According to statistics, every second girl who comes to see a gynecologist has encountered such an intimate disease as colpitis at least once in her life.
Colpitis or vaginitis is an inflammatory process of an infectious or non-infectious nature, affecting the mucous membrane of the vagina, and in some cases, the vulva.
This disease brings a lot of discomfort - from discharge and unpleasant odor to painful sensations during sexual intercourse, and worsens a woman’s quality of life.
At the initial stage of development, the infection is not dangerous, but the lack of timely qualified medical care or self-medication can lead to serious complications.
Causes of the disease
Depending on what is the cause of colpitis, one can distinguish specific, that is, caused by an infectious agent, and non-specific, caused by vaginal microorganisms, which normally do not cause problems in a healthy woman, but when exposed to certain factors begin to multiply intensively, causing discomfort and leading to pathological processes.
It is important to correctly determine the cause of the inflammatory process and prescribe appropriate treatment precisely aimed at eliminating the problem.
The most common causes of vaginitis are:
● Sexually transmitted infections.
A large group of diseases is caused by infections acquired through unprotected sex.
There are microorganisms that can be transmitted in this way from an infected partner through mucous membranes, but do not cause any harm to a healthy person, since his immune system suppresses the proliferation of pathogenic microflora.
However, if particularly pathogenic microorganisms occur, as well as with decreased immunity, the presence of microtrauma or concomitant diseases, an inflammatory process develops.
Colpitis can be caused by syphilis, chlamydia, gonorrhea, trichomoniasis, human papillomavirus, ureaplasmosis and many others.
The most reliable option for preventing vaginitis in this case is the use of barrier contraception methods during sexual contact.
● Damage to the vaginal mucosa.
The mucous membrane plays a very important role as a barrier that prevents microorganisms from entering the thickness of the vaginal walls. Injury to it can occur both during sexual contact and with medical instruments during improper manipulation. Through microtrauma, bacteria and microorganisms penetrate tissue and multiply there, causing inflammation.
● Impaired blood supply.
With blood, not only oxygen enters the vagina, but also many nutrients that ensure the normal functioning of the mucous membrane. With a lack of microelements, it becomes thinner and does not produce a sufficient amount of natural secretions, which leads to the formation of microtraumas.
● Endocrine diseases.
The proper functioning of the endocrine system is also responsible for the sufficient production of natural vaginal secretions and the timely renewal of the mucous membrane. With diseases of the ovaries, thyroid gland, pancreas and adrenal glands, a hormonal imbalance occurs in a woman’s body, which can lead to inflammatory processes in the vagina.
● Antibiotics.
Long-term use of broad-spectrum antibacterial drugs can lead to disruption of the vaginal microflora. The effect of antibiotics is that they destroy all pathogenic microorganisms, but along with them they also kill beneficial bacteria that make up the natural microflora.
● Weak immune system.
Immunity plays an important role in the human body, accurately identifying pathogenic microorganisms and eliminating them. After surgical interventions, long-term use of antibiotics, vitamin deficiencies, general exhaustion of the body and previous diseases, the immune system weakens and becomes unable to repel the attacks of infections, which provokes colpitis.
Trichomonas vulvovaginitis: clinical picture, diagnosis and treatment
Scientific Center of Obstetrics, Gynecology and Perinatology of the Russian Academy of Medical Sciences, Moscow
Trichomoniasis is one of the most common diseases of the genitourinary tract and ranks first among sexually transmitted diseases. Around the world, trichomoniasis affects 170 million people every year. The importance of the problem is due not only to its wide distribution and danger to the health of the sick person, but also to severe consequences in the form of complications that can cause infertility, pathology of pregnancy, childbirth, newborns, infant mortality, defective offspring, etc. This disease equally often affects both women and men. In girls, Trichomonas infestation is extremely rare. The causative agent of genitourinary trichomoniasis is Trichomonas vaginalis, it belongs to the protozoa, class of flagellates, genus Trichomonas and is a mobile unicellular organism that has adapted in the process of evolution to life in the organs of the human genitourinary system. Thanks to the movements of the flagella and the vibrations of the undulating membrane, the Trichomonas makes jerking, rotational and weakly progressive movements. Its reproduction occurs by simple transverse division; the optimal conditions for the development of Trichomonas are a pH of 5.5–6.5. Therefore, Trichomonas multiply intensively during and after menstruation, which is associated with a change in the acidity of the vaginal contents during this period. Urogenital trichomonas was first described in 1836. The Parisian physician Donne discovered it in the vaginal discharge of women with gonorrhea and syphilis, and gave it the name “vaginal trichomonas.” This term is used to this day. To date, more than 50 varieties of Trichomonas are known, distinguished by size, cell shape, number of flagella, etc. Only 3 types of Trichomonas parasitize humans: urogenital, oral and intestinal. Urogenital trichomonas are an independent species, morphologically and culturally different from oral and intestinal trichomonas. Under natural conditions, they live only in the human genitourinary system and do not affect animals. In women, the habitat of Trichomonas is the vagina, in men - the prostate gland and seminal vesicles. The urethra can be affected in both men and women. Trichomonas quickly lose their viability outside the human body. A prerequisite for life is the presence of moisture; when dried, they quickly die. Trichomonas are not resistant to high temperatures (more than 40°C), direct sunlight, or antiseptics. In distilled water, parasites die almost instantly. The low stability of urogenital trichomonas in the environment is probably due to the inability to form cysts, which sharply limits the possibility of infection through indirect contact. Water as a factor in the transmission of an infectious agent is practically eliminated. And in baths, where protozoa are exposed to high temperature, soap and water, transmission of infection is simply impossible. Infection with trichomoniasis occurs from a sick person, more often through extramarital sexual relations (in 67.2–71.6%, according to various authors). Women who have casual sex suffer from trichomoniasis 3.5 times more often than those who have one sexual partner. There is zero incidence reported in adult virgins. In prostitutes, people suffering from other sexually transmitted diseases, and in sexual partners of infected patients, it reaches 70%. Without treatment, these protozoa do not leave the host’s body and can cause all sorts of complications. Trichomoniasis was diagnosed in 70–80 year old men with last sexual intercourse 30 years ago.
