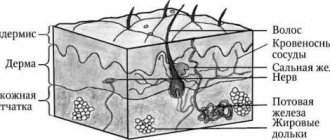
Skin weighs up to 15% of body weight.
It is the largest organ on which many neoplasms arise and disappear. People are especially familiar with nevi. This is what doctors call them, and the name mole has taken root in colloquial speech.
What it is?
A nevus is a benign formation of melanocyte cells, usually dark and smooth. Most people have between 10 and 40 moles nestled on their skin. Some appear at birth. The rest - throughout life. During puberty, old nevi enlarge and darken, and they also grow due to exposure to the sun. The more often a person sunbathes, the more moles decorate him. Or it doesn’t decorate, depending on your luck.
Nevi often change. For example, they turn into flabby and soft new growths, or vice versa - into dense and colorless ones.
There are many types of moles: complex, transitional, borderline, non-pigmented, epidermal. Some are harmless. Others are more dangerous and can develop into malignant tumors. A doctor should regularly examine complex nevi to prevent their transformation.
Make an appointment with a dermatologist
Other types of moles also have their own characteristics.
Types of nevi
Doctors classify moles by location, pigmentation and other characteristics.
Main types of nevi:
- Congenital
These are moles you were born with. They come in small, medium or giant sizes with different colors and shapes. Some nevi in newborns cover large areas of skin and often develop into cancerous formations.
- Regular
Smooth one-color moles. Sometimes they appear at birth, but mostly grow out during adolescence. Common colors are brown and pink. The surface is flat or dome-shaped.
- Dysplastic or atypical
Non-standard moles, of which there are not very many on the skin - fewer than ordinary nevi . May develop into melanoma . The skin on moles can be multi-colored, and the edges of the new growths are asymmetrical with unclear boundaries. Dysplastic nevi often degenerate into melanoma. The more there are, the higher the risk.
- Blue
Blue moles can be congenital or acquired. The shade of the new growths ranges from gray to black, but they are always clearly distinguishable due to their blue color. Most cases of these nevi occur in people of Asian descent. For others - rarely.
- Miescher's nevi
Brown or flesh-colored growths on the neck or face. Smooth and hard dome-shaped moles from which hair often grows.
- Nevi of Unna
Soft brown moles similar to Miescher nevi. They appear mainly on the arms and neck, and their texture resembles raspberries.
- Meyerson's nevi
Eczema surrounds the moles, which causes a red rash. Such tumors grow even in patients without eczema. Mainly found in men. In women - 3 times less often. Most Meyerson nevi form in people over 30 years of age.
- Halo nevi
Moles are surrounded by a pale ring. They do not remain until the end of their lives - first they acquire a pink color, then completely disappear. Sometimes new white rings appear around the growths.
- Spitz nevi
Raised dome-shaped moles. Such pink neoplasms mainly grow at a young age - up to 20 years. Sometimes they have a different color. Some nevi bleed and are difficult to distinguish from malignant tumors.
- Reed nevi
Black or dark brown raised growths that grow very quickly. Therefore, doctors often confuse them with melanoma, but these moles are not dangerous. Occurs mainly in women.
- Agminated
Clusters of similar moles on a small area of skin. They are not the same - one group may consist of smooth nevi, the other of dome-shaped ones.
As you can see, dermatologists have managed to identify many types of moles. We haven't listed everything, just the main ones. Doctors perform dermatoscopy of the nevus to determine its species. A typical example is papillomatous nevus.
How dangerous are dysplastic nevi?
There are specific, proven figures here that it would be better for those who spread hysteria on the “Internet” to become familiar with.
- The annual risk of a dysplastic nevus turning into melanoma is 1 in 10,000. According to the authors [4], this is very low.
- About 70% of melanomas develop not against the background of nevi, but against the background of unchanged skin [5].
- A study examining the genetic profile of atypical nevi has challenged the hypothesis that they are precursors to melanoma [6].
- In two studies, the authors followed patients with incompletely removed, histologically confirmed dysplastic nevi for a long time (up to 17 years) [8,9]. Based on this, the very thesis about the increased risk of developing melanoma from a dysplastic nevus can be seriously questioned.
What is papillomatous nevus
Not all skin growths are moles. There are also warts, condylomas and papillomas, which are sometimes difficult to distinguish from nevi. It is especially difficult with papillomatous pigmented nevus .
It looks like a regular papilloma.
But in fact, this is a convex, bumpy mole - a benign formation that never turns into cancer. Usually a nevus is flesh-colored, brown or brown. Black is rare.
Most interdermal pigmented nevi grow hair and form on the head or neck. In rare cases - in other areas.
Such moles appear at any period of life: at birth, in adolescence, in old age. At first they are invisible. However, nevi continually grow and soon begin to interfere. If they appear among the hair on the head, then combing can damage them. Inflammation will begin. Moles constantly hurt, and the skin around them turns red.
A papillomatous nevus on the face is a serious cosmetic defect, because it constantly grows and is striking.
People with such moles often want to have them removed. But we recommend making a decision only after consulting a dermatologist and checking the tumor for the risk of degeneration. This nevus is similar to papillomas. Without the help of a doctor, you will not be able to determine how dangerous a mole is.
Usually, a dermatologist prescribes surgery if the nevus is constantly injured and inflamed or spoils the patient’s appearance. Before surgery, the doctor must rule out the possibility of melanoma. He performs a dermatoscopy of the mole.
Papillomatous nevus is removed using different methods:
- Laser
- Cryodestruction
- Radio wave surgery
- Electrocoagulation
- Surgical excision
A common method for removing tumors on the face and neck is laser.
Diagnostics
It is necessary to diagnose melanoma in time and determine the stage of its development in order for the treatment of the disease to be successful.
First, an anamnesis is collected, the doctor learns about changes in the nevus.
Do not take a biopsy or expose the mole to chemical and electrical effects unnecessarily.
To diagnose you need to do:
- Histological examination (a superficial smear is taken if there is bleeding or cracks, provided that the tumor is removed immediately after the diagnostic results);
- Epiluminescent microscopy (examination of a mole using a special apparatus to determine its structure);
- CT (image recording, data processing, comparison with standards).
