Traumatic brain injury is damage to the bones of the skull and/or soft tissues (meninges, brain tissue, nerves, blood vessels). Based on the nature of the injury, a distinction is made between closed and open, penetrating and non-penetrating TBI, as well as concussion or contusion of the brain. The clinical picture of traumatic brain injury depends on its nature and severity. The main symptoms are headache, dizziness, nausea and vomiting, loss of consciousness, memory impairment. Brain contusion and intracerebral hematoma are accompanied by focal symptoms. Diagnosis of traumatic brain injury includes medical history, neurological examination, skull x-ray, CT or MRI of the brain.
ICD-10
S06 Intracranial injury
- Causes
- Classification
- Concussion Symptoms
- Diagnosis
- Treatment
- Symptoms
- Symptoms
- Symptoms
- Conservative therapy
Main causes and types of injuries in the skull area
The pathologies under study can arise as a result of many factors, for example, during road traffic accidents, human falls from a height, at work and at home, during active sports.
Content:
- Main causes and types of injuries in the skull area
- Clinical course of the pathology
- First aid
The main types of traumatic brain injuries include closed, open and penetrating injuries to the head. The closed type of such injuries include those in which the aponeurosis remains without damage, but there are injuries or bruises to the head in the soft tissue section. Open craniocerebral injuries are characterized by damage to the aponeurosis and integrity of the skin on the head. Experts consider penetrating injuries to be those that result in disruption of the integrity of the dura mater of the brain.
General information
Traumatic brain injury is a collective concept that includes various injuries to the bone and soft structures of the head. The following clinical forms of TBI are distinguished: concussion, brain contusion, diffuse axonal damage, brain compression. The most common possible traumatic brain injury (about 70% of all TBIs) is a concussion. Mild brain contusion is diagnosed in 10-15% of victims with traumatic brain injury, moderate severity is diagnosed in 8-10% of victims, severe contusion is diagnosed in 5-7% of victims.
Traumatic brain injury (TBI)
Clinical course of the pathology
More often than others, with traumatic brain injuries, a concussion occurs without macrostructural lesions. Brain damage at the cellular level is reversible and treatable. The main symptoms of a concussion are loss of consciousness for a short time, nausea and vomiting, dizziness, headaches, double vision, sweating, memory loss. From a neurological point of view, there is a violation of symmetry in tendon reflexes, small-scale nystagmus, which under normal conditions disappears a week after the injury. If the victim undergoes a computer or magnetic resonance imaging scan, they will not reveal any pathologies.
With traumatic brain injuries, brain contusion can occur. This pathology leads to hemorrhages and destruction (gross macrostructural disorders) in the brain, accompanied by subarachnoid hemorrhage. Often a brain contusion is accompanied by a fracture of the skull bones. All this together can lead to swelling of the brain.
Manifestations of brain contusion by severity:
- Mild degree - the patient’s loss of consciousness can last up to 20 minutes, after which dizziness, vomiting and nausea, headaches, anterograde or retrograde amnesia occur. Vital functions remain unchanged; cardiovascular changes in the form of hypertension or bradycardia may occur. Neurological symptoms include pyramidal insufficiency, clonic nystagmus, and slight anisocoria.
- In the middle stage, the patient’s unconscious state lasts for several hours, after which severe memory loss occurs, repeated vomiting occurs, and mental health is impaired. Vital functions are impaired, persistent bradycardia, tachypnea with preservation of airway patency, hypertension. From a neurological point of view, nystagmus, imbalance in tendon reflexes and muscle tone, and various meningeal signs are observed. Focal manifestations in the form of ocular and pupillary disorders, changes in speech, and paresis of the limbs are also obvious.
- In severe cases, the patient falls into a coma, which, if not fatal, can last several weeks. Severe violations of vital functions pose a threat to life. The movements of the eyeballs are floating, the rhythm and frequency of breathing are disturbed, bilateral miosis or mydriasis, and convulsions occur. With such traumatic brain injuries, there are fractures of the skull bones in combination with massive subarachnoid hemorrhage.
Compression of the brain substance may occur due to intracranial hematomas that form above or below the soft membrane.
Clinically, compression can manifest itself in the same way as a bruise, but it has a very dangerous consequence. After the victim returns to consciousness, he usually feels better, but this does not last long, until the intracranial hematoma grows in size and begins to compress the brain. After this, the person falls into a coma again, and the prognosis for this state is rarely satisfactory. The functioning of the respiratory and vascular centers is disrupted.
