Intervertebral hernias of the thoracic spine, also called the thoracic spine, are a rather rare occurrence. This is mainly due to low mobility of the thoracic region. Therefore, disc herniations account for no more than 1% of all spinal diseases. But this is precisely where the main danger of this pathology lies. Since it can be accompanied by symptoms similar to the manifestations of cardiovascular diseases, this often leads to an incorrect diagnosis and, accordingly, the prescription of treatment, which will not have any effect on the main cause of the person’s condition, i.e. intervertebral hernia. Thus, time will be lost, the hernia will progress, and the patient’s well-being will deteriorate.
What is an abdominal hernia?
Extension of the internal organs of the abdominal cavity and small pelvis through existing openings beyond their anatomical zone under the general outer covering or into another area is called an abdominal hernia. Unlike prolapse (loss) and eventration (depressurization), a hernial protrusion necessarily consists of three components:
- Gate (exit point).
- Sac (part of the peritoneum).
- Contents (internal organs and structures).
Most often, the hernial sac contains intestinal loops and the greater omentum.
MBST therapy
MBST therapy is an advanced nuclear magnetic resonance technology. It is used for therapeutic purposes for problems with the musculoskeletal system. A similar procedure for thoracic vertebral hernia helps not only to relieve pain, but also to eliminate the need for surgery.
You can sign up for the MBST therapy procedure for the treatment of a herniated thoracic spine at ArthroMedCenter.
Symptoms of thoracic vertebral hernial protrusion are difficult to treat conservatively, especially in the last stages of pathology development. As a consequence, the use of such treatment is advisable only if it was possible to achieve positive results within six months after the start of therapy.
Classification
The classification will help you find out what hernias are:
- by origin - congenital and acquired;
- according to the presence of complications - free, chronically complicated (irreducible) and acutely complicated (strangulated, inflamed, etc.);
- according to the location of the hernial orifice - umbilical, periumbilical, inguinal, femoral, white line of the abdomen, perineal, lumbar, obturator, sciatic, Spigelian line;
- by structure - single- and multi-chamber;
- by quantity - single and numerous.
Only a doctor can accurately determine the type of abdominal hernia.
External
Hernias that come out along with the parietal layer of the peritoneum, as well as through “weak spots” in the muscle-tendon layer of the abdominal walls and pelvic floor, including without damaging the skin, are called external. Hernial orifices can form in natural anatomical areas (femoral ring, Petit's triangle and others) or in areas that have been negatively impacted (after operations, injuries, certain diseases).
Domestic
This type of abdominal hernia is characterized by an internal location. The pathology is localized in the pockets (folds) of the abdominal or thoracic cavity, penetrating through anatomical or acquired defects in the diaphragm.
Congenital
During the prenatal period, for various reasons, the abdominal wall of the abdomen is underdeveloped or its anomalies are formed. This becomes the basis for the formation of pathology.
Purchased
This type of abdominal hernia is formed during a person’s life. Under the influence of numerous factors, a hernial sac appears first. Then, under the influence of increased pressure in the abdominal cavity, internal structures and organs enter it and exit.
Complicated
The danger of such a disease as abdominal hernia (especially irreducible) is that it can suddenly lead to serious complications:
- final uncontrollability;
- inflammation, the “source” of which can be internal or external infectious agents;
- infringement;
- coprostasis;
- damage to the hernial contents (organ rupture, bleeding from an injured vessel, and so on).
Any exacerbation of an abdominal hernia is a reason to urgently seek medical help.
Uncomplicated
A hernia that occurs without complications is a disease that requires dynamic monitoring and treatment by a surgeon. It should be borne in mind that it can change its status at any time and become a complicated pathology.
Diagnosis of thoracic pathology
The disease is diagnosed based on anamnestic data, the results of neurological tests and instrumental methods for examining the thoracic spine. A primary role in diagnosis is played by methods of visualization of the corresponding area of the musculoskeletal system.