Intradermal nevus
This is another name for common moles - dome-shaped nevi.
We have already mentioned that such neoplasms rarely grow in children - only in every hundred, while in adults they pop up in dozens.
Why are they called that?
Intradermal - moles under the top layer of skin. Therefore, their color does not differ from the color of the surrounding skin and they are noticeable due to their height.
Intradermal nevi grow everywhere. Most often they appear on the neck, head, upper arms and even on the eyelids.
Most moles are small - from 5 mm to 1 cm, and are hardly noticeable in children. As you grow older, nevi change. They become more convex and darker. In people over 70 years of age, intradermal nevi, on the contrary, become discolored and are almost invisible.
Why do common moles appear?
Such neoplasms arise for 3 main reasons:
- Heredity
If parents have more than 50 moles, then the child is likely to get many nevi.
- Sun exposure
When the sun damages skin, especially light skin, moles often appear.
- Immunosuppressive treatments
Some drugs reduce immunity, which causes new nevi to form.
Should intradermal moles be checked?
We recommend checking any nevi regularly. At least once a year. See a dermatologist outside of your regular schedule if the growths have changed color, shape, or size.
The main reasons for removing a mole:
- Degenerates into melanoma
- Gets damaged on clothes every day
- Looks disgusting
The nevus is easily removed. Doctors even remove tumors on the face or neck with laser or other methods.
Symptoms of nevus
Nevi are the result of the accumulation of neocyte cells in one place. They are mutated melanocytes: sources of melanin, which colors human skin. Nevi are located on the face, body, head, arms and legs from birth. Over the course of life, their number increases. The opposite cases have also been recorded - a decrease or disappearance of atypical pigmentation on the human body.
The International Classification of Diseases (ICD) includes three main categories of disease:
- melanoform nevus;
- non-tumor nevus;
- non-tumor congenital nevus.
Benign formations are distinguished by a variety of locations on the human body, shape and size. The surface of pigmented nevi is formed flat or voluminous, similar to a wart, with or without hair. The category of small clusters of nevocytes includes those that have a diameter of 0.5 to 1.5 mm. Medium nevi have a diameter of up to 10 mm, the rest belong to the large category. Giant nevi include formations that cover large areas: cheeks, legs, forearms, back, etc. The color of the formations remains different: black, red, brown, purple, gray.
Epidermal nevus
This type of neoplasm grows from cells in the outer layer of the skin. Up to half of epidermal moles appear at birth, the rest - in the first year of life. After that they don't change.
Varieties of epidermal nevus differ in the type of cells they are composed of. The outer layer of the skin, or epidermis, is made up of keratinocyte cells.
A separate group of moles is keratinocyte or non-organoid. It includes neoplasms that consist of keratinocytes and grow on the trunk or limbs. Never on the head. Nevi can be flat or raised. As a person gets older, moles thicken and darken.
Another group of epidermal nevi is organoid. These moles are not only made up of keratinocytes, but also cells that form sweat glands. Yellow-orange neoplasms. They grow exclusively on the face and head, making it appear that a person is bald. Like non-organoid nevi, these moles gradually become denser. A quarter of nevi cause the development of malignant tumors.
Typically, people develop one or more moles of varying sizes and shapes. Less often - more. According to studies, out of 1000 people, no more than 3 will become carriers of epidermal nevus.
diagnosis of pigmented nevus
- Finding out the history of the disease and visual examination of the pigment spot allows you to obtain up to 50% of the information.
- Dermatoscopy is performed in most developed clinics. The essence of the study is to view the nevus under a fluorescent microscope. Using this method, you can evaluate the surface of the nevus, the presence of microcracks, the color of individual parts, the condition of nearby skin, signs of inflammation, and more.
- Computer diagnostics of pigment spots is an expensive procedure and is not carried out everywhere. With its help, the diagnosis of one or another type of nevus is made with up to 90% confidence.
- A nevus biopsy is performed as a last resort and according to strict indications. It is better to carry out a targeted biopsy of an already removed formation followed by histological examination. This type of diagnosis is the most accurate.
What is an apigmented nevus?
Most moles have a characteristic color: from pink to black.
There are exceptions.
Pigmentless nevi have almost no pigment cells and appear as light or whitish spots of irregular shape. Moles appear in childhood and remain with a person for life. However, not everyone has them. Mostly such neoplasms settle on the skin of representatives of the Caucasian race.
The size of the nevus does not exceed 2 cm. In most cases, only moles on the face are removed if they spoil the appearance. This happens quite often.
That's why.
Unlike other neoplasms, non-pigmented nevi do not darken due to the sun. Against the background of tanned skin, they are striking, which for many people is a good reason for removing moles.
However, the chance of their appearance is small - only 1%.
What to do? Should I delete or not?
Fortunately, I was not able to find practical recommendations in which the mere presence of an atypical nevus on a person’s skin would be considered a direct indication for its removal.
On the other hand, the presence of single or multiple, atypical [7] and dysplastic [3] nevi on a person’s skin equally increases the risk of developing melanoma on the skin as a whole.
Thus, in my opinion, the most logical tactic seems to be not prophylactic removal of atypical nevi, but increasing the frequency of preventive self-examinations and examinations by an oncologist.
Borderline nevus
A type of mole that often turns into a malignant formation. They need to be checked regularly.
A borderline nevus grows under the stratum corneum of the skin and looks like a uniform brown spot. It has different shades: from light to dark. Not much different from a regular mole - the same round or oval shape, clear boundaries.
The following signs indicate degeneration:
- The tumor increases in size
- Nevus darkens or brightens
- Pigment spots appear near the mole
- The neoplasm becomes denser
- There is itching or pain in the mole
Contact a dermatologist if any of these symptoms appear - he will examine the moles and, if necessary, refer you to an oncologist.
You also need to be careful about giant tumors.
Melanocytic nevi
The article presents options, clinical manifestations, clinical features, and diagnostic criteria for various types of melanocytic nevi.