Causes
According to the genesis and mechanism of occurrence, TBI can be primary (the impact of traumatic mechanical energy on the brain is not preceded by any cerebral or extracerebral catastrophe) and secondary (the impact of traumatic mechanical energy on the brain is preceded by a cerebral or extracerebral catastrophe). TBI in the same patient can occur for the first time or repeatedly (twice, three times).
- Primary lesions are focal contusions and crushes of the brain, diffuse axonal damage, intracranial hematomas, brainstem ruptures, multiple intracerebral hemorrhages resulting from mechanical head trauma.
- Secondary lesions arise as a result of the action of secondary intracranial factors (delayed hematomas, disturbances of liquor and hemocirculation due to intraventricular or subarachnoid hemorrhage, cerebral edema, hyperemia, etc.) or secondary extracranial factors (arterial hypertension, hypercapnia, hypoxemia, anemia, etc.)
Complications
Violations of vital functions - a disorder of the basic life support functions (external respiration and gas exchange, systemic and regional circulation). In the acute period of TBI, the causes of acute respiratory failure (ARF) are dominated by pulmonary ventilation disorders associated with impaired airway patency caused by the accumulation of secretions and vomit in the nasopharynx with their subsequent aspiration into the trachea and bronchi, and retraction of the tongue in comatose patients.
Dislocation process: temporotentorial inclusion, representing a displacement of the mediobasal sections of the temporal lobe (hippocampus) into the fissure of the tentorium of the cerebellum and herniation of the cerebellar tonsils into the foramen magnum, characterized by compression of the bulbar sections of the trunk.
Purulent-inflammatory complications are divided into intracranial (meningitis, encephalitis and brain abscess) and extracranial (pneumonia). Hemorrhagic - intracranial hematomas, cerebral infarctions.
Classification
The classification of TBI is based on its biomechanics, type, type, nature, shape, severity of injury, clinical phase, treatment period, and outcome of the injury.
Based on biomechanics, the following types of TBI are distinguished:
By type of damage:
- focal (characterized by local macrostructural damage to the brain matter, with the exception of areas of destruction, small and large focal hemorrhages in the area of impact, counter-impact and shock wave);
- diffuse (tension and spread of primary and secondary axonal ruptures in the centrum semiovale, corpus callosum, subcortical formations, brain stem);
- combined (a combination of focal and diffuse brain damage).
Based on their type, TBIs are classified into:
- closed - damage that does not violate the integrity of the scalp; fractures of the bones of the calvarium without damage to the adjacent soft tissues or a fracture of the base of the skull with developed liquorrhea and bleeding (from the ear or nose);
- open non-penetrating TBI - without damage to the dura mater and open penetrating TBI - with damage to the dura mater.
In addition, isolated (absence of any extracranial damage), combined (extracranial damage as a result of mechanical energy) and combined (simultaneous exposure to various energies: mechanical and thermal/radiation/chemical) traumatic brain injury are distinguished.
Based on severity, TBI is divided into 3 degrees: mild, moderate and severe. When correlating this rubric with the Glasgow Coma Scale, mild traumatic brain injury is assessed at 13-15, moderate at 9-12, severe at 8 points or less. A mild traumatic brain injury corresponds to a mild concussion and contusion of the brain, a moderate one corresponds to a moderate brain contusion, a severe one corresponds to a severe brain contusion, diffuse axonal damage and acute compression of the brain.
The course of TBI is divided into 3 basic periods: acute, intermediate and long-term. The duration of the periods of traumatic brain injury varies depending on the clinical form of TBI: acute - 2-10 weeks, intermediate - 2-6 months, long-term with clinical recovery - up to 2 years.
There are several main types of interrelated pathological processes:
- direct damage to the brain substance at the time of injury;
- cerebrovascular accident;
- violation of liquor dynamics;
- disorders of neurodynamic processes;
- formation of scar-adhesive processes;
- autoneurosensitization processes.
The basis of the pathological picture of isolated brain injuries is primary traumatic dystrophies and necrosis; circulatory disorders and organization of tissue defect. Concussions are characterized by a complex of interconnected destructive, reactive and compensatory-adaptive processes occurring at the ultrastructural level in the synaptic apparatus, neurons, and cells.
Brain contusion is an injury characterized by the presence in the substance of the brain and in its membranes of macroscopically visible foci of destruction and hemorrhage, in some cases accompanied by damage to the bones of the vault and base of the skull. Direct damage to the hypothalamic-pituitary, brainstem structures and their neurotransmitter systems during TBI determines the uniqueness of the stress response. Impaired metabolism of neurotransmitters is the most important feature of the pathogenesis of TBI. Cerebral circulation is highly sensitive to mechanical influences.