Magnetic resonance imaging is recognized as the most accurate method for making a diagnosis. Using MRI, soft paravertebral structures and all components of the spine are visualized layer by layer, including intervertebral discs, spinal cord, and neurovascular formations. Thanks to MRI, the specialist receives the necessary array of information:
- location and direction of the outbreak, its volume;
- the condition of adjacent bone structures, joints and ligaments;
- level of damage to nerve roots, spinal vessels;
- condition of the spinal cord and sagittal size of the spinal canal;
- the presence of concomitant diseases in the area under study (for example, vertebral hemangiomas, spinal cord tumors, neurinoma, spondylosis, etc.).
An example of computed tomography imaging.
If for some reason the patient cannot undergo MRI, he will be recommended the second most diagnostic imaging method - computed tomography. However, although CT visualizes a hernia, it does not have the ability to reliably determine the parameters of the protrusion and the degree of spinal compression. Conventional radiography provides the least information regarding the confirmation and characteristics of the disease, since it allows only the assessment of bone structures, so it is rarely used.
As additional examination methods, the patient may be recommended electroneuromyography (assessment of the bioelectric potentials of skeletal muscles) and myelography (a study with contrast of the cerebrospinal fluid tract). Also, if there is a differential need, the patient may be referred for:
- X-ray or fluorography of the lungs (to exclude/detect pneumonia, pleurisy, pulmonary neoplasms);
- Doppler ultrasound (USDG) of the coronary vessels and ECG (to exclude/detect cardiac pathologies);
- gastroscopy EGDS, ultrasound of the digestive organs (for the purpose of refuting/confirming gastrointestinal diseases);
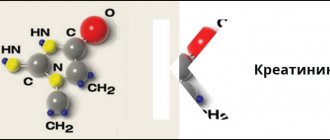
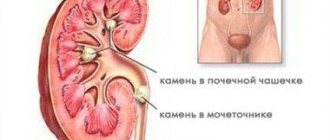
- Ultrasound of the urinary tract and kidneys, urography, urine analysis (to exclude/confirm glomerular nephritis, urolithiasis, pyelonephritis).
Types of abdominal hernia
Depending on the anatomical location, typical (common) types of abdominal hernias and rare forms are distinguished. The most common hernias are:
- inguinal (75%);
- postoperative (12%);
- femoral (8%);
- umbilical (4%).
All other abdominal hernias account for no more than 1% of cases. Females are characterized by femoral and umbilical variants, males - inguinal localization.
Inguinal
There are hernias of the groin area:
- straight (more common in older people, a rounded protrusion is determined near the inguinal ligament);
- oblique (more often diagnosed in children and middle-aged men on one side, usually descending into the scrotum);
- sliding.
In the latter case, one of the walls of the hernial sac is an organ partially covered by the peritoneum (cecum, bladder). As the disease progresses, the function of the latter will suffer, and the person will begin to be bothered by characteristic complaints (constipation, impaired urination, etc.).
Umbilical
Most often, protrusions in the navel area are diagnosed in children, as well as women who are over 40 years old. In children, pathology easily develops due to underdevelopment of the umbilical ring. In women, the provoking factor is stretching of the muscular-connective structures of the abdomen during pregnancy and childbirth. In addition, an embryonic hernia of the umbilical cord is identified, associated with an anomaly of intrauterine development.
Femoral
Due to its anatomical structure, this abdominal hernia occurs much more often in women than in the opposite sex. It is located in the area of the triangle of the same name. Externally, there is a small hemispherical protrusion in the area of the femoral-inguinal flexure.
Hernia of the white line of the abdomen
Between the rectus abdominis muscles, humans have a small strip of tendon called the linea alba. It is in this area that characteristic protrusions appear. In men they occur between the ages of 20 and 40, slightly more often than in women (after 40 years).
Crotch
Hernia formations can be localized in front or behind the intersciatic line. They are observed mainly in women. The hernial sac may include the bladder or genitals.