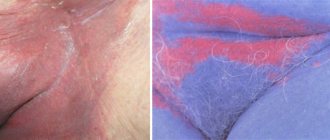
Clinical picture Trichomoniasis is a multifocal disease. Depending on the degree of involvement of certain organs and systems in the process, a topical diagnosis is made. Urogenital Trichomonas can infect the mucous membranes of the genitourinary tract, which leads to ulcers and erosions. Protozoa enter the mucous membranes of the genitourinary tract through contact with a person with trichomoniasis or a carrier of trichomonas. Trichomonas are fixed on the cells of the squamous epithelium of the mucous membrane, penetrate into the glands and lacunae. Once in the genitourinary organs, Trichomonas can cause the development of an inflammatory process. An inflammatory reaction develops in the presence of a large number of parasites. Trichomonas, feeding endosmotically, release hyaluranidase into the external environment. Hyaluronidase secreted by pathogens leads to significant loosening of tissues and more free penetration of toxic metabolic products of bacteria and accompanying flora into the intercellular space. In the area of infection of the mucous membranes, an inflammatory process develops: hyperemia, swelling, exudation, desquamation of damaged epithelial cells. Minor hemorrhages and ulcerations may occur. Cell fragments of dead and living pathogens accumulate in the exudate. Thus, the site of penetration of Trichomonas in women is the vaginal mucosa. Then, gradually, the pathological material enters the urethra and cervical canal and spreads over the surface of the mucous membranes. Vulvitis, vestibulitis, bartholinitis, cervicitis are rarely primary; they arise secondary and are combined with colpitis. Ascending infection of the genitourinary organs also occurs. The internal os of the cervix is a kind of boundary for the upward spread of urogenital trichomonas due to the circular compression of the cervical muscles and the sharply alkaline reaction of the endometrial secretion. These protective barriers lose their strength during menstruation, abortion and childbirth. In addition, the rhythmic movements of the uterus during sexual intercourse are predisposing factors for the absorption of urogenital trichomonas located in the cervix into its cavity. When trichomonas penetrate into the pipes, trichomonas salpingitis occurs. As a rule, there is no isolated inflammation of the ovaries; usually this lesion is observed together with damage to the fallopian tubes. Urogenital Trichomonas penetrate into the ovary through the wound surface of a burst Graafian vesicle. Tuboovarian formations may occur. Urethritis can be either primary or secondary. Most often, the anterior part of the urethra is affected, but sometimes the infection spreads to the posterior part of the urethra and total urethritis occurs, which over a long period of time can lead to the formation of multiple strictures. Paraurethritis, cystitis and even pyelitis may occur. The pathogenesis of the disease is influenced by the following factors:
- intensity of infection,
- pH of vaginal contents,
- physiological state of the mucous membranes,
- accompanying flora.
Depending on the duration of the disease and the intensity of the body’s reaction to the introduction of the pathogen, the following forms of trichomoniasis are distinguished.
- Fresh
- spicy,
- subacute,
- torpid (low-symptomatic).
- Chronic (torpid course and duration of the disease for more than 2 months or unknown duration of the disease).
Trichomonas carriage (in the presence of Trichomonas in the vaginal discharge there are no objective and subjective symptoms of the disease) None of the clinical signs of Trichomonas infection is strictly specific. In acute trichomoniasis, the inflammatory process proceeds violently, with copious discharge that irritates the skin and severe itching of the external genitalia. I am concerned about burning and pain when urinating. Discharge from the genital tract is noted by 50–75% of women, an unpleasant odor – 10%, itching of the genital organs – 25–80%. Often the itching is so severe that sleep is disturbed. Dysuria occurs in approximately 35% of patients. Painful urination can be understood as a symptom indicating damage to the urethra, or, more often, as a possible leakage of urine onto the inflamed vulva. Pain in the lower abdomen occurs in 5–12% of infected women. Complaints appear soon after the start of sexual activity or casual sexual intercourse. The incubation period for trichomoniasis is on average 5–15 days. Clinical manifestations of the inflammatory process intensify after menstruation. Upon examination, inflammatory changes are revealed from moderate hyperemia of the vaginal vault and cervix to extensive erosions, petechial hemorrhages and diaper rash in the perineal area. A very characteristic, but not constant symptom is the presence of granulomatous, loose lesions of the mucous membrane of the cervix, red in color (crimson cervix). In the area of the posterior fornix, there is an accumulation of liquid grayish-yellow, foamy discharge that flows freely from the vagina, irritating the skin. Genital warts may form in the area of the vaginal vestibule. When the urethra is involved in the inflammatory process, its lips are often swollen and hyperemic; a small amount of purulent discharge can be squeezed out with a massage. When palpating the urethra, its soreness and pastiness are noted. There may be hyperemia at the mouth of the duct of the greater vestibular gland. During colposcopy, pinpoint hemorrhages are detected on the mucous membrane of the vagina and the vaginal part of the cervix (strawberry cervix symptom). Foci of inflammation when stained with Lugol's solution are iodine negative. In the subacute process, the symptoms are minor, the discharge is not abundant. The torpid form of trichomoniasis, which most often occurs in men, is characterized by a paucity of objective and subjective symptoms or their complete absence. In women, the mucous membranes of the vagina and external genitalia are of normal color or slightly hyperemic, vaginal