A nevus is a benign skin tumor, popularly called a mole or birthmark. The name comes from the Latin Naevus, because. the tumor consists of nevoid cells. Appearing on the human body as a result of environmental influences, such formations can be localized in any part of the body, not excluding the mucous membranes. Nevi can vary in shape and size, appear as a flat spot or pea, and their color varies from light to dark brown. The number of moles changes throughout life; they are almost never found in newborn children, but in adolescence they appear in almost everyone.
Main types of nevi
- Giant pigmented nevus is usually of congenital origin. These extensive formations can be located on the limbs, face, torso, even the smallest of them can reach a diameter of up to 20 cm.
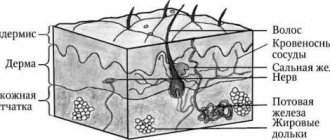
- Epidermodermal nevi are different stages of the transition of epidermal melanocytic structures into the dermis, as well as the initial stage of development of its intradermal part. This can only be determined by histological examination (see Fig. 2)
- Intradermal nevus is the most common. This form is characterized by localization at different levels of the dermis, and a combination of different stages of appearance is possible. In its development, this type of mole goes through several stages: resumption of borderline activity and transition to a complex form, spontaneous focal or complete regression, appearance of a nodular or superficially growing melanoma against the background of a nevus (see Fig. 3)
- Epidermal melanocytic nevi - differ in size, shape, degree of pigmentation, as well as the nature of the surface. The most common are flat moles, the sizes of which vary from 0.1 to 10 cm (see Fig. 4)
- Blue nevus is a melanocytic type with a rare primary localization of the process in the dermis. Most often it affects the skin of the face, limbs, and buttocks.
- Halonevus or Setton's nevus - occurs in most cases in adolescence; their appearance in a later period may indicate the presence of a serious pathology. This species is characterized by the appearance of a white corolla around a brown mole (see Fig. 5)
- Papillomatous nevus - protrudes on the surface of the skin and has an irregular shape, resembling a cauliflower in appearance. It attracts attention with its repulsive appearance (see Fig. 6).
- Fibroepithelial nevus - this type of tumor is characterized by a rounded dome-shaped shape, the size of the formation is 0.3-1.5 cm. The color is close to the color of the skin. Due to exophytic growth, they are often injured, but malignancy is extremely rare (see Fig. 7).
Borderline nevi are formations that rise slightly above the surface of the skin, but without a specific localization. Their sizes are usually 0.2-0.5 cm, the color can be from light to dark brown. Formations of this type have clear cytological, topographic and architectural features. At the level of the epidermal junction in the basal layer of the epidermis, they form spherical structures, large nests, and, less commonly, zones of diffuse melanocytic transformation (see Fig. 7-10).- Reed's nevus is very dangerous due to its possible degeneration into melanoma. A tumor of this type is characterized by a combination of signs of juvenile and dysplastic nevi (see Fig. 8).
- Dysplastic nevus or Clark's nevus is the most dangerous type of tumor. According to statistics, half of them develop into melanoma. A flat, irregularly shaped mole has an uneven color. It is characterized by three stages of dysplasia, the third being the stage preceding melanoma. The reverse process is possible, but complex forms can also appear, which means either the reversibility of the stage or incomplete completion. The development of a complex nevus is characterized by several stages: 1) transition to an intradermal form; with the activation of borderline activity, a transition to a complex form is possible; 2) spontaneous regression (reverse development); 3) transition to melanoma.
Diagnostics
The set of diagnostic measures includes:
- Examination by a dermatologist/oncologist.
- Dermatoscopy is a microscopic examination.
- Ultrasound of the neoplasm - to assess the depth of nevus growth into the layers of the skin.
Reference! A biopsy of a “living” mole is not performed, since as a result of this procedure the nevus is injured, and mechanical damage can provoke degeneration into melanoma. Therefore, histological examination is carried out after removal of the tumor.