The increased attention of doctors of all specialties to melanocytic nevi (MN) is explained by late diagnosis and poor prognosis of melanoma developing against them - one of the most malignant human tumors. Making up less than 10% of the structure of malignant skin neoplasms (MSN), melanoma is responsible for 80% of deaths in the entire group of MNS /1/. On the other hand, timely treatment of melanoma (at the stage of “horizontal” growth) allows patients to achieve a 10-year disease-free period of life in 90% of cases /7/.
It is known that melanoma occurs in approximately 50% of cases against the background of MN, which may be due to a common genetic defect - loss of heterozygosity in the 9p21 locus of chromosome /16/ with a mutation in the nRAS oncogene /20/ in both melanoma tissue and MN, against the background which it developed.
The most important factor in the development of melanoma against the background of MN is exposure of human skin to an excessive dose of UVR, which leads not only to damage to keratinocytes and melanocytes, but also to immunosuppression, caused primarily by the suppression of NK cells. In addition, risk factors for the development of melanoma are: skin phenotype I-II (proneness to sunburn of the skin, red hair, blue eyes, fair skin), 3 or more episodes of sunburn of the skin during life, the presence of freckles and lentigo or 3 or more atypical MN, familial cases of melanoma in close relatives /1/.
MNs are observed in ¾ of Caucasians /18/ and are benign tumors of the melanogenic system. Only some of them transform into melanoma (melanoma-dangerous MN) or are a marker of an increased risk of its development. /4,11,12,19/. Identifying them in order to prevent the development of melanoma is extremely important for doctors of all specialties.
The vast majority of MNs are acquired. They are divided into regular and special types.
Among common MNs, borderline, complex (epidermal-dermal) and intradermal forms are distinguished /15)/. They arise after the birth of a child and have characteristic dynamics: first, due to the proliferation of nevus cells along the border of the epidermis and dermis, the formation of borderline MN occurs; over time, nevus cells move into the dermis, forming mixed MN; the borderline component may disappear with age, leaving only the dermal (intradermal MN) component /3, 5, 6, 9/. The evolution of MN is associated with the phases of melanocyte involution: melanocyte - nevus cell - fibrous tissue /10/.
Clinically, borderline MN is manifested by a uniformly pigmented (from light brown to dark brown) spot with a diameter of 1-5 mm, round or oval in shape with a smooth surface and clear boundaries, located on any part of the skin and existing until approximately 35 years of age. Mixed MN is a pigmented papule, sometimes with papillomatosis, rarely reaching 1 cm in diameter. Intradermal MN is characterized by a dome-shaped or papillomatous papule, which in shape can resemble a blackberry (Fig. 1.), have a stalk or the shape of a mollusc-shaped element on a broad base (Fig. 2); its surface is covered with hair, its diameter rarely exceeds 1 cm, and its color varies from light brown to black. Rarely, depigmented MN with a whitish or pink-red color is found.
Rice. 1. Intradermal melanocytic nevus in the form of a blackberry.
Rice. 2. Intradermal melanocytic nevus mollusciform.
The dependence of the clinical picture of ordinary MNs on the localization and location of nevus cells in them was noted. Thus, on the palms and soles, the complex and intradermal MN (due to the large thickness of the stratum corneum) do not rise above the skin level; MNs raised above the skin level have a pronounced intradermal nevus component, and flat ones have a borderline component; The more the MN is raised above the skin level, the less pigmented it is.
Conventional MNs grow in proportion to the growth of the human body; after birth, their number increases, reaching a maximum during puberty, and after 50 years it gradually decreases, and by 7-9 decades of life they usually disappear. The regression of conventional MN is due to the degeneration of the cells that form it with their gradual replacement by fibrous and adipose tissue /10,24/. Sudden regression of such MNs occurs very rarely /29/.
The idea that melanoma-dangerous MN should include borderline and mixed forms (as those that retain a borderline component in their structure, including those localized in the area of the palms and soles, external genitalia, and nail bed) has now been revised. Thus, MN of the palms and soles, accounting for 4-9% of all MN, is currently not classified as melanoma-dangerous due to the fact that only dysplastic nevi of this localization transform into melanoma /17/. MN of the nail bed, the so-called longitudinal (linear) melanonychia in the form of pigmented lines running along the nail plate, can be not only borderline, mixed MN or acral-lentiginous melanoma, but also, often, the so-called “melanotic spot” (formed by increased melanin content in the cells of the basal layer of the epidermis without increasing the number of melanocytes) / 28 /. Although subungual melanoma occurs not only in adults but also in children, longitudinal melanonychia in children is almost always a benign process /21/.
Conventional MNs of the external genitalia are more often observed in young women in the area of the vulva and perineum, less often in the area of the male genital organs, but atypical histological signs are found in them extremely rarely (in 0.02% of cases) /27/. On the other hand, convincing evidence has been obtained that melanoma can develop both in the tissue of the intradermal MN and directly beneath it /30/.
Due to the possibility of developing melanoma against the background of intradermal MN, as well as due to the difficulty of clinically distinguishing borderline and mixed MN from dysplastic nevus, in order to avoid malignancy in ordinary MN, they should not be subjected to constant friction with clothing, contact with irritating substances, and mechanical hair removal from them is unacceptable. surface /25/.
Melanoma-dangerous MNs include congenital and dysplastic nevi. Congenital MN are benign pigmented tumors consisting of nevus melanoblast-derived cells. arising as a result of impaired differentiation of melanoblasts in the period between 10 weeks and 6 months of intrauterine life. They occur in 1% of Caucasian children, are detected at birth or during the first year of a child's life and come in different sizes: from tiny to gigantic. Any of them can develop melanoma. Clinically, they are light or dark brown in color, slightly raised above the skin level and sometimes covered with hair (hair growth does not begin immediately), and have a round or oval shape. Their boundaries are clear or blurred, the shape is regular or irregular, the surface has a preserved skin pattern or is bumpy, wrinkled, folded, lobulated, covered with papillae resembling cerebral convolutions (loss of skin pattern occurs when the reticular layer of the dermis is involved in the pathological process (blue congenital MN), color - light or dark brown. They are localized on any part of the skin and in 5% of cases they are multiple (in this case, one of them is large). Larger nevi have a soft consistency when palpated.