discharge is milky in color, and its amount is insignificant. Obliterated signs of the inflammatory process (often pronounced focal or diffuse hyperemia, petechiae) are revealed only during colposcopy. The transition of infection to the chronic stage occurs through the gradual subsidence of acute and subacute phenomena. However, periodic exacerbations may occur, which are most often caused by sexual intercourse, alcohol consumption, decreased body resistance, impaired ovarian function and changes in the pH of the vaginal contents. Chronic genitourinary trichomoniasis, as a rule, is a mixed protozoan-bacterial process, since Trichomonas is a reservoir for chlamydia, ureaplasma, gonococci, staphylococci and other flora. Only in 10.5% of patients trichomoniasis occurs as a monoinfection; in 89.5% of cases mixed trichomonas infections in various combinations are detected. According to our data, Trichomonas vaginalis is most often found in association with mycoplasmas (47.3%), gonococcus (29.1%), gardnerella (31.4%), ureaplasma (20.9%), chlamydia (18.2% ), mushrooms (15.7%). The ability of urogenital trichomonas to phagocytose gonococci, chlamydia, mycoplasmas, fungi and viruses contributes to a quantitative reduction of the latter, which can lead to a decrease in antigenic and toxicogenic effects on the woman’s body, and this leads to a decrease in the phagocytic reaction and a decrease in the body’s immune response to the infectious factor. As a result, an asymptomatic, sluggish course of the inflammatory process is often observed. Under the influence of protistocidal therapy, urogenital trichomonas, as a rule, disappear. However, clinical recovery does not always occur - post-trichomoniasis inflammatory processes remain. Their formation is facilitated by the fact that with the death of urogenital trichomonas, inflammation is supported by the abundant microflora that accompanies trichomoniasis. Post-trichomonas inflammatory process after treatment is diagnosed in 14.6–48.2% of women. In addition, treatment of trichomoniasis with protistocidal drugs leads to the release of the flora located inside the trichomonas and the maintenance of the inflammation process. With mixed processes, complications in patients are observed 2 times more often and are more profound. Significant disorders that develop in the body of patients with mixed urogenital infections are difficult to correct with therapeutic agents, which makes the process extremely persistent, despite the use of etiotropic therapy, and contributes to the occurrence of relapses. Trichomonas carriage should be understood as the presence of Trichomonas in the human body in the absence of clinical signs of the disease. The frequency of Trichomonas carriage, according to various authors, ranges from 2 to 41%. The true number of Trichomonas carriers is unknown. Trichomonas carriage depends both on the strain of Trichomonas and on the characteristics of the host organism. The complex antigenic structure of the outer surface of urogenital trichomonas (as well as the diversity of the erythrocyte mosaic) contributes to the formation of anti-trichomonas antibodies (AT), detected by serological reactions. It is possible that, in terms of antigenic determinants, various serological strains of urogenital trichomonas may be similar to erythrocyte antigens, which are responsible for the production of normal antibodies that constantly circulate in the blood serum from the moment of birth of the individual. In Trichomonas carriers, the natural immune response to the introduction of Trichomonas antigens, related to the antigens of their own erythrocytes, develops insufficiently. Local cellular immunity also plays a role. Trichomonas carriers, like patients with a sluggish inflammatory process, pose a serious epidemiological danger, being a source of spread of trichomoniasis. Trichomonas infection does not lead to the development of pronounced immunity. Serum or secretory antibodies detected in patients or survivors of trichomoniasis are only signs of an existing or previously suffered infection, but are unable to provide immunity. They are detected within a year after the illness. Therefore, their definition is not suitable for establishing cure.
Diagnosis The diagnosis of genitourinary trichomoniasis is established on the basis of clinical signs of the disease and the detection of trichomonas in the test material. For high-quality laboratory research, proper preparation of the patient for laboratory examination is important. A necessary condition is to stop using external and internal trichomonocidal agents 5–7 days before taking the material. Material for research is taken from the vagina, urethra, rectum in women and from the urethra, rectum in men; urine centrifuge and rinsing waters are also used. The material is taken with a metal loop, a pipette with a rubber balloon, or a grooved probe is used. Before taking material from the urethra, it is recommended to delay urination for more than 1–1.5 hours. The external opening of the urethra is cleaned with a cotton swab moistened with sterile saline, a probe is inserted into the urethra to a depth of 1–1.5 cm and the material is collected with a rotational movement. In children, the probe is not inserted into the urethra, but only comes into contact with the external opening. The discharge from the cervical canal is collected in the same way. Pregnant women are examined at any stage of pregnancy from all possible foci of inflammation. In the 2nd half of pregnancy, the flowing mucopurulent discharge is carefully taken from the cervical canal without inserting an instrument or loop into the canal. In girls, discharge from the vaginal mucosa is also examined, without using a speculum. The material is collected using an ear spoon, which is carefully inserted into the hymenal opening. The following methods are used for laboratory diagnosis of trichomoniasis:
- microscopy of native preparation,
- microscopy of a stained specimen,
- cultural,
- immunological,
- latex agglutination.
