with hydrocephalus of the brain at Clinic No. 1
- X-ray
- Craniogram
- Ophthalmoscopy (as prescribed by a doctor)
- Angiography
For one-time payment for services - 20% discount
Call
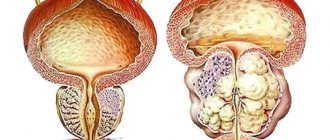
Hydrocephalus
Hydrocephalus (possible synonyms and terminology: “hydrocephalus of the brain”, “hydrocephalus of the brain”, “hydrocephalus of the brain”, “internal hydrocephalus”, “external hydrocephalus”, “hydrocephalus in children”, “replacement hydrocephalus”, “external replacement hydrocephalus” , “mixed hydrocephalus”, “atrophic dropsy”, “large ventricles of the brain”, “brain atrophy”, “multilocunar hydrocephalus”, “brain cysts”, etc.)
We have presented only a small list of synonyms and terms that are found in popular and medical literature, which are identified with hydrocephalus. This once again confirms how many-sided and complex this disease is (developmental defect, brain abnormality). The cornerstone of hydrocephalus is the presence of excess cerebrospinal fluid (CSF) in the brain.
As a rule, hydrocephalus is detected in children. Very high incidence of congenital hydrocephalus, i.e. when the disease is detected during pregnancy (during an ultrasound of the fetus) or immediately after the birth of the child. The average incidence of congenital hydrocele of the brain is on average 1 case per 1000 newborns.
Liquor is a fluid that is formed, circulates and is absorbed in the brain. It is essential for the normal functioning of the brain and spinal cord and is an integral part of the nervous system. But when any disturbances occur in the formation (cerebrospinal fluid production), circulation (cerebrospinal fluid circulation) or absorption (cerebrospinal fluid resorption) of cerebrospinal fluid (CSF), this leads to the development of hydrocephalus.
It is not difficult to guess that an increase (excessive accumulation) of cerebrospinal fluid in the brain leads to disruption of its functioning. First of all, the brain tissue is compressed by the increasing volume of additional fluid. The brain is in a constricted state and begins to shrink (atrophy). The more pronounced the hydrocephalus (for example, with a late visit to a neurosurgeon), the more severely the brain suffers. If the child does not receive adequate treatment and hydrocephalus progresses, it becomes noticeable even during an external examination, as the head circumference begins to increase. The skull bones of a newborn, an infant, or a child under one year old are still quite pliable, so for some time this helps a little. But at the same time, if such a baby is not provided with neurosurgical assistance in a timely manner, then the head circumference can reach catastrophic proportions!
Therefore, it is very important to promptly detect the first symptoms of hydrocephalus, monitor these symptoms, and not miss every little detail.
Symptoms (signs) of hydrocephalus in a child depend on the age and under what clinical circumstances hydrocephalus arose and began to develop. Among the most common symptoms of hydrocephalus are headache, anxiety (or, conversely, drowsiness), vomiting (regurgitation), and a rapid increase in head circumference (usually the frontal region). With long-term observation or at an older age, a lag or delay in the child’s psycho-speech development and behavioral changes will be noticeable. There may be visual disturbances, convulsions, impaired muscle tone, movement disorders, and coordination problems.
Our Perinatal Center sees pregnant women who have been diagnosed with fetal hydrocephalus and/or other brain malformations (often combined with spina bifida, Chiari malformation). Together with the neurosurgeons of our department, strict dynamic monitoring is carried out over the characteristics of the pathological process, the vital activity of the fetus (primarily the state of the brain) and the condition of the mother. The tactics for managing pregnancy and childbirth are determined at a consultation with the participation of Center specialists in each specific case. The first successful intrauterine manipulations for fetal hydrocephalus have already been carried out. And in most cases, a child with hydrocephalus is observed after birth and, if necessary, operated on in the first days of life.
Hydrocephalus often develops in children at an older age. The causes of hydrocephalus are varied. But there are always 3 main mechanisms at the core:
- too much production of cerebrospinal fluid (post-inflammatory hydrocephalus, tumor of the lateral ventricles, choroid plexuses);
- difficulties in the passage of cerebrospinal fluid (impairment or occlusion (blockade) of the transport of cerebrospinal fluid along the cerebrospinal fluid pathways inside the brain and spinal cord). The cause of such hydrocephalus can also be brain tumors, brain cysts, adhesions, congenital absence of holes and channels between the cerebrospinal fluid cavities.
- impaired absorption (resorption) of cerebrospinal fluid. The most common cause of hydrocephalus in young children and congenital hydrocephalus.
All children with hydrocephalus should be consulted by a pediatric neurosurgeon!
If the symptoms of hydrocephalus are not strong, the size of the ventricles of the brain according to ultrasound (CT, MRI) is not so large (mild or moderate internal hydrocephalus, moderate or not expressed mixed hydrocephalus, not expressed external hydrocephalus), the child feels satisfactory, there are no symptoms of intracranial hypertension (increased intracranial pressure), or they are not so pronounced, there is no clear lag in psycho-speech or motor development, then conservative treatment by a neurologist is possible.