Lateral
These hernias are formed along the Spigelian line and from the rectus abdominis muscles. They are difficult to differentiate. Often the patient first comes to the doctor with an infringement of the formation.
Prevention
To reduce the likelihood of a hernia forming or reoccurring, it is important to make lifestyle changes. First of all you should:
- stop smoking and minimize the amount of alcohol consumed;
- do exercise therapy and stretching exercises daily;
- undergo a course of manual therapy twice a year;
- avoid stress and change your attitude towards stressful situations;
- sleep at least 7–8 hours;
- wear high-heeled shoes no more than 2 hours a day;
- visit the pool twice a week;
- balance your diet, give up unhealthy foods and adhere to a normal drinking regime (at least 1.5 liters of water per day);
- take vitamins, especially group B and unsaturated fatty acids (Omega-3).
Symptoms and signs
The clinical picture will depend on the location of the protrusion and existing complications. More often, the symptoms of an abdominal hernia will be as follows:
- the presence of education itself;
- pain of varying intensity and character, with possible irradiation and intensification with physical activity, coughing, sneezing, increased gas formation and constipation;
- disruption of the functioning of the organs that make up the contents of the hernial sac.
If complications occur, corresponding symptoms will appear. Sometimes, in addition to physical complaints, patients are concerned about aesthetic discomfort associated with the presence of an external defect. This can trigger emotional problems and depression.
Establishing diagnosis
if the patient’s symptoms indicate the presence of a hernia, an examination, instrumental examination, and the use of a number of diagnostic tests are necessary. An MRI or CT scan of the spine will help you see the full picture of the disease. These methods not only help to visualize the protrusion and its exact location, but also make it possible to assess the condition of the surrounding tissues and the width of the spinal canal. When performing tomography, a specialist can change the step at which the slice is made in order to get into the desired area. In addition, tomography does not harm the body and has virtually no contraindications.
Using computer diagnostics, concomitant pathologies are also identified, which play a role in the further treatment of the hernia. If conventional diagnostics do not provide the necessary information, an examination with a contrast agent may be used. It is rarely prescribed, as it has a number of contraindications and can negatively affect the patient’s health.
Treatment of abdominal hernia
The only method to cure the pathology is surgery. Unreasonable use of a bandage only contributes to injury to the abdominal hernia and the development of complications. The likelihood that a reducible protrusion will become irreducible increases. Wearing a bandage is recommended only for people who have contraindications to surgery. The latter include:
- age up to one year;
- acute infectious processes in the body;
- chronic diseases and infections in the acute stage;
- oncological diagnosis (except for stable remission);
- pathology of the blood system;
- serious diseases in the stage of decompensation (diabetes mellitus, cirrhosis of the liver, etc.);
- recently suffered strokes and heart attacks, other “severe” conditions.
The operation should not be performed on pregnant women.
Surgical intervention
There are many options for surgical techniques for this pathology. If complications occur, emergency intervention is indicated. For uncomplicated abdominal hernias, elective surgery is performed. It includes the following steps:
- dissection of tissue over the hernial formation and the area of the hernial orifice;
- isolation and opening of the hernial sac;
- return of internal organs “to their place”;
- stitching and ligation of the neck of the hernial sac, its removal;
- strengthening the abdominal wall with your own tissues or special means;
- layered sutures.
Surgery can be performed under local or general anesthesia.
Folk remedies
When an abdominal hernia hurts, what to do and what absolutely cannot be done - only a doctor can answer. This disease should not be treated at home using traditional recipes, as there is a high probability of complications arising from this background. Amateur activities are especially dangerous for young children. Methods such as applying a coin to the umbilical hernia in infants and others cannot replace medical consultation.