In native preparations, the pathogen is detected by its movement among cellular elements and microorganisms. Trichomonas vaginalis is identified by its pear-shaped and oval shape, slightly larger than a leukocyte, characteristic jerking movements and flagella, which are especially clearly visible when examined under a phase-contrast microscope. Due to the fact that when the native drug is left for a long time at room temperature, Trichomonas lose their mobility, the study should be carried out as soon as possible after receiving the material. The advantage of studying Trichomonas in stained preparations is the possibility of studying them long after the material was taken. In stained preparations, Trichomonas have an oval, round or pear-shaped shape with well-defined contours and a delicate cellular structure of the cytoplasm. The information content of this method is higher, since not only mobile forms are determined, but also stationary ones. If the results of direct examination of the pathological material are negative, Trichomonas can be detected by culturing discharge from the urethra, vagina, prostate secretion and sperm. The cultural method is of great value in recognizing atypical forms for the purpose of diagnosing trichomoniasis and monitoring the results of treatment. Immunological methods have also been repeatedly proposed for the diagnosis of trichomoniasis, but they do not give satisfactory results. With the help of various immunological reactions (RSK, RIF, RPGA) various antibodies are detected in the blood serum and secretions of the genital organs of patients. However, serological reactions cannot be used as the main diagnostic test, since in some patients they are false negative in the presence of infection, positive after treatment of trichomoniasis for 1 year, false positive in people who have not had trichomoniasis. In some cases, their use as a screening test is acceptable. However, none of these methods guarantees complete detection of Trichomonas. Therefore, to increase the percentage of detection of trichomonas, it is necessary to resort to repeated repeated studies in all patients using all available laboratory diagnostic methods. All of these examination methods complement each other. Their combination dramatically increases the detection of Trichomonas vaginalis.
Treatment Treatment of genitourinary trichomoniasis is one of the urgent and serious tasks facing doctors all over the world, which is due to the high incidence of this infection, the lack of a guaranteed etiological cure for trichomoniasis and the significant proportion of post-trichomoniasis complications. Modern methods of treating trichomoniasis are based on the use of specific anti-trichomoniasis drugs. When treating trichomoniasis, the following principles must be observed:
- treatment is carried out simultaneously for both sexual partners;
- During treatment, sexual activity and alcohol consumption are not recommended;
- factors that reduce the body's resistance (concomitant diseases, hypovitaminosis) are eliminated;
- Patients with all forms of the disease are subject to treatment (including Trichomonas carriers and patients with inflammatory processes in whom Trichomonas are not detected, but these pathogens are detected in a sexual partner);
- local treatment is prescribed simultaneously with systemic drugs;
- control of cure is carried out 1 week after the end of treatment, then after the next menstruation.
The main principle of treatment of genitourinary trichomoniasis is an individual approach to the patient, based on a thorough analysis of the anamnesis and a comprehensive clinical and laboratory examination. One of the most effective general drugs for trichomoniasis is metronidazole. Before the discovery of metronidazole, therapy for genitourinary trichomoniasis was often unsuccessful and was limited to the use of external agents. Preparations from various acids were used: lactic, boric, etc., as well as hypertonic solutions of table salt, magnesium sulfate, sublimate, and various soaps (tar, baby, sulfur). This treatment was ineffective and contributed to the transition of trichomoniasis to a chronic form, a wider spread of this infection and an increase in the number of complications. Despite the huge number and wide distribution of nitroimidazole drugs, metronidazole is used more often and is actually the main one in the treatment of Trichomonas infection. Metronidazole acts not only on protozoa, but also on anaerobic flora. In addition, metronidazole can induce the production of interferon. The minimum inhibitory concentration of metronidazole under aerobic conditions is 1–10 μg/ml, under anaerobic conditions – 0.1–7.0 μg/ml. The majority (76%) of Trichomonas vaginalis strains die at a metronidazole concentration in the medium of 3.0–5.0 μg/ml. Metronidazole concentrations were measured in various body fluids and tissues after oral, rectal, intravaginal and intravenous administration of the drug. When studying the concentration of metronidazole in the blood serum after a single oral dose of 0.5 g, its level after 1, 2, 4, 6, 8 and 12 hours was 14.4, 12.5, 10.1, 8.4, 6.6, 4.8 μg/ml, respectively. The maximum level of metronidazole in the blood is determined after 1–3 hours. Then its decrease is observed. After just 6 hours, the concentration of metronidazole was below 10 μg/ml, i.e. below the upper limit of the minimum inhibitory dose for Trichomonas vaginalis strains. The concentration of metronidazole in the blood serum was determined after its rectal administration in suppositories. The maximum concentration of metronidazole was approximately half the dose observed after oral administration. The duration of reaching the maximum concentration was 4 hours. Slower absorption of the drug was noted. The level of metronidazole in the blood serum was studied after intravaginal administration of this drug in tablet form. The maximum concentration of metronidazole in the blood when 0.5 g of the drug was administered was 1.63 μg/ml, i.e. 20% of the maximum concentration achieved after oral administration. Absorption was very slow, and the maximum concentration was determined only after 4-8 hours. The concentration of metronidazole in the blood serum after intravenous administration was the same as after oral administration. Thus, the most acceptable method of administering metronidazole to the body is oral. Complex therapy is required: oral administration must be combined with local administration. For example: metronidazole tablets 250 mg + metronidazole vaginal tablets 500 mg. Just as many bacteria, as a result of adaptive reactions, began to produce penicillinase, which makes them insensitive to penicillins, some strains of urogenital trichomonas began to show 10 times less activity to metronidazole drugs. In this regard, reports began to appear about the ineffectiveness of treatment for trichomoniasis due to the resistance of urogenital trichomonas to conventional therapeutic doses of metronidazole. The researchers concluded that strains with lower sensitivity are more often isolated from patients with a latent or erased clinical picture of the