From ancient Greek, the word “coma” is translated as “deep sleep.” In the myths of those distant times, the god of sleep, Hypnos, was called the brother of Thanatos, the messenger and personification of death. In modern medicine, “deep sleep” in a coma is also considered borderline and near-death.
In this state, consciousness is lost, reflexes fade, the frequency and depth of breathing is disrupted, the pulse and vascular tone change abnormally, and the mechanisms of temperature regulation are disrupted.
What causes coma?
The coma is caused by impaired blood circulation in the brain and/or toxic damage to the cells of the central nervous system. These pathologies arise for the following reasons:
- head injuries;
- drowning, suffocation, cardiac arrest;
- stroke;
- decompensated diabetes mellitus;
- meningitis, encephalitis;
- kidney or liver dysfunction as a result of poisoning or disease;
- epileptic seizures that follow one after another.
In addition, there is an artificial medical coma. It is used as an alternative to anesthesia if a neurosurgical operation is performed, as well as when the patient is brought out of an epileptic state.
Consequences of coma
Traumatic brain injuries are considered the most dangerous due to their consequences on the nervous system. A comatose state only aggravates the situation, since some brain cells die off, and other areas must take over their functions. In addition, the consequences of a coma after a traumatic brain injury may not appear immediately, but some time after recovery from this state.
All consequences can be divided into several groups:
- Impaired cognitive functions. It occurs even with a mild degree of coma, when, some time after leaving this state, confusion periodically occurs. Due to the fact that the blood supply to the brain is affected, mental abilities deteriorate. In severe cases, hearing and vision may deteriorate during the recovery period. Some patients experience amnesia. A person quickly gets tired of any mental activity;
- Deterioration of speech skills. In severe cases, speech function can be lost completely, sometimes even swallowing skills are affected. But even with mild degrees, speech can become inarticulate;
- Deterioration of motor skills and function of the musculoskeletal system. It all depends on the degree of brain damage due to injury. Sometimes the problems are limited to impaired coordination of movement; in more serious cases, the patient suffers from limb cramps and loss of sensitivity. In the most difficult situations, paralysis occurs;
- The appearance of pain syndrome. Even with mild brain damage, patients may experience chronic headaches;
- The psychological state of the patient worsens, since the person has a hard time experiencing what is happening to him - headaches, and partial loss of previous skills. He becomes irritable and even aggressive, and may become depressed.
Most of the listed consequences can be eliminated after a long rehabilitation period. But there are serious complications that are almost impossible to cope with; you can only improve the patient’s quality of life - these are chronic cephalalgia, the development of epilepsy, etc.
Depth of coma
A comatose state can develop gradually over several days, or occur suddenly in a matter of minutes. According to the degree of depth, the following stages of coma are distinguished:
- Precoma with severe retardation or, on the contrary, psychomotor agitation. Reflexes are preserved, coordination of movements is impaired, thinking suffers.
- The first degree, in which sleep or stupor occurs. Reactions to external stimuli are inhibited, but the person can take liquid food and make simple movements.
- Second degree, the stage of deep sleep with a complete lack of contact, pathological forms of breathing, rare chaotic movements, weakened pupillary response to light, convulsive muscle twitching.
- The third degree, in which there is no consciousness, there is no reaction to painful stimuli, reflexes are lost, the normal breathing rhythm is lost, blood pressure drops, and body temperature decreases.
- The fourth degree or extreme coma, in which reflexes disappear, muscle tone is absent, and blood pressure and temperature drop sharply. Spontaneous breathing stops. It is supported by artificial ventilation, and nutrients are injected.
Death most often occurs in a state of extreme coma. However, if a person can be brought out of it, and further improvement occurs, then brain functions can be restored partially or completely.
Treatment
Treatment is a complex, comprehensive process that must prevent death, maintain vital body functions, and at the same time combat the root cause of this condition.
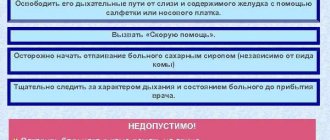
The first resuscitation measures aimed at preserving a person’s life are carried out immediately upon the arrival of the ambulance team and during transportation of the patient, before all diagnostic procedures are carried out. First aid consists of fixing the patient's position, ensuring patency of the airway - straightening the tongue, clearing the nose and mouth of vomit, an oxygen mask, tracheotomy with the installation of a breathing tube. It is necessary to normalize blood circulation by administering medications that normalize cardiac activity and blood pressure. If necessary, indirect cardiac massage is performed.
In the intensive care unit, the patient is connected to an artificial respiration apparatus. Medicines are administered aimed at eliminating the pathological symptoms of the disease - anticonvulsants, antipyretics, hemostatics. Intravenous infusions of glucose and saline solutions are required. Measures are necessary to normalize body temperature. In case of hypothermia, the patient is covered and covered with hot water bottles. If there is a suspicion of poisoning with chemical or pharmacological drugs, gastric lavage is performed.
At the second stage, having detailed results of all types of examinations, the cause is eliminated. In case of hyperglycemic coma, measures are taken to normalize blood sugar and insulin levels. In case of renal failure, hemodialysis is performed. If an injury, hematoma or brain tumor is detected, urgent or planned surgical intervention is performed according to indications.
Communicating with a person in a coma
Those who managed to come out of a coma say that they felt as if they were in an extremely deep sleep. Some report that very near-death tunnel, at the end of which a bright light was visible. Almost everyone remembers nothing about the events that led to the coma, and, moreover, about what happened to them in this state.
However, although comatose patients have no reaction to external stimuli, there is reason to believe that some forms of subconscious perception still remain. Therefore, the British Department of Health has made the following recommendations for those visiting a relative, loved one or friend who is in a coma:
- Introduce yourself and share the news in a positive way.