Massage for some forms of hernia
If a patient has a high probability of developing a hernial protrusion in the abdominal area, therapeutic massage is an excellent means of prevention. Daily tummy massage is recommended for all infants in the absence of medical contraindications. Massage procedures are also recommended for all women after childbirth. They are also prescribed after hernia repair so that the body recovers faster and to prevent relapse. You cannot perform a massage if there is a formed hernial formation without a doctor’s permission.
Causes
Most often, people aged 25–40 years old experience disc herniations in the thoracic or thoracic spine, especially those who spend a lot of time in a sitting position and also regularly experience severe physical activity. Therefore, they are most often diagnosed in professional athletes, welders, seamstresses, office employees, programmers, and drivers.
The main cause of the formation of a hernial defect of the intervertebral disc is osteochondrosis, i.e. degenerative changes in its tissues. This may be a consequence of age-related changes, a sedentary lifestyle, excessive exercise, obesity, autoimmune diseases and a number of other factors.
In any case, the disc, which is a cartilaginous fibrocartilaginous formation, begins to experience increased stress, which leads to disruption of its nutrition and tissue wear. Gradually it becomes dehydrated, becomes thinner and ceases to cope with its natural functions. As a result, the pressure on the vertebrae increases, which causes an increase in pressure inside the disc.
Since its nutrition is disturbed, the fibers that form its outer shell, called the annulus fibrosus, lose their natural elasticity and firmness and micro-tears appear in them under the influence of pressure from the internal contents of the disc (nucleus pulposus). As a result, deformation of the disc shape already occurs, which is called protrusion. In this state, the nucleus pulposus penetrates into the thickness of the fibrous ring. This is accompanied by an inflammatory process and pain.
If at this stage you do not intervene in the pathological process and do not eliminate the destructive factors acting, the disc will continue to deform, since the processes of destruction proceed much faster than regeneration. Ultimately, under the pressure of the nucleus pulposus, the fibrous ring will finally rupture and the contents of the disc will have a free exit into the spinal canal or the anterior part of the spine, which is extremely rare. Thus, posterior or dorsal hernias are formed, which pose a serious threat.
In the absence of treatment, an already formed hernia can enter the final stage of its development, i.e., the prolapsed part of the nucleus pulposus (sequestrum) will separate from it. This is the most dangerous condition, since this piece of cartilage can move freely along the spinal canal, pinching, injuring the spinal roots, descending into the area where the cauda equina passes, and thus provoke irreversible consequences, including complete paralysis.
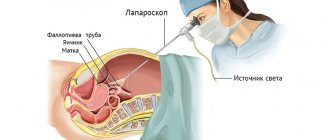
Rehabilitation period
If a hernia in the abdomen was removed laparoscopically as planned, rehabilitation will be much easier and faster than after abdominal surgery for a complication caused by it. Therefore, surgeons insist that there is no point in delaying the operation if there are direct indications for it.
After surgical treatment, the patient remains in the ward for several hours or days, under the supervision of medical personnel. He is then discharged home. Further rehabilitation includes:
- walking and physical activity comparable to the intervention;
- nutritious food with enough fluids;
- body weight control;
- walks in the fresh air three days after surgery;
- mandatory dressings;
- taking medications prescribed by a doctor (antibiotics, laxatives, etc.);
- wearing special postoperative underwear;
- You should not bend forward, do gymnastics, lift weights and provoke an increase in intra-abdominal pressure.
To prevent relapses, even after final recovery, it is advisable to adhere to these recommendations.
Who will treat you?
The Innovative Medical Center employs doctors of the highest category, doctors and candidates of medical sciences, who have accumulated extensive experience in the treatment of intervertebral hernias and have already helped many patients:
Bogdanov Vadim Yuryevich – chief physician, orthopedist-traumatologist. Completed internships in Germany to perform complex arthroscopic interventions, successful experience in performing thousands of operations. Read more about the doctor.
Ronami Valery Guseinovich is a professor, doctor of medical sciences, neurologist, reflexologist and chiropractor with 40 years of experience. Read more about the doctor.