Treatment
Treatment of nevi is indicated only in cases where there are signs of transition to a malignant formation. However, in cases where there is a high probability of injury to the mole, its removal is recommended. To select the appropriate method, the size of the tumor is taken into account, as well as its condition and the presence of signs of malignancy. Among the most commonly used treatment methods are:
- Destruction using a laser or electrocoagulator - excision under the influence of high temperatures or a laser. With the electrocoagulation method, the vessels are cauterized during the procedure, so the risk of bleeding is eliminated. The laser affects the deep layers of the skin, but healthy areas are not affected. This method is recommended for removing small moles.
- Chemical destruction - based on the destructive action of chemicals. It should be taken into account that incomplete removal of a mole threatens the development of a malignant process. Therefore, the most effective method is still surgery.
Signs of nevus degeneration into melanoma
Symptoms of nevus malignancy are:
- Change in color (decrease or increase in pigmentation).
- Mole compaction.
- Growth of the neoplasm – in diameter or height.
- Redness.
- The presence of ulcers on the mole.
- Bleeding from a nevus.
- The appearance of black dots around a mole or birthmark.
- Hair loss from nevus.
- Feeling of warmth, itching or burning in the area of the tumor.
- Enlargement of regional lymph nodes.
If such signs are present, you should immediately contact a dermatologist and oncologist.
Prognosis and prevention
The prognosis of the disease depends on its size and the number of metastases. Thus, with a tumor thickness of less than 0.75 mm, non-pigmented melanoma is completely cured. If the tumor extends to 0.75-1.6 mm in thickness, the 5-year survival rate is about 85%. The nodular form of the tumor has a poor prognosis due to its rapid progression.
Prevention consists of protection from ultraviolet radiation - clothing, sunscreen, avoiding sunbathing. If there have been cases of skin cancer in the family, or the person has risk factors for melanoma, the presence of mutations in individual genes can be determined. If the result is positive, you will have to be extremely careful when tanning, avoid skin injuries and, in particular, damage to pigment formations.
| Read more about dermatological research at Euroonko | |
| Consultation with a dermatologist-oncologist | from 5100 rub. |
| Skin examination using the German FotoFinder device | 12100 rub. |
| Diagnosis of melanoma | from 5100 rub. |
Book a consultation 24 hours a day
+7+7+78
Literature
- Fernanda Teixeira Ortega, Rogério Nabor Kondo and etc. Primary cutaneous amelanotic melanoma and gastrointestinal stromal tumor in synchronous evolution // An Bras Dermatol. 2021, Sep-Oct; 92 (5)
- Kubanov A.A., Gallyamova Yu.A., Bisharova A.S., Sysoeva T.A. Features of diagnosing amelanoma // Attending physician, No. 8, 2018.
- Snarskaya E.S., Avetisyan K.M., Andryukhina V.V. Pigmentless nodular melanoma of the skin of the leg // Dermato-oncology, No. 2, 2014.
- Lemekhov V.G. Epidemiology, risk factors, screening for skin melanoma // Practical Oncology, No. 4, 2001.
- Melanoma of the skin. Clinical recommendations of the Ministry of Health of the Russian Federation. 2021 approval year.
- Zhapekova Zh.A. Genetic predisposition to melanoma. Materials of the IX International Student Scientific Conference, 2017.
- Queirolo P., Spagnolo F., BRAF plus MEK-targeted drugs: a new standard of treatment for BRAF-mutant advanced melanoma, 2021.
Symptoms of the disease
Amelanotic melanoma is a nodule on the skin:
- round or oval;
- densely elastic to the touch;
- "fleshy";
- flesh-colored, pinkish, brownish or bluish-reddish in color;
- with a surface on which there is no usual skin pattern;
- may have a leg;
- It doesn't hurt, but it may itch.
Unlike pigmented melanoma, a tumor of melanocytes without pigment is often more symmetrical, it is less prone to swelling and the formation of small satellite papillae around it.
“Colorless” melanomas grow quickly - growing from 2-3 mm to 2-3 cm in just 2-4 months. Such a “nodule” may be lumpy, and ulcers or formations similar to small papillomas can be found on it.