disease or from women already treated with metronidazole. Most likely, treatment failures are due to the low concentration of the drug in the foci of infection, its irregular use, and low dosage. For the treatment of genitourinary trichomoniasis, a wide variety of methods have been proposed, differing in the use of both single and course doses, intervals between doses and duration of treatment. However, etiological cure is not guaranteed when using existing regimens. Relapse rates range from 2.2 to 44.1. There are several methods of treatment with metronidazole. When treating fresh, uncomplicated genitourinary trichomoniasis, the following regimens are recommended: 1) Metronidazole 250 mg 2 times a day (in case of a complicated course, you can add another dose of metronidazole 250 mg) + metronidazole, vaginal tablets, 500 mg. The duration of this course is 7–10 days. 2) Metronidazole at a dose of 2 g (8 tablets of metronidazole 250 mg for 1 day). Vaginal metronidazole tablets 500 mg at night can be added to the course of treatment for local action. In the torpid and chronic process, due to impaired vascularization with the subsequent development of scar tissue in the affected organs, the morphological structure of the vaginal mucosa is disrupted and protistocidal drugs penetrate into the lesions in a lower concentration, which is insufficient to suppress the parasite, which in turn leads to drug resistance of Trichomonas to prescribed doses. In the treatment of sluggish, chronic, recurrent, complicated genitourinary trichomoniasis, the following treatment regimens are recommended: 1) 7 metronidazole tablets 250 mg (preferably in one dose) + vaginal metronidazole tablet 500 mg at night. Course 3–5 days; 2) 100 ml of metronidazole solution (containing 0.5 g of metronidazole) is administered intravenously over 20 minutes, 3 times a day for 5–7 days; Currently, in addition to metronidazole, a number of other nitroimidazole derivatives are used. Tinidazole Prescribed according to one of the following regimens: 1) 0.5 g every 15 minutes for 1 hour; course dose 2 g; 2) 0.5 g 2 times a day every day for 1 week; 3) 2 g per day once for 2 days, course dose 4 g. Ornidazole Antimicrobial agent for the treatment of infections caused by trichomonas, amoebas, lamblia, anaerobic bacteria, prescribed once 1.5 g or 0.5 g 2 times a day within 5 days; course dose 5 g. Tenonitrazole Capsules 0.25 g, 8 pieces per package. It has an antitrichomocidal and antimycotic effect; 1 capsule is prescribed 2 times a day for 4 days. Nimorazole Prescribed 0.5 g 2 times a day for 6 days or a single dose of 2 g per day (4 tablets). In a chronic, low-grade inflammatory process, the biological and biochemical protective factors of the vagina decrease, the amount of glycogen in the epithelial cells decreases, the rod-shaped flora of the vagina is replaced by coccal flora, the acidity of the environment decreases, and the specific and nonspecific resistance of the body decreases. Therefore, in such forms, the therapeutic effect should be aimed not only at the destruction of Trichomonas, but also at normalizing the vaginal contents and restoring its functional state. In addition, treatment of a chronic process should include nonspecific treatment methods aimed at increasing the patient's body's defenses. For this purpose, for chronic and torpid forms of trichomoniasis, nonspecific immunotherapy (pyrogen drugs, biogenic stimulants, vitreous, aloe, FIBS), vitamin therapy, and proteolytic enzymes are recommended. In women with impaired function of the gonads, hormonal therapy is prescribed. Estrogens increase the overall tone of the body, improve the trophism of the mucous membranes of the genital organs, and transform the reaction of the vaginal environment from alkaline to acidic, unfavorable for the activity of trichomonas. In addition, when studying Trichomonas vaginalis L.Fjld et al. They found specific receptors for estradiol and dehydrotestosterone, with the highest level of receptors found in Trichomonas sensitive to metronidazole.
Proteolytic enzymes Proteolytic enzymes are highly active biological preparations that have necrolytic, fibrinolytic, mucolytic and anti-inflammatory effects. They enhance the effect of antibacterial drugs and reduce the resistance of microflora to them. Proteolytic enzymes enhance the trichomonas activity of metronidazole by 2–10 times. They help accelerate proliferative processes in tissues, activate cellular reactions, and enhance the phagocytic activity of leukocytes. Proteolytic enzymes can be of animal (trypsin, chymotrypsin) and plant (terrilitin) origin. There are commercially available preparations that include other enzymes. The use of these drugs significantly increases the effectiveness of complex therapy, helps reduce relapses of the disease, prevents and reduces the frequency of peritubar adhesions. Crystalline trypsin is prescribed 10 mg once a day intramuscularly for 5 days. Then or simultaneously, etiotropic therapy is carried out. Terrylitin is administered rectally or vaginally at a dose of 600–1000 units 2–3 times a day for 5–10 days. Then or simultaneously, etiotropic treatment is carried out. Administration of terrilitin is continued throughout the course of treatment. Wobenzym is a film-coated tablet that is resistant to gastric juice. It contains: bromelain (45 mg), papain (60 mg), pancreatin (100 mg), chymotrypsin (1 mg), trypsin (24 mg), amylase (10 mg), lipase (10 mg), rutin (50 mg). Prescribe 3 capsules 3 times a day for 1–2 months. Local treatment of trichomoniasis is used in the presence of contraindications to the use of metronidazole, as well as in patients with a torpid recurrent course of the disease. When prescribing local therapy, it is necessary to take into account the stage of the inflammatory process. In acute cases, douching, baths with infusion of chamomile flowers and sage herbs are used. For local treatment of colpitis, use metronidazole 500 mg in the form of vaginal tablets once a day for 10 days. If candidal infection is accompanied, the course of treatment can include new generation antifungal drugs of the fluconazole group; 1 capsule is prescribed once during the course of treatment (which is very convenient, effective and least safe for the patient). If necessary, the capsule can be taken again. Chronic inflammatory process in 89.5% of cases occurs as a mixed infection. Disorders that develop in the body of patients with mixed urogenital infections and are difficult to correct with therapeutic agents contribute to the recurrence of the disease, causing an extremely persistent course of the process, despite the use of fairly effective etiotropic drugs. Metronidazole derivatives affect not only Trichomonas, causing their death, but also the accompanying vaginal gram-negative anaerobic flora (for example, Gardnerella), which contributes to the development of the post-Trichomonas inflammatory process. When combined with candidiasis, it is recommended to add fluconazole drugs to the regimen (discussed above). In the presence of other diseases, antibiotics are prescribed to which the pathogens are sensitive.