Congenital MNs can be small (up to 1.5 cm), large (up to 20 cm) and giant. Congenital MNs are practically indistinguishable from acquired conventional MNs, the only difference is a diameter of more than 1.5 cm (acquired MNs do not have such a diameter), therefore, it is currently proposed that MNs with a diameter of more than 1.5 cm be regarded as congenital MN or dysplastic nevus /2/. Large and giant congenital MNs, in contrast to small congenital MNs, which are solitary in 95% of cases, are usually represented by large or very large MNs, occupying part or all of the anatomical region (trunk, limb, head and neck), but in combination with many small ones MN (Fig. 3).
Rice. 3. Congenital melanocytic nevus.
In this case, nevus cells form ordered accumulations in the epidermis and dermis in the form of layers, nests or strands. The presence of nevus cells in the lower third of the reticular layer of the dermis or in the subcutaneous tissue indicates the congenital nature of MN /19/ Nevus cells are found, in contrast to acquired MN, also in the appendages of the skin, bundles of nerve fibers, muscles that raise the hair, in the walls of the blood and lymphatics vessels. In large and giant congenital MNs, nevus cells sometimes penetrate muscles, bones, and dura mater.
Unlike acquired MNs, congenital MNs do not disappear spontaneously. The risk of developing melanoma against the background of small congenital nevi is 1-5%, giant ones - 6.3% (and in 50% of cases, melanomas develop at the age of 3-5 years). The prognosis for melanoma growing from a large congenital MN is always unfavorable, since it is usually detected in the later stages of development.
Dysplastic nevus (DN) (syn.: Clark's nevus, atypical nevus) is an acquired pigmented neoplasm, characterized histologically by random proliferation of atypical melanocytes. It occurs in 5% of the population /8/ (including 30-50% of patients with sporadic and all patients with familial melanoma) and occurs on clinically unaffected skin or against the background of complex or (rarely) borderline MN. DNs appear later than acquired MNs—shortly before the onset of puberty or throughout life until old age. Their development is promoted by insolation. They are not characterized by spontaneous involution. DN can be sporadic (30-50% of cases) or hereditary, transmitted in an autosomal dominant manner (DN syndrome or familial atypical MN syndrome). DN syndrome and familial melanoma are caused by mutations of various genes, most often localized in chromosome segments 1p36 and 9p21 /19/. Clones of mutant melanocytes can be activated under the influence of photons from sunlight.
DN occupies an intermediate position between acquired MN and superficially spreading melanoma /2/ and is clinically manifested as: a spot with individual areas raised above the skin level (papule against the background of the spot), large (more than 15 mm in diameter) in size, uneven (motley, reminiscent of scrambled eggs - fried egg or target) coloring, asymmetry, irregular borders (the edges are partly fuzzy, uneven) (Fig. 4).
Rice. 4. Dysplastic nevus
Located mainly on the torso and limbs. Transformation of DN into superficial spreading melanoma occurs in 18-35% of cases /2.9/. The risk of developing melanoma in DN in persons with immunosuppression (organ transplant recipients, etc.) increases significantly, and in DN syndrome transformation into melanoma occurs in 100% of cases. It is estimated that in the presence of one DN, the likelihood of developing melanoma increases by 2 times, compared with cases where it is absent, and in the presence of 10 or more - by 12 times /2/. The risk of malignant transformation is especially high if a relative has more than 100 elements of DN or melanoma.
Histologically, DN is characterized by: hyperplasia and proliferation of melanocytes, which in the form of spindle-shaped cells are located in a single row along the basal layer of the epidermis (lentiginous melanocytic dysplasia) or in the form of epithelioid cells form scattered nests of irregular shape (epithelioid cell melanocytic dysplasia); atypical melanocytes (large cell size, polymorphism of cells and their nuclei, nuclear hyperchromasia); Nests of melanocytes are also characteristic: scattered, irregular in shape, forming “bridges” between the interpapillary processes of the epidermis; spindle-shaped melanocytes are oriented parallel to the skin surface; there is a proliferation of collagen fibers in the dermal papillae and fibrosis (a variable sign) / 19 /.
In connection with the problem of melanoma formation in melanoma-dangerous MN, it is important to take into account that its cytological diagnosis is not sufficiently reliable, therefore, for the purpose of diagnosis and differential diagnosis, a diagnostic biopsy of the neoplasm is performed.
Excisional biopsy for the purpose of histological examination, a reliable method for detecting melanoma, is safe and recommended for MNs less than 1.5 cm in diameter and carried out 2 mm from its edge /4.12/.
An incisional (partial) biopsy is performed by an oncologist for very large (congenital) MNs /4/. In particular, with the sudden appearance of longitudinal melanonychia, to exclude acral-lentiginous melanoma or Bowen's disease of the nail matrix (also causing longitudinal melanonychia), a biopsy is performed with a 3-4 mm punch (through the nail plate and matrix to the phalangeal bone) /26/.
Superficial biopsy (“cutting”, curettage, etc.) is unacceptable, because does not make it possible to determine the depth of tumor invasion /19/.
Differential diagnosis of MN with various dermatoses and skin neoplasms is presented in Table 1.
Table 1.
To the differential diagnosis of melanocytic nevus
| Form MN | Dermatosis/skin tumor |
| Border | Freckles, lentigo simplex, lentigo solar (senile), café au lait spots, congenital MN, macular nevus, xeroderma pigmentosum, dysplastic nevus, Dubreuil's melanosis. |
| Mixed | Seborrheic keratosis, Kaposi's sarcoma |
| Intradermal | Dermatofibroma, wart vulgaris, trichoepithelioma, juvenile xanthoma, syringoma, molluscum contagiosum, accessory nipple, pyogenic granuloma, neurofibroma, acrochordon, cystic basal cell carcinoma |
| Congenital | Dysplastic nevus, blue nevus, Becker's nevus, verrucous epidermal nevus, café au lait spots |
| Dysplastic nevus | Congenital MN, Dubreuil's melanosis, Spitz nevus, pigmented basal cell carcinoma |
The differential diagnosis of MN with Dubreuil's precancerous limited melanosis and some forms of melanoma should be discussed in more detail.