The most dangerous thing is that the growth of achromatic melanoma is observed not only upward, but also deep into the skin. It is prone to decay. Therefore, in the later stages, the tumor looks like an ulcer, the edges of which are dense and raised, and small papillae are visible at the bottom.
How to recognize amelanotic melanoma in the early stages?
The first symptoms of non-pigmented melanoma are the appearance of a pink spot on the skin (clean or in the area of pigment formations). Such a spot grows over several weeks/months and is characterized by increased friability and bleeding.
Some types of melanoma without pigment look like a gradually enlarging wart or papilloma. Other non-pigmented melanomas appear as a brown streak on the nail that extends to the tip of the finger.
In the initial stages, non-pigmented tumors do not hurt or itch, so they are rarely paid attention to.
Causes
The following causes of pigmented nevi are distinguished:
- Congenital features. The migration of cells and their redistribution between the layers of the epidermis are disrupted. In children, the development of the disease occurs mainly according to this mechanism.
- Hereditary factor. Caused by a violation of cellular proliferation of the epidermis due to hereditary defects in the structure of cells.
- Impact of negative external factors. First of all, we are talking about exposure to ultraviolet rays. In this case, a restructuring of the cellular structure of the formation occurs and its degeneration into oncogenic forms, for example, melanoma. Strong background radiation also matters.
- Skin injury. Scratching the formation, its damage by friction with clothing and shoes can lead to the growth of pigment spots.
- Incorrect treatment of pigmented nevi. With illiterate therapy, a relapse of the disease is possible. The reason for this may also be folk methods of self-medication (cauterization with acid, for example)
- Ethnic race. The factor is associated with the pattern of melanocyte redistribution in people of different ethnicities. People with white skin and blond or red hair are at high risk of degeneration.
- Endocrine disorders (hormonal imbalance during pregnancy). Exchange and metabolic processes in the human body (including in the layers of the epidermis) are restructured.
- Unbalanced diet. This factor plays a significant role in the development of any pathological process in the human body, including various birthmarks.
Amelanotic melanoma - what is it?
This is a malignant tumor whose cells contain an extremely small amount of the pigment melanin (this is what gives the brown color to “regular” melanoma). As a result, neoplasia is very similar to various other skin growths, both malignant and benign. Therefore, it is quite difficult to diagnose achromatic melanocytic tumor at an early stage.
Melanoma containing little melanin is characterized by fairly rapid growth into fatty tissue and early ulceration. This creates conditions for metastasis.
A peculiarity of non-pigmented melanoma is the cessation of its growth after the sending of the first metastases. Moreover, after this, the primary tumor can completely disappear.
Colorless melanoma cells contain small amounts of melanin due to:
- insufficient content of the amino acid tyrosine in the body;
- disruption of melanin formation during tumor cell division.
Melanoma histology
Microscopic diagnosis of pigmented skin lesions is based on identifying and determining the properties of malignant melanocytes. Aggregation (clustering) of atypical pigment cells can be observed in atypical dysplastic nevi. They are sometimes difficult to distinguish from superficial spread of malignant melanoma. Rare forms such as desmoplastic melanoma are morphologically similar to benign skin changes, which can cause diagnostic errors.
All cases of histological testing of tumors require experience and high professional skill.
When conducting histology of malignant melanoma of the skin, the pathologist has to evaluate many factors:
- type of melanoma;
- tumor thickness;
- presence of ulceration;
- infiltration;
- degree of vascular invasion;
- fields of surgical resection (tumor edges);
- mitotic rate or Clark levels.
In addition, the doctor comments on the possible invasion of lymphocytes, the presence of necrosis, cell regression and the level of neurotropism (tumor growth relative to the nerves).
Based on the results of histology of skin cancer, the type of tumor is determined in accordance with the characteristics of cellular morphology.
Tumor thickness is the most important factor in histological evaluation. It is measured in micrometers (μm) and represents the longest diameter from the top of the tumor to the lowest (deepest) epidermal tumor cell.