Treatment of trichomonas infection during pregnancy In the first trimester of pregnancy during the period of organogenesis and placentation, treatment with protistocidal drugs is not indicated, since as a result of the pathogenic effect of metronidazole in the embryo and fetus, those organs and systems that are in the process of differentiation at this time may be affected primarily . They recommend daily lubrication of the urethra and vagina with a 4% aqueous solution of methylene blue or brilliant green or a solution of potassium permanganate (1:10,000). In the second trimester of pregnancy, it is permissible to use vaginal metronidazole tablets 500 mg (1 tablet at night for 8–10 days), since during this period the redox reactions of the fetus are already developing, associated with the inactivation of drugs. Treatment with metronidazole 250 mg tablets for oral use can only be prescribed in the third trimester of pregnancy. However, it is necessary to take into account the decrease in detoxification and excretory function of the kidneys, characteristic of pregnancy, a slowdown in metabolism and the elimination of chemical compounds from the body. Metronidazole during pregnancy is prescribed in a lower dosage than usual, 0.25 g 2 times a day for 8 days or in combination of metronidazole for oral use 250 mg with metronidazole in vaginal tablets 500 mg; course dose 3–4 g.
Medical examination One of the unresolved problems in the fight against trichomoniasis is the problem of medical examination of patients. According to Order No. 286 of the Ministry of Health of the Russian Federation dated December 7, 1993, work on identifying patients, diagnosing, treating and preventing trichomoniasis can be carried out by doctors in dermatovenerology clinics, obstetrics, gynecology, urology and other treatment and preventive institutions. The cure of genitourinary trichomoniasis is established using bacterioscopic and cultural research methods. The first control studies in women are carried out 7–8 days after the end of treatment. If necessary, a provocation is carried out: an injection of gonovaccine (500 million microbial bodies) or pyrogenal (200 MTD) and after 24, 48 and 72 hours the discharge of the urethra, vagina, and rectum is examined. The second control examination is carried out immediately after the next menstruation. Material for research must be taken from all lesions. A patient with trichomoniasis is under medical supervision to establish cure after completion of treatment for fresh trichomoniasis for 2 months, for chronic trichomoniasis for 3 months. For patients with an unidentified source of infection, the period of follow-up observation is increased to 6 months. At the same time, monthly clinical and serological examinations are carried out to detect syphilis, since metronidazole has treponemocidal properties and can complicate its diagnosis.
Cure criteria:
- absence of trichomonas when examining discharge from the urethra, urethra, vagina, rectum;
- favorable results of clinical and laboratory studies during 2–3 menstrual cycles;
- absence of clinical manifestations of Trichomonas infection.
Taking into account the criteria for cure, if the results of clinical and laboratory tests are favorable, patients are removed from the register.
Prevention Preventive measures for trichomoniasis should be aimed at timely and complete identification of women infected with Trichomonas. These include:
- identification and treatment of patients with trichomoniasis;
- identification, examination and treatment of sexual partners;
- examination for the presence of trichomoniasis of all persons suffering from inflammatory diseases of the genitourinary organs;
- periodic examination for the presence of trichomoniasis of persons working in children's groups, hospitals, maternity hospitals;
- sanitary and hygienic measures
previous article
Polpharma supports young scientists from all over the world
next article
Pharmacology of the enteric form of acetylsalicylic acid
Top
Types of colpitis
Depending on the cause of colpitis, several types can be distinguished. Each form of the disease has different manifestations, recovery time and risks of complications, so the approach to treatment must be selected individually.
Candidiasis colpitis
A type of infection called thrush is caused by the fungus Candida. These fungi can live in the body for years without causing any discomfort, and certain factors can trigger their intensive growth and lead to inflammation. Candida colpitis occurs both as a result of unprotected sex and with weakened immunity, dysbacteriosis, and antibacterial therapy.
Atrophic colpitis
Most often they appear in women after the onset of natural menopause, when the amount of estrogen decreases, due to which the vaginal epithelium becomes insufficiently moisturized, it becomes thinner, and microcracks appear. For a woman, colpitis is accompanied by a lot of discomfort, dryness, itching, and pain during sexual intercourse.
Atrophic colpitis can also occur in girls who have undergone surgery to remove the ovaries or uterus, and after taking certain medications.
Trichomonas colpitis
Associated with infection by the microorganism Trichomonas vaginalis. Transmission of the infection occurs during sexual intercourse with an infected partner without the use of barrier contraception.
At an early stage of development of the disease, it is easily diagnosed and treated. But an advanced stage can lead to chronicity of the disease, the cure of which is a big problem. In this case, periods of exacerbation are replaced by short periods of remission.
Trichomonas colpitis is dangerous because, in the absence of competent and timely treatment, it leads to dangerous complications, including infertility.
Infectious agents
In the case of a specific nature of the disease, the causative agents are sexually transmitted infections, and in the case of a nonspecific nature - opportunistic microflora.
Among the factors that provoke opportunistic microorganisms to become pathogens, the following can be identified:
● Frequent use of panty liners;
● Wearing underwear made of artificial materials;
● Tight clothing that does not allow ventilation of the genitals;
● Failure to maintain regular intimate hygiene;
● Weakening of the body’s immune defense due to stress, taking antibiotics, vitamin deficiency, and malnutrition;
● Abortion;
● Diabetes mellitus;
● Postmenopausal period.