In cases where hydrocephalus begins to progress despite conservative treatment, neurosurgical treatment (surgery for hydrocephalus) is necessary.
What methods of surgery do we use for hydrocephalus in children?
Our department uses all currently existing methods of neurosurgical treatment of hydrocephalus in children.
First of all, it is necessary to establish the cause of hydrocephalus and, if possible, eliminate it. That is, we consider the primary task to remove a brain tumor, cyst, excise adhesions, i.e. remove causes that may disrupt the movement of cerebrospinal fluid within the brain. For this purpose, popular endoscopic techniques are used, among other things. They allow you to minimally invasively excise the walls of an arachnoid cyst, remove adhesions inside the ventricles of the brain, create a bypass for the circulation of cerebrospinal fluid, or restore the natural one (for example, eliminate stenosis of the cerebral aqueduct).
Unfortunately, in many cases, a clear cause of hydrocephalus cannot be found, or the cause (the etiology of hydrocephalus) cannot be eliminated surgically (for example, malabsorption of cerebrospinal fluid). Or we know for sure that this will not be effective.
In such cases, various modifications of liquor shunting are used. The most common and effective is ventriculoperitoneostomy - when a child with hydrocephalus is implanted with a special cerebrospinal fluid shunt system, which allows excess fluid to be removed into the peritoneal cavity.
Hydrocephalus - what symptoms should alert you?
Since the disease in most cases develops in the first months of life, doctors carefully monitor the growth rate of the child's head. Excessively rapid enlargement of the head, occurring ahead of the age norm, is an undoubted sign of hydrocephalus ; this in itself is a formidable symptom that requires immediate medical intervention.
At a later age, the bones of the skull lose their plasticity and the disease develops without external visual manifestations. However, the increase in intracranial pressure does not go away, which is manifested by a variety of neurological disorders, such as decreased vision, noise or ringing in the ears, and impaired coordination of movements. Sometimes the disease proceeds covertly, then no obvious symptoms appear, but the child’s mental development still lags behind the age norm, and learning problems appear. There is also an aggressive course, in which case the intracranial pressure rises so much that the eyes seem to protrude from their sockets.
Myths about increased intracranial pressure
The diagnosis of “increased intracranial pressure”, “intracranial hypertension (ICH)” or “hypertensive-hydrocephalic syndrome”, as already mentioned, is often made and in some cases - without reason. How does increased intracranial pressure (ICP) manifest? As already noted, in children under 2 years of age such manifestations are, first of all, accelerated growth of head circumference, bulging and enlarged fontanelle, possible eye movement disorders, and delayed psychomotor development. Most often, all these disorders manifest themselves in a complex. In children over 2 years of age, these are headaches with nausea and vomiting, more often in the morning, changes in the fundus of the eye (detected during examination by an ophthalmologist). Of course, the clinical picture may be different, but without the above symptoms, the diagnosis of “increased intracranial pressure” is doubtful.
This is how pediatrician Evgeniy Komarovsky describes the diagnosis of “increased intracranial pressure.” “Since the main symptom of hydrocephalus is a rapid increase in head size, measuring head circumference is included in the standards of any preventive examination, starting, of course, from the moment of birth. It is very important to emphasize here that it is not the specific size expressed in centimeters that matters, but rather the dynamics of this indicator. That is, stating the fact that the boy Petya at 3 months has a head circumference of as much as 45 cm is not at all a reason to become depressed and urgently save this boy. But the fact that the head circumference has grown by 7 cm over the past month is already alarming and dangerous, and requires both serious attitude and active control. Let me emphasize once again - not immediate treatment, but control. And if the trend continues, then measures should be taken.”
Symptoms such as sleep and behavior disorders, hyperactivity, attention deficit, bad habits, poor academic performance, hypertonicity in the legs, “marble” skin pattern, including on the head, nosebleeds, chin trembling, tiptoe walking, are not in themselves indicate increased intracranial pressure. And yet, some neurologists make a diagnosis of ICH based on these complaints. Neurosonography, having become a huge boon for pediatrics and neurology, has made a significant contribution to the excessive and false diagnosis of “hypertensive-hydrocephalic syndrome.” NSG makes it possible to quickly obtain an image of the brain substance and measure the size of the ventricles. However, to clarify the diagnosis, as we have already said, CT and MRI are mandatory.
Consequences of hydrocephalus
The complications of hydrocephalus are very serious, so treatment should not be delayed. The neuropsychic development of a child, his intelligence, motor skills, vision and even life depend on a correct diagnosis. In many cases, hydrocephalus is the result of a more serious problem, such as a brain tumor.
To prevent the negative consequences of the disease, parents are advised to regularly examine their child with a pediatrician and neurologist. Routine examinations will help identify pathology at an early stage. The Into-Sana clinic employs the best specialists who care about the health of each patient. Here you will receive qualified assistance at the European level.