The pathologist, examining the removed pathological tissue, must make sure that the entire tumor has been resected and sent for examination, and determine the type and stage of melanoma growth. Pathological sections should include fragments with expected deep infiltration.
Any suspicion of skin cancer must be accompanied by histology. Histological information is important for treatment selection and further evaluation of patients with melanoma. Satellites present in the dermis must also be included in the preparation. Assessment of tumor thickness may be uncertain or impossible if there have been regressive changes in the tumor.
The pathology report of malignant tissue should include the following factors:
- histological type (invasive or in-situ);
- tumor thickness during germination (Breslow) in tenths of mm;
- ulceration (present or not);
- other factors (vascular infiltration, lymphocyte infiltration);
- marginal resection margins.
For resected lymph nodes, the following data are decisive for diagnosis and treatment:
- number of metastatic nodes;
- total number of resected nodes;
- perinodal tumor growth;
- properties of the tumor in the area of the resected area.
Histological examination of malignant melanomas of the mucous membranes reveals a variable microscopic picture. Lymphocyte infiltration is less pronounced compared to skin lesions. About 1/3 of melanomas in the nose and mouth are amelanotic. This type of tumor is difficult to differentiate from other types of mucosal cancer. Melanoma immunohistochemistry is useful in this regard.
What is papillomatous nevus
Not all skin growths are moles. There are also warts, condylomas and papillomas, which are sometimes difficult to distinguish from nevi. It is especially difficult with papillomatous pigmented nevus .
It looks like a regular papilloma.
But in fact, this is a convex, bumpy mole - a benign formation that never turns into cancer. Usually a nevus is flesh-colored, brown or brown. Black is rare.
Most interdermal pigmented nevi grow hair and form on the head or neck. In rare cases - in other areas.
Such moles appear at any period of life: at birth, in adolescence, in old age. At first they are invisible. However, nevi continually grow and soon begin to interfere. If they appear among the hair on the head, then combing can damage them. Inflammation will begin. Moles constantly hurt, and the skin around them turns red.
A papillomatous nevus on the face is a serious cosmetic defect, because it constantly grows and is striking.
People with such moles often want to have them removed. But we recommend making a decision only after consulting a dermatologist and checking the tumor for the risk of degeneration. This nevus is similar to papillomas. Without the help of a doctor, you will not be able to determine how dangerous a mole is.
Usually, a dermatologist prescribes surgery if the nevus is constantly injured and inflamed or spoils the patient’s appearance. Before surgery, the doctor must rule out the possibility of melanoma. He performs a dermatoscopy of the mole.
Papillomatous nevus is removed using different methods:
- Laser
- Cryodestruction
- Radio wave surgery
- Electrocoagulation
- Surgical excision
A common method for removing tumors on the face and neck is laser.
How to distinguish a regular mole from a dysplastic nevus?
Atypical nevi have a number of characteristic features that can occur either individually or in combination with each other.
| Round, symmetrical shape | Uneven edge and/or asymmetrical shape |
| Completely flat or completely raised above the skin | One part can be raised, the other flat (fried egg) |
| Uniform color or shades of brown | Black, red, brown at the same time |
| Size less than 6mm | Size over 6mm |
| Localization on any part of the body | Rarely located on the face |
Surgical operations
Large papillomatous nevus undergoes surgical excision. The application of small cosmetic stitches after the removal operation guarantees minimal cosmetic defects. The possibility of relapse is excluded, since along with the nevus, the doctor also captures part of the healthy tissue when removing it. Giant nevi are also treated surgically. They are rare, but the risk of developing cancer in them is very high. Treatment of giant pigmented nevus is carried out in stages, with the involvement of plastic surgeons for further cosmetic operations.
Currently, there is no method that can prevent the appearance of a nevus. The only thing that can be avoided is the transformation of a nevus into melanoma. To do this, you just need to make sure that the nevus is not injured. Under no circumstances should you engage in self-extraction and self-diagnosis of nevi, as this may lead to undesirable consequences. Do not neglect your health, and if a large mole appears or damages an existing one, consult a doctor immediately.