Precancerous melanosis limited by Dubreuil (syn.: Hutchinson's melanotic freckle), in contrast to intradermal MN, has a larger (over 20 mm) diameter, irregular outline, uneven pigmentation; it occurs on exposed areas of the skin (usually on the cheeks in older people) and is characterized by slow progression to melanoma; Histological examination reveals the structure of melanoma in situ.
Acral-lentiginous melanoma, in contrast to intradermal MN, is characterized by a brown or black plaque with unclear contours and uneven coloring /2/.
Desmoplastic (amelanotic) melanoma, in contrast to intradermal MN, looks like a non-pigmented spot or papule, reminiscent of a scar or scar, and in the “vertical growth” phase it is characterized by a dense node, most often developing in the head and neck area in people of the 6th-7th decade life, may occur in association with acral-lentiginous melanoma or de novo /14/; microscopically consists of spindle-shaped cells located between thin layers of collagen, which are often formed into bundles.
Differential diagnosis of intradermal MN with superficial spreading and nodular forms of melanoma is carried out according to the “FIGARO” rule:
F - shape. Melanoma is characterized by a convex shape (which is best seen in side lighting). Melanoma in situ and acral lentiginous melanoma are flat.
And - change in size. Accelerated growth is one of the most important signs of melanoma.
G - the boundaries are incorrect. The tumor has “ragged” edges.
A- asymmetry - one half of the tumor is not similar to the other.
P - large sizes (usually more than 6 cm)
O- the color is uneven - randomly scattered brown, black, gray, pink and white areas /9/.
Dark brown and black MNs in people with fair skin color should be considered the most suspicious for melanoma. You should also be suspicious of MN with bluish, reddish and white areas on the surface. However, changes in the color of MN may be due to factors not related to its malignant transformation: pregnancy, puberty, taking glucocorticoid hormones, exposure to external factors, including solar radiation. In such cases, all MNs or MNs of the same localization that were affected by external factors change simultaneously. Only changes in a single MN require oncological alertness.
When collecting anamnesis, the dermatologist must exclude other causes of sudden changes in MN that are not related to its transformation into melanoma. Thus, a sudden change in color, surface or size in the presence of pain, itching, ulceration and bleeding can be caused by the formation of a cystic enlargement of the hair follicle, an epidermal cyst in the MN, the development of folliculitis in it, as well as trauma, hemorrhage, compression or thrombosis of skin vessels. With such changes, dynamic observation is required with serial photography of the elements until the effects of injury or inflammation pass (usually 7-10 days), and in some cases a histological examination is required.
Among the instrumental methods for excluding melanoma, epiluminescence microscopy is currently used - a non-invasive method for studying skin formations in a special immersion environment using a dermatoscope, as well as a computer diagnostic method in which images recorded using a digital video camera are stored in computer memory and compared with the existing one based on certain characteristics. database /1/.
The accuracy of histological diagnosis of melanogenic skin tumors increases when using the “diagnostic ploidometry” method /10/.
Treatment tactics
Although in the vast majority of cases acquired MN do not require treatment, it is still undertaken in some conditions.
Indications for excision of conventional MNs may include:
- the patient’s desire to remove it for cosmetic reasons, however, it should be taken into account that histological preparations of “disfiguring MN” often reveal atypical cells /25/;
- location in places difficult for self-control (scalp, perineum, etc.), this primarily applies to hyperpigmented MN and if there is a personal or family history of DN;
— presence of signs of atypia in the MN: uneven distribution of pigment, jagged and unclear boundaries, relatively large size (more than 5 mm);
- atypical evolution of MN, including a sudden change in size and shape /13/;
— MN with a high risk of malignancy (lentigo maligna, giant congenital MN); DN, including as part of spotted MN; prophylactic removal prevents the possibility of melanoma even with a significant number of MNs /25/;
- although the features of the anatomical location are not considered as an indication for removal of MNs, nevertheless, intensely pigmented MNs of acral localization in the extremities, as well as on the mucous membrane, should be removed, as well as MNs of the subungual region and conjunctiva, since the possibility of DN of such localization should cause caution regarding its transformation into melanoma /22/.
If the element is frequently repeatedly irritated, it is better to remove it than to miss melanoma or other malignant tumor /11/; at the same time, MNs located under a belt, bra, or collar do not have to be removed if they look benign /25/;
Based on this, the MN can be surgically removed in case of: rapid change in the element, atypical clinical picture, suspicious for melanoma, for cosmetic reasons, repeated injury to the element /13/.
The indication for immediate excision of the MN is the presence of at least one of 7 signs of its sudden (within one or several months) change:
- increasing the area and height of the element;
- increasing the intensity of pigmentation, especially if it is uneven;
- signs of local regression;
- the appearance of a pigment corolla around the MN, the appearance of satellite elements;
- inflammatory reaction in the MN;
- itching;
- erosion and bleeding.
Removal of MN must be complete and performed surgically with mandatory histological examination. After partial removal, the MN repigments and recurs, forming pseudomelanoma /23/. Other removal methods (electrocoagulation, cryodestruction, dermabrasion, laser) for pigmented formations of the skin and mucous membranes should not be performed, because do not provide documentary verification of the diagnosis /12/.
When starting treatment for MN, it should be taken into account that with its non-radical removal, the cosmetic outcome is often unpredictable, because treatment may lead to relapse with less favorable consequences than before treatment /25/.
All small congenital MNs that look unusual (uneven coloring, irregular outline, etc.) are subject to surgical removal before the patient reaches the age of 12 years. Giant congenital MN is removed as early as possible. Full-thickness skin flaps are used to close the defect. For large sizes, they resort to expander plastic or plastic with local tissues.
Treatment of DN should be carried out by an oncologist.