Treatment methods
Trichomonas are often found in association with other pathogenic microorganisms, so treatment is aimed at suppressing all infections.
Therapy begins immediately after receiving positive test results. Medicines should be taken by both sexual partners, even if the man has no signs of infection. The exception is women in the 1st trimester of pregnancy, since during this period the placenta, which can protect the fetus from the negative effects of antibiotics, has not yet formed. If possible, treatment is shifted to the 2nd or 3rd trimester.
Systemic therapy
Monotherapy for trichomonas colpitis is used very rarely. Systemic treatment allows not only to stop the process of active life of parasites, but also to create conditions for restoring the body’s immune defense.
This table shows the groups of drugs that are used for Trichomonas colpitis.
| Group of drugs | Name | Action |
| Antibiotics | Metronidazole, Nitazole, Ornidazole | They destroy not only Trichomonas, but also other bacteria. |
| Suppositories (candles) | Trichomonacid, Terzhinan | They relieve inflammation and have an antiprotozoal effect (destroy the DNA structure of parasites). |
| Antitrichomonas drugs | Trichopolum, Fazizhin (in tablets), Furazolidone (for irrigation) | Effective against monoinfection. |
| Antiseptics | Miramistin (for washing the genitals) | Relieves inflammation and disinfects. |
| Immunostimulating agents | Immunal | Helps strengthen the immune system. |
| Antagonists | Bifidumbacterin | Restores the balance of vaginal and intestinal flora. |
It is undesirable to use folk remedies, since the prognosis of treatment will be uncertain. The disease does not go away on its own. If you have symptoms of Trichomonas colpitis, you should definitely consult a doctor and start therapy immediately!
Read more about the treatment of trichomonas colpitis
Symptoms
Signs of this disease can be very different, depending on the cause of its occurrence and the stage of development. In later stages, the patient may experience increased body temperature, headaches, and general malaise. And at the initial stage of the disease, the most common manifestations are vaginal odor, unhealthy discharge, and painful sensations both during sexual intercourse and in everyday life.
Vaginal discharge
Vaginitis discharge is in no way related to the phase of the menstrual cycle. With candidiasis, they are white in color and have a heterogeneous cheesy texture. Trichomoniasis is characterized by gray-green discharge, and in the bacterial form it is foamy and has a uniform consistency.
Smell
Often a sign of the proliferation of pathogenic microflora in the vagina is odor. It may vary depending on the specific type of microorganism. Its appearance is due to the fact that in the process of life, bacteria decompose various substances, releasing gas, which in turn has an odor.
Pain
When the vaginal walls are inflamed, they often experience pain during sexual intercourse. Pain can also occur when urinating, when substances contained in the urine irritate the already irritated mucous membranes. Often women complain of the presence of burning and itching, and the pain is characteristic of inflammation as a result of mechanical damage.
Trichomonas vaginitis, colpitis
Damage to the genitourinary organs caused by the urogenital trichomonas Trichomonas vaginalis. Rare cases of extrasexual infection occur in girls who become infected through objects contaminated with the secretions of patients (napkins, towels, intimate toiletries, etc.). Usually infection occurs through sexual contact.
Due to the common path of spread with gonococci, urogenital trichomonas often cause a mixed infection, detected in the form of post-gonorrheal vaginitis and endocervicitis. In girls, urogenital trichomonas cause only vulvovaginitis, and in women - urethritis, bartholinitis, colpitis and endocervicitis. Due to insufficient production of antibodies, immunity does not develop and re-infection with trichomoniasis is possible.
Clinical picture
The incubation period lasts on average from 3 to 12-15 days, but can last up to a month. According to the course, fresh trichomoniasis, chronic and trichomonas carriage are distinguished. In girls, symptoms of vulvovaginitis predominate with foamy, mucous-serous discharge, causing itching and burning of the external genitalia. In torpid and chronic cases, hyperemia of the mucous membrane of the external genitalia and vagina may be absent, discharge is scanty, and subjective disorders are often absent. The cervix and urethra may be involved in the process.
Treatment of trichomonas vaginitis, colpitis
For all forms of Trichomonas vaginitis, specific anti-Trichomonas drugs are prescribed: metronidazole, tinadazole, etc. In complicated and chronic cases, complex treatment is used. In addition to taking metronidazole, nonspecific immunotherapy and local procedures are prescribed.
Criterion for cure of trichomonas vaginitis, colpitis
Determined within 3 months. The first control is carried out 7-10 days after the end of therapy. In menstruating girls, subsequent studies are carried out over 3 menstrual cycles. Girls are examined monthly for 3 months. In the absence of trichomonas in smears and inflammatory changes in the genitourinary organs, those who have had trichomoniasis are removed from the register.
Diagnosis of the disease
When diagnosing colpitis, the doctor’s task is not only to identify the disease, but also to determine the factor that provoked its appearance. Usually, already at the first appointment, a gynecologist can suspect the disease based on the patient’s complaints and examination in the gynecological chair.
For a more accurate diagnosis, colposcopy, ultrasound of the pelvic organs, and rectal examination are performed to detect various neoplasms in the rectum. A vaginal smear for cytology will determine the nature of the inflammatory process, and with the help of bacteriological analysis, a specific type of microorganism can be identified.
If necessary, the doctor also prescribes a general blood and urine test and a blood test for hormones.
How to protect yourself from infection
The consequences of infection caused by Trichomonas are dangerous not only for women of reproductive age, but also for men, as they affect sperm quality and erectile function. To protect yourself from infection, you must have sex with one partner or protect yourself with condoms.
To prevent Trichomonas colpitis, it is recommended to undergo regular examinations with a gynecologist and venereologist, and promptly treat other STIs.