Treatment of specific skin lesions
The treatment process for various pigmented nevi begins after all diagnostic measures have been completed (it is recommended to perform a tissue biopsy). Drug therapy is almost never used, since it does not have a pronounced effect on existing formations. A course of drug treatment is prescribed if moles arise against the background of other abnormal processes in the body. Getting rid of the nevi themselves involves surgical removal.
The following treatment methods are available:
- surgical removal of a pigment spot or mole;
- folk recipes for mole excision;
- preventive measures in case of refusal of removal.
Mole resection
A surgical procedure is prescribed for medical reasons or in connection with the desire of the patient in case of obvious cosmetic defect. A mole is removed in a medical office in the following ways:
- Tissue excision. Manipulation is carried out using a scalpel. The doctor removes the pigment and some area of the skin around it.
- Cryodestruction. Tissue freezing is performed. At the same time, cell division stops and their death occurs. The frozen skin fragment is removed without damaging the dermis underneath. The advantage of this method is that it is painless and leaves no traces after the procedure. But with cryodestruction, in 50% of cases there is a risk of leaving parts of the nevus, which contributes to relapse of the disease.
- Laser surgery. Surgical removal with a laser is the most popular way to get rid of the formation. The laser evaporates fluid from the tissue, causing the cells to die. This procedure is usually carried out without anesthesia. When removed, the patient feels a slight tingling or warmth. The advantage of the procedure is that it can be used for multiple nevi. There are no scars or scars after removal.
- Electrocoagulation. The event is reminiscent of laser evaporation of tissue. Cell destruction occurs under the targeted influence of electric current. The method is used mainly when removing small-sized formations.
Folk remedies
Many people try to remove moles using traditional medicine. It is important to visit a dermatologist or oncologist before this to rule out precancerous conditions or the degeneration of nevi into a malignant stage.
Among the folk methods of getting rid of moles, the following are popular:
- Using a lapis pencil. Lapis is the name given to silver nitrate. This substance has been used in medical practice for several centuries for the purpose of cauterization and disinfection of wounds and other skin lesions. This remedy is not used in clinics today, since in the 21st century more effective silver preparations with a similar effect have been developed. Moles are burned with lapis 1 – 2 times a day, until signs of formation appear.
- Celandine juice. The product has a disinfectant and cauterizing effect, which helps in getting rid of certain types of moles. Juice with an oily or liquid texture is applied in a thin layer to the surface of the neoplasm. The drug is sold in a pharmacy; before applying, you should read the instructions, make sure that the juice does not get on healthy skin; the treated area may tingle. The procedure is carried out after full confidence in the benign quality of the formations.
- Vinegar essence. Treatment with 70 or 80% acetic acid is considered a more effective remedy, compared to lapis or celandine, and can eliminate the tumor in 7 days. The action of the product is based on tissue cauterization. The procedure is painful. Perform treatment once a day. Afterwards, the area is bandaged with a clean bandage to prevent infection. There may be residual defects after cauterization of the mole.
Preventive measures in case of refusal of removal
To prevent the development of melanomas (degeneration of pigmented nevi into a malignant tumor), it is recommended to sunbathe with caution, especially for those with white sensitive skin. Sunscreen and wearing closed clothing made from breathable natural fabrics on sunny days will help. Regular visits to an oncologist are recommended for examination and monitoring of the condition of the tumor.
It is important to monitor the changes taking place and not to injure them. Special creams to lighten pigmentation on the skin will help. Lakshma Maxxi whitening cream is considered a successful preventive remedy that will not allow pigment formation to degenerate into skin cancer. It is one of the most popular products in the United States and has been tested by the American Dermatological Association. It eliminates the manifestations of hyperpigmentation on the skin easily, reliably and safely. Based on the results of clinical studies, the drug demonstrates high efficiency in a short time of use.
Add to cart
Underarm skin brightening treatment
RUB 1,400.00
Add to cart
Whole body skin lightening milk
RUB 3,100.00
Add to cart
Cream Lakshma Maxxi (Lakshma Maxxi)
RUB 1,800.00
Add to cart