Prevention of melanoma consists of early and active detection of pre-melanoma lesions (primarily DN and lentigo maligna), the need to allocate patients with their presence to a “risk group” with constant dynamic monitoring of macroscopic changes in these spots.
Patients with DN should be informed about the signs of transformation of these MNs into melanoma and independently regularly monitor the nature of individual elements. They are advised to avoid exposure to the sun and use sunscreen (Anthelios XL60+) when going outside.
V.A. Molochkov
Moscow Regional Research Clinical Institute named after M.F. Vladimirsky)
Molochkov Vladimir Alekseevich - Doctor of Medical Sciences, Professor, Head of the Clinic of Dermatovenereology and Dermato-Oncology
Literature:
1. Demidov L.V., Kharkevich G.Yu. Markina I.T. and others. Melanoma and other malignant neoplasms of the skin/Encyclopedia of Clinical Oncology. Guide for practitioners / M.I. Davydov et al. - M.: RLS-2005.-P.341-364;
2. Borisova G.N., Kudryavtseva G.T. //Vestn. dermatol.-2006.-No.3.-P.43-45;
3. Dermato-oncology /Ed. G.A. Galil-ogly and others - Medicine for all - 2005;
4. Makin I.L.. Pshenistov K.P. Selected issues of plastic surgery-1999.-No. 1-Yaroslavl-DIA-press;
5. Molochkov V.A. //Aesthetic Medicine-2005.-No. 3-P.266-270;
6. Molochkov V.A. //Russian Journal of Skin and Venereal Diseases-1998.-No.2.-P.68-76;
7. Organizational technology of interaction between dermatovenerological and oncological services to provide specialized care to patients with pre-tumor and malignant skin pathologies - Guidelines No. 2003/60-M, 2003;
8. Paltsev M.A., Potekaev N.N., Kazantseva I.A. and others. Clinical and morphological diagnosis of skin diseases (atlas) - M.: Medicine-2004;
9. Fitzpatrick T., Elling D.L. Secrets of dermatology /Trans. from English - M.S.Pb - BINOM - Nevsky dialect - 1999;
10. Chervonnaya L.V. Diagnosis of skin tumors of melanocytic origin // Abstract. dis. .. doc. medical sciences-2003;.
11. Chissov V.I., Romanova O.A., Moiseev G.F. Early diagnosis of melanoma. - M.: Yulana Trade, 1998;
12. Anderson RG //Select. Read. Plast. Surg.-1992.-Vol.7.-P.1-35;
13. Barnhill RL, Lewellin K. Benigh Melanocytic Neoplasm /In: Dermatology /Ed. J.Bolognia et al.-Mosby-Edinburg-2003.-P.1757-1787;
14. Barnbill RL, Mihm MC Histopathology and precursor lesions /In: Cutaneous melanoma, 3ed/Ed. CM Balch et al.-St.Louise, Quality Medical.-1998.-P.103-133;
15. Bhawan J.//Cutan Pathol.-1979.-Vol.6.-P.153;
16. Bogdan I., Smolle J., Kerl H. et al.//Melanoma Res.-2003.-Vol.13.-P.213-217:
17. Clemente C., Zurrida S., Bartoli D. et al. //Hitopathology-1998.-Vol.27.-P.549-555;
18. Crulich AE et al.//Int.J.Cancer-1996.-Vol.67.-P.485;
19. Elder DE, Elenitsas R., Murphy GF, Xu X. Benign pigmented lesions and malignant melanoma / Lever's Histopathology of the Skin .Ed.: DEElder-9th ed- Lippincott Williams & Wilkins-Philadelphia-2005.-P.715-803 ;
20. Eskandrapour M., Hashemi J., Kanter L. et al. Frequency of UV-inducible NRAS mutations in melanomas of patients with germline CDKN2A mutations //J.Natl.Cancer Inst.-2003.-Vol.95.-P.790-798;
21. Goettman-Bonvallot S., Andre J., Belaich S. // J.Am.Acad. Dermatol.-1999.-Vol.41.-P.17-22;
22. Kopf AW, Waldo E.//Aust.J.Dermaatol.-1980.-Vol.21.-P.59;
23. Kornberg R., Ackerman AB//Arch.Dernatol.-1975.-Vol.111.-P.1588;
24. Maize JC, Foster G. //Clin. Exp. Dermatol. - 1979. - Vol.4. - P.49;
25. Rhodes AR Benign neoplasias and hyperplasias of melanocytes //Fitzpatrick's dermatology in general medicine - 5th ed.//Ed. IMFreedberg et al. —Mc Graw-Hill-New York. - 1999. - P.1018-1059;
26. Rich P. //J.Dermatol.Surg.Oncol.-1992.-Vol.18.-P.673-682;
27. Rock B., Hood AF, Rock JA // J.Am.Acad. Dermatol.-1990.-Vol.22.-P.104-106;
28. Scher RK, Silvers DN // J.Am.Acad. Dermatol.-1991.-Vol.24. -P.1035-1036;
29. Shelly WB //Arch. Dermatol.-1960.-Vol.81.-P.208;
30. Tajima Y., Nakaijama T., Sagano I. et al //Am.J.Dermatopathol-1994.-Vol.16.-P.301-306.
What to do with huge nevi
We are accustomed to the fact that most moles are small formations and are almost invisible on the skin. Giant nevi do not live up to expectations.
As the name suggests, they are very large - with a diameter of 20 cm. Such moles cover a significant part of the arms, legs and face.
Congenital nevi of this type grow in people of any race - they spoil the lives of 2% of the world's population. But it is not their size that is dangerous.
A giant mole is likely to degenerate into melanoma, especially when the nevus grows near the spinal column.
The surface of the new growth is rough, and its color is gray, brown or black. Gradually the nevus grows. The skin on it thickens, and pigmentation intensifies. Very often, hair grows in certain areas of the mole.
The neoplasm looks especially terrifying after the birth of a child - on a tiny body it looks simply gigantic. The baby grows faster than the nevus. Therefore, the mole appears to shrink over time, but in fact it continues to grow.