To make an appointment or get advice, call the 24-hour number
+7
or fill out the form
Prevention
To prevent colpitis, a number of rules should be followed:
● Regular examinations by a gynecologist to identify disorders in the initial stages of their occurrence.
● Caring for the vaginal lining, including maintaining personal hygiene, frequent changes of underwear, and proper use of toilet paper.
● Taking antibacterial agents exclusively as prescribed by a doctor and, if necessary, combining them with taking medications that will maintain the microflora of the mucous membrane in a normal state.
● Strengthening the immune system.
Diagnostics
The presence of Trichomonas in the genital tract must be proven by detection under a microscope or by growing it in a special nutrient medium.
They specifically look for Trichomonas vaginalis in women who complain of discharge from the genital tract, with long-term and drug-resistant inflammation of the vaginal mucosa, and, of course, in the risk group. A swab is taken from the genital tract and immediately examined under a microscope. For men, urine or discharge from the penis is tested.
If trichomoniasis is detected, then it is worth checking for other sexually transmitted diseases: it is quite possible that they were transmitted at the same time as trichomoniasis.
Growing the pathogen in a nutrient medium is a more effective method for detecting Trichomonas vaginalis, but even better - 100% results are obtained by polymerase chain reaction - PCR, which detects Trichomonas DNA.
Treatment of colpitis
Proper treatment should include not only eliminating disturbing symptoms, but also getting rid of the cause of the pathology. The latter falls within the purview of etiotropic therapy. It is based on the use of antifungal, antibacterial or antiviral drugs.
To treat nonspecific colpitis, combination medications are prescribed to kill several types of infections. Local therapy consists of the external use of various antiseptics and other medications in the form of douching or moistened vaginal tampons.
Do not forget that if vaginitis is associated with the acquisition of an infectious agent through sexual contact with an infected partner, both partners must be treated at the same time.
It is recommended to abstain from sexual intercourse during therapy until complete recovery.
Is this a peaceful carrier?
Why someone develops violent symptoms of damage to the genital tract by Trichomonas, and someone does not even suspect that the protozoa is present, cannot be said with certainty. Most likely, this is due to both the ciliate strain and the characteristics of the host. But in men this state of clinical affairs is observed an order of magnitude more often than in women.
It is assumed that the immune response to the introduction of Trichomonas can be very sluggish, because its genes are somewhat similar to red blood cells - erythrocytes. Or perhaps, on the contrary, the local immunity is so strong that it is not capable of completely killing Trichomonas vaginalis, but does not allow it to go away, not allowing it to actively manifest itself.
However, the absence of clinical symptoms does not make the carrier harmless to a sexual partner; he is the same source of infection as a person who recognizes himself as having a sexually transmitted infection. Trichomonas carriers are dangerous because, not feeling a venereal disease, they do not consider it necessary to limit their sexual behavior. It is to Trichomonas carriers that we owe a fairly significant spread of the disease.
Carriage of Trichomonas allows for much easier infection with other sexually transmitted infections and HIV, since the protective properties of the mucous membrane with trichomoniasis are lower, damage occurs in the mucous membrane of the genital organs, through which other pathogens easily penetrate. There is a suspicion that although Trichomonas itself rarely affects the cervical canal, it increases the likelihood of developing not entirely benign changes in the cervical mucosa - cervical neoplasia.
Why is colpitis dangerous?
Colpitis is not a dangerous disease if treatment is started in a timely manner. If a woman neglects medical care, the disease can become chronic, which will significantly worsen the quality of life.
If vaginitis is not treated correctly, it can develop into endometritis, urethritis or cervical erosion. Also, bleeding microcracks on the walls of the vagina serve as open gates for the acquisition of new pathogenic microorganisms, complicating the treatment process.
Diet for colpitis
Following a diet for colpitis makes it possible to strengthen the immune system and speed up the process of restoration of damaged mucous membranes. During treatment, a woman should consume:
- food products that contain polyunsaturated acids (tuna, cod, shrimp);
- dairy products;
- vegetables, grains, fruits.
You should avoid heavy foods (fatty, fried) and alcohol. They interfere with the normal functioning of the liver, contribute to the exacerbation of chronic diseases, which ultimately leads to inhibition of the recovery process in the vaginal mucosa.
Treatment regimen for Trichomoniasis
The pathogen is effectively affected by drugs from the 5-nitromidazoles group:
- Metronidazole is taken 500 g 2 or 3 times for 7 days. The doctor may prescribe a single dose of the drug for 1 or 5 days, depending on the severity of the disease.
- Tinidazole or ornidazole is also used for treatment. The dose is selected individually. Metronidazole and ornidazole are also prescribed to children.
Important! Self-medication most often leads to the disease becoming latent. Therefore, at the first signs of pain and discomfort, you should consult a specialist. Self-medication can be dangerous to a woman's health.
Causes of Trichomonas colpitis
Most often, trichomonas are transmitted from a partner during sexual intercourse. Having established itself on the mucous membrane, the microorganism begins to multiply rapidly, gradually infecting new cells.
Cases have been recorded in which the infection passed from mother to fetus during pregnancy and childbirth. In addition, since trichomes live up to 3 hours in a humid external environment, the source of infection can be a bathtub, toilet rim, sauna, swimming pool, hygiene items, and joint water procedures. However, the household method of spreading infection is extremely rare.
Factors that increase the risk of infection:
- promiscuous sexual intercourse,
- ignoring barrier contraception,
- the presence of diseases of the vagina and vulva, for example chlamydia, genital herpes, etc.,
- pathologies of the endocrine system,
- chronic fatigue,
- constant nervous tension,
- reduced immunity,
- consequences of taking certain medications.