- Talk about your current life as if the person in a coma were an ordinary interlocutor, or rather, a listener.
- Show your support. To do this, just sit next to him and hold the person’s hand.
- Let him listen to his favorite music using headphones.
Causes
The most common cause of hepatic coma is a pre-existing liver disease that is in the stage of decompensation. Liver diseases such as:
- cirrhosis of various origins (alcoholic, viral, stagnant);
- hepatosis (fatty, pigmented);
- hepatitis (alcoholic, viral, toxic, drug);
- malignant neoplasms (hepatocellular carcinoma, mixed cancer);
- inherited liver pathologies (Gilbert syndrome, Konovalov-Wilson disease).
Risk factors for the development of pathology are:
- poisoning with toxic substances (arsenic, phosphorus, alcohol, mushrooms);
- hepatotoxic effect of certain drugs (barbiturates, nitrofuran);
- excess protein-rich foods in the diet;
- severe stressful conditions;
- chronic intestinal obstruction;
- performing heavy abdominal operations;
- sepsis.
The causes of the precursors and symptoms of hepatic coma remain unknown in 17% of cases.
Rehabilitation after a coma
To bring a patient out of a coma, doctors make many attempts, and this process takes an indefinite amount of time. If persistent efforts are successful, the person’s consciousness returns, the mood for recovery is formed, and rehabilitation is carried out under the supervision of specialists.
For this purpose, targeted centers with multifaceted rehabilitation programs are created. In the Minsk region, one operates in the Aksakov region. Those who require specialized assistance are there free of charge.
Rehabilitation course: main features
Until relatively recently, the possibilities for rehabilitation after such a condition were limited. In recent years, centers have been opened in which patients undergo recovery from TBI. This is a whole complex of events. It involves:
- neurologists who help restore central nervous system functions;
- physiotherapists who carry out procedures to restore muscle tone select treatment to eliminate headaches;
- psychologists who help the patient overcome apathy, adapt to a new stage of life and return to society. The patient’s relatives may also need the help of a psychologist;
- neurospeech therapists who restore speech function, etc.
Rehabilitation programs are developed taking into account the patient's condition. Rehabilitation is carried out in specialized centers that collaborate with highly specialized doctors. For example, occupational therapists help patients regain self-care skills, including driving a car. These doctors also conduct classes on the development of motor skills. Kinesiotherapists work to restore the functioning of the musculoskeletal system and normalize coordination of movements. The actions of all doctors are supervised by a rehabilitation specialist.
Physical therapy classes are required, including on simulators designed for this purpose. Breathing exercises play an important role, since the lungs in coma suffer as much as the brain. To restore muscle tone, swimming in the pool and various water procedures are recommended.
We carefully select a unique therapy, taking into account all the complications of the patient’s condition, and therefore show highly effective results. An individual approach to each of our patients is a distinctive feature of the Evexia center and the staff working there.
How is it determined that coma has turned into death?
Modern medicine is able to maintain breathing, cardiac activity and provide nutrition for a long time to a person in a deep coma. Death is declared when blood flow to the brain stops and irreversible pathological changes occur.
These changes are diagnosed using computed tomography or magnetic resonance imaging. The absence of any brain activity is determined by electroencephalography methods, and cessation of cerebral circulation is recorded angiographically.
Based on the totality of the obtained indicators, death is diagnosed and, in agreement with relatives, life support equipment is turned off.
Duration of coma
The duration of a coma can be very different: from several hours to several days or weeks. Some patients die without regaining consciousness. Rarely does a patient remain in a coma for several months, a year, or more. But the chances of recovery after such a long coma are extremely low.
A quick exit is more likely when:
- moderate area of necrosis;
- ischemic nature of stroke;
- partial preservation of reflexes;
- young age of the patient.
Question and answer
Does it happen that a patient comes to his senses after he has been declared brain dead?
Such cases do happen. For example, on December 23, 2011, doctors definitely and objectively confirmed the brain death of 21-year-old American student Sam Schmidt, who fell into a deep coma after an accident. Sam's parents were advised to think about consenting to the removal of their son's organs for transplantation, and an hour later a consultation was to be held on the issue of turning off the equipment that supports life in his body. Suddenly Sam moved his fingers, began to respond to calls and woke up.
How to get to the rehabilitation center in Aksakovshchina?
From the metro station "Pushkinskaya", "Kamennaya Gorka" by minibus 1203 TK, from the railway station, metro station "Kamennaya Gorka" - by minibus 1500 TK.
Do the Belarusian media publish information about those who came out of a coma, about what they felt?
The most recent publication with such interviews was on the TUT.BY website in the “Health” section on May 20, 2021.
Life prognosis for liver cirrhosis
Hepatic coma often occurs with cirrhosis of the liver, so the question arises how long people live with this disease. Survival depends on a number of factors: the age of the patient, his general condition, and the presence of concomitant diseases.
Survival rates for cirrhosis are quite high: about 50% of all patients live more than 7 years. But, if the disease is not in a compensated state, then the survival rate for a period of 5 years is about 40%. For ascites complicated by cirrhosis, the survival rate is 25% at 3 years. With hepatic encephalopathy, the patient lives no more than 1 year.
The life prognosis for hepatic coma in liver cirrhosis is extremely unfavorable: less than 20% of patients survive.
The most severe prognosis for hepatic coma is expected with severe respiratory failure, increased levels of bilirubin in the blood, and the addition of an infection.
How long do children live with end-stage hepatic coma? Age under 10 years is a factor that increases the risk of death.