In 30% of cases, a giant nevus degenerates into melanoma. Transforms at any age. Some people face this threat in their youth, others live with it into old age. It is noteworthy that large moles do not disappear even in old people.
When reborn they:
- Are increasing
- Change colors and shapes
- Bleeding
- Covered with a crust
Doctors recommend removing these nevi. Usually a surgical operation is performed - the doctor cuts off the mole with a scalpel. This method is not always available if the tumor is located in a complex location or for other reasons.
Instead it is assigned:
- Curettage
- Dermabrasion
- Ablative laser therapy
These procedures do not completely remove the nevus, but eliminate its external imperfections: hair, strong pigmentation.
Large moles on the face are especially difficult to deal with.
Complications of nevi
The most common complications of all types of pigmented nevi are degeneration into melanoma and infection. Malignization is typical mainly for giant and blue nevi, as well as for borderline pigmented nevi.
Signs of malignant degeneration of nevus:
- horizontal or vertical growth;
- ulceration and bleeding;
- the appearance of irregular shapes and changes in shape;
- change in color of the nevus;
- the appearance of burning, itching, pain;
- dropouts (daughter spots next to the main one).
The occurrence of at least one of the above symptoms is a reason to immediately consult a doctor.
Nevi on the head
One of the main reasons why people remove moles is cosmetic. Growths on the chest and legs can also look unsightly, but they are almost always hidden under clothing.
With nevi on the head everything is more complicated.
For some people, these moles emphasize beauty, for others they spoil the whole impression. Many people want to get rid of even harmless tumors that will never develop into malignant tumors.
Nevi on the neck are removed for similar reasons.
Moles in this place constantly touch clothing and become damaged. Of course, not all. Flat growths are usually invisible and do not rub against tight clothing. High nevi are another matter. Dermatologists recommend removing such moles if they become damaged and inflamed. In general, they cause a lot of trouble without possibly turning into deadly melanoma.
The face and neck are not the only places where nevi appear. They also appear in the hair, and it is much more difficult to detect them. And it's easier to damage.
In this part of the body, nevi of the sebaceous glands are often found - a warty yellow-pink plaque without hair. Has an oval or irregular shape.
This mole grows due to:
- Human papillomavirus
- Genetic predisposition
Nevus of the sebaceous glands appears both among the hair and near the ears, on the neck or face. In most cases, it is formed during fetal development, but it can also grow in children.
How to identify such a mole?
Doctors usually notice it immediately after the baby is born. They perform examination and dermatoscopy. Sometimes a histological examination is necessary - dermatologists examine a sample of the nevus under a microscope.
Do I need to remove a mole right away?
No. She is reborn only at puberty. Therefore, nevi of the sebaceous glands are removed in adolescents, and not in infants.
Moles of different sizes are removed.
Large ones are eliminated surgically, small ones - with laser, cryodestruction or electrocoagulation.
Before surgery, the child should have the nevus checked regularly by a dermatologist.
Treatment of congenital non-tumor nevus
Congenital non-tumor nevi do not require special treatment. More often, patients are only concerned about a cosmetic defect. However, changes in the color, size, shape and consistency of the nevus, its severe pain, and enlargement of nearby lymph nodes are indications for excision. After surgery, the patient’s treatment tactics are determined taking into account the biopsy data of the affected and nearby skin area and the localization of the formation. Removal of nevus of the sebaceous glands is carried out for preventive and cosmetic purposes (there is no hair in this area), and not because of the risk of malignancy.
Out of sight, out of sight. How to get rid of moles
Not an easy question. Many factors influence the ability to remove tumors. Unfortunately, no pills have yet been invented that will relieve you of annoying or dangerous moles.
Yes, treatment of small nevi usually does not cause problems.
Successful removal depends on:
- Doctor's qualifications
- Mole size
- Nevus locations
The first option is surgery. The doctor cuts off the mole, some adjacent skin, and then stitches the wound. After removal, the nevus heals quite quickly, but a noticeable mark remains.
Whether this is good is up to you to decide.
What about laser surgery?
Yes, modern technologies do offer new treatments, but they do not work miracles, as some people believe. Some skin diseases are treated with lasers. But not all nevi.
The laser beam vaporizes the outer layer of skin and cells of the mole. The deeper it is rooted, the more difficult it is to destroy it completely - sometimes the surface layer is burned out, but the base remains intact. Then the nevus grows back.
The operation has to be repeated again and again, and there is no guarantee of results. So the surgical procedure is sometimes more reliable than laser surgery.
However, in some situations, a high-tech procedure accomplishes the task. Removes small nevi. Working with large tumors is much more difficult.
We recommend choosing laser nevus removal only after consulting a dermatologist and checking the tumor.
Another important point is the choice of doctor. Many doctors have accumulated vast experience in removing small moles. Everyone has them. Therefore, doctors work with them very often and know well how to quickly remove nevi.
But what about large moles?
They are not common and therefore it is difficult to find a doctor who regularly operates on them. Read reviews about nevus removal on the websites of different clinics. This is useful. You will learn what operations the doctors of these medical institutions performed and the patients’ impressions of their work.
Gather more information.
When you see your dermatologist, ask about available methods for removing moles. Perhaps in your case, surgery and laser therapy are not the best options. Harmless nevi do not need to be removed at all.
Many medical institutions remove moles. But where to go? We would like to recommend one of these clinics.
Seeing a doctor
Visiting a doctor is recommended in three cases. The first is the detection on the body of obvious signs of degeneration of nevocytes. The second is the presence of nevi with an inconvenient localization (neck, armpits, perineum). The third is the active growth in the number of moles and the desire to make sure that there is no risk of developing a malignant tumor.
A dermatologist examines the spot, if necessary, takes a sample of the nevus for histology to determine the nature of the formation and prescribes treatment.
The specialist needs to obtain maximum reliable information about the non-cell cells in question:
- date of appearance (present from birth or appeared later);
- behavior over the past weeks (pain, growth, change in color);
- history of previous treatment (if any).
You can get advice from qualified dermatovenerologists at JSC “Medicine” (clinic of academician Roitberg). The clinic is located in the central administrative district, within walking distance from the Mayakovskaya, Belorusskaya, Novoslobodskaya, Tverskaya and Chekhovskaya metro stations.
The clinic’s equipment makes it possible to analyze nevi and melanomas, and to painlessly and completely remove these formations from the skin of patients. You can make an appointment by calling +7.
Removal of nevi at the Lasersvit clinic in 100 seconds or less
Nowadays, beauty salons easily remove nevi of various types. And the procedure is inexpensive. But the quality and result of the operation are not always guaranteed.
Only have moles removed in well-equipped clinics.
And that's why.
The basis of a successful operation is accurate diagnosis of tumors. Sometimes simply examining a mole is not enough and dermatoscopy is needed. That is, the use of a dermatoscope.
The Lasersvit clinic uses a Delta 20 T dermatoscope, which magnifies the image of the skin 16 times. With its help, our doctors can easily determine the type of nevus and promptly notice signs of degeneration. Helps quickly detect melanoma.
Our doctors have accumulated enormous experience in diagnosing moles - they have examined over 100,000 patients. They are familiar with cutting-edge research in the field of neoplasms because they studied abroad. Even dermatologists of the second category.
Lazersvit doctors can easily remove nevi from an adult or child. Benefits of the procedure:
- Rapidity
On average, one small mole is removed in 1-2 minutes. Therefore, sometimes doctors remove many nevi at once, one after another - for 20 moles it will take from 30 to 40 minutes.
- Painless
The laser pulses are very short - they last a fraction of a second, and the skin is constantly cooled. Patients do not have time to feel anything. In long operations on large moles, local anesthesia is used.
- Bloodlessness
The laser beam destroys nevi, seals blood vessels and prevents bleeding.
- Easy healing
A protective crust grows at the site of the removed mole, which prevents infection. It disappears within a week. Skin redness disappears within 3 weeks.
- Tracelessness
The laser destroys only nevus cells and when they are destroyed, the skin is restored. The new skin is smooth and without scars.
- Efficiency
Evaporated tumors are not rebuilt, as doctors burn out all their cells.
What about the price of nevus removal?
It depends on the type of tumor, its size and location. Moles in hard-to-reach places are more difficult to remove, which means the cost of the procedure increases. Sometimes additional surgery is needed.
Large nevi cannot be removed immediately and doctors treat them in several stages. Talk to your dermatologist after your examination and he will explain in detail how much it costs to remove a specific mole and how long the procedure will take.
Come to Lasersvit for quick and comfortable removal of dangerous and inconvenient nevi.
Congenital malformations of the skin and subcutaneous fat
Congenital malformations of the skin and subcutaneous fat in children have various forms of manifestation.
One of them is nevus. This is a neoplasm that appears as a result of a high concentration of nevocytes in a certain area of the skin. Normally, skin color is formed by melanocytes distributed in equal density. However, pathology may develop, due to which melanocytes degenerate into nevocytes, which, through their accumulation, form a pigmented nevus in a child. It can occur during pregnancy or appear shortly after birth.
To one degree or another, the following factors can lead to the development of pathology:
- gene breakdown;
- the presence of a genitourinary infection in the mother during pregnancy;
- heredity;
- the impact of negative external factors on the mother’s body during pregnancy;
- incorrect diet of the mother during pregnancy, the predominance of artificial colors, preservatives, and flavors;
- long-term use of hormonal contraceptives before pregnancy.
Initially, pigmented nevus in children is defined as a benign formation. However, it may have melanocytic activity, which means it can grow. As the child ages, not only the spots may grow, but also the appearance of new ones, as well as their degeneration into malignant tumors. A skin tumor - melanoma - is aggressive, as it quickly progresses and metastasizes to nearby organs and tissues.
Pigmented nevus is detected in approximately 1% of children.
Boys and girls are equally susceptible to the appearance of spots on the skin. A nevus can look different: a medium or large-sized nodule, a spot colored differently from the main skin tone, a wart. Localization is also varied: limbs, torso, head. In most cases, nevus occurs on the child's head, neck, chest or upper back.
The size of the formations varies from several mm to several cm. In approximately 5%, the number of nevi is so large that they occupy a significant proportion of the skin surface. Normally, when palpated, they can be both soft and nodular, but without pain.
Symptoms
A giant nevus is visible immediately after the birth of a newborn. It has the following distinctive features:
- localized on the body, neck, limbs, head;
- rarely found on the face;
- the diameter of the spot is more than 10 - 40 cm;
- its area can occupy the entire anatomical region (symmetrical or unilateral location);
- increases with the growth of the child;
- brown, gray or black;
- heterogeneity of color;
- uneven surface (with knots, cracks);
- completely or partially covered with hair (vellus or coarse);
- sometimes surrounded by small nevi;
- does not disappear;
- may be accompanied by other congenital anomalies (hydrocephalus, neurofibromatosis, etc.).
Methods for treating nevi
Treatment is allowed only in patients over 2 years of age. Therapy has 4 main directions:
- surgical removal;
- laser excision;
- cryodestruction;
- electrocoagulation.
As a rule, nevi that have grown deeply into the tissue are surgically removed. Giant neoplasms are removed in several stages, but the disadvantage of this method is the formation of scars at the site of the nevi.
Laser coagulation is used to remove dysplastic pigmented nevi and other clinical types of spots. The method allows removal of the formation without pain and without subsequent scarring.
Cryodestruction involves exposing the affected area of skin to very low temperatures. As a result, the altered cells die and are replaced by healthy ones. After cryodestruction, a small crust appears, which quickly disappears.
Electrocoagulation affects the nevus with high temperatures. Typically this method is used to remove small and medium-sized stains.
Forecast
In some patients, as they mature and grow, the size and intensity of the color of the giant nevus decreases somewhat. But the transformation of a benign giant nevus into a malignant melanoma occurs in 1.5–13% of patients (including in childhood), so patients should be monitored by an oncologist for life (even after removal of this pigmented formation). In addition, they should beware of excessive insolation, mechanical and chemical effects on the giant pigmented nevus.