The main changes that develop in the vascular system are expressed by spasm or dilation of blood vessels, as well as increased permeability of the vascular wall. Directly related to the vascular factor is another pathogenetic mechanism for the formation of the consequences of TBI—a violation of liquor dynamics. Changes in the production of cerebrospinal fluid and its resorption as a result of TBI are associated with damage to the endothelium of the choroid plexuses of the ventricles, secondary disorders of the microvasculature of the brain, fibrosis of the meninges, and in some cases, liquorrhea. These disorders lead to the development of liquor hypertension, and less commonly, hypotension.
In TBI, hypoxic and dysmetabolic disorders play a significant role in the pathogenesis of morphological disorders, along with direct damage to nerve elements. TBI, especially severe, causes respiratory and circulatory disorders, which aggravates existing cerebral dyscirculatory disorders and collectively leads to more pronounced brain hypoxia.
Currently (L. B. Likhterman, 1990) there are three basic periods during traumatic brain disease: acute, intermediate, and remote.
The acute period is determined by the interaction of the traumatic substrate, damage reactions and defense reactions, and is the period of time from the moment of the damaging effects of mechanical energy until the stabilization at one or another level of impaired cerebral and general body functions or the death of the victim. Its duration ranges from 2 to 10 weeks, depending on the clinical form of TBI.
The intermediate period is characterized by the resorption and organization of areas of damage, and the development of compensatory and adaptive processes until complete or partial restoration or stable compensation of impaired functions. The length of the intermediate period for non-severe TBI is up to 6 months, for severe TBI – up to a year.
The long-term period is the completion or coexistence of degenerative and reparative processes. The length of the period for clinical recovery is up to 2–3 years, for a progressive course it is not limited.
Brain concussion
Symptoms
Depression of consciousness (to the level of stupor) during a concussion can last from several seconds to several minutes, but may be absent altogether. Retrograde, congrade and antegrade amnesia develops for a short period of time. Immediately after a traumatic brain injury, a single vomiting occurs, breathing becomes more frequent, but soon returns to normal. Blood pressure also returns to normal, except in cases where the medical history is aggravated by hypertension. Body temperature during a concussion remains normal.
When the victim regains consciousness, there are complaints of dizziness, headache, general weakness, cold sweat, flushing of the face, and tinnitus. The neurological status at this stage is characterized by mild asymmetry of skin and tendon reflexes, small horizontal nystagmus in the extreme abductions of the eyes, and mild meningeal symptoms that disappear during the first week. With a concussion as a result of a traumatic brain injury, after 1.5 - 2 weeks, an improvement in the patient’s general condition is noted. It is possible that some asthenic phenomena may persist.
Diagnosis
Recognizing a concussion is not an easy task for a neurologist or traumatologist, since the main criteria for diagnosing it are the components of subjective symptoms in the absence of any objective data. It is necessary to familiarize yourself with the circumstances of the injury, using the information available to witnesses to the incident. Of great importance is an examination by an otoneurologist, with the help of which the presence of symptoms of irritation of the vestibular analyzer in the absence of signs of prolapse is determined.
Due to the mild semiotics of a concussion and the possibility of a similar picture arising as a result of one of many pre-traumatic pathologies, special importance in diagnosis is given to the dynamics of clinical symptoms. The justification for the diagnosis of “concussion” is the disappearance of such symptoms 3-6 days after receiving a traumatic brain injury. With a concussion, there are no fractures of the skull bones. The composition of the cerebrospinal fluid and its pressure remain normal. CT scan of the brain does not detect intracranial spaces.
Treatment
If a victim with a traumatic brain injury has come to his senses, first of all he needs to be given a comfortable horizontal position, his head should be slightly raised. A victim with a traumatic brain injury who is in an unconscious state must be given the so-called. The “saving” position is to lay him on his right side, his face should be turned to the ground, his left arm and leg should be bent at a right angle at the elbow and knee joints (if fractures of the spine and limbs are excluded). This position promotes the free passage of air into the lungs, preventing the tongue from retracting and vomit, saliva and blood from entering the respiratory tract. Apply an aseptic bandage to bleeding wounds on the head, if any.
All victims with traumatic brain injury are necessarily transported to a hospital, where, after confirmation of the diagnosis, they are placed on bed rest for a period that depends on the clinical characteristics of the course of the disease. The absence of signs of focal brain lesions on CT and MRI of the brain, as well as the patient’s condition, which allows one to refrain from active drug treatment, allows us to resolve the issue in favor of discharging the patient for outpatient treatment.
For concussions, do not use overly active drug treatment. Its main goals are to normalize the functional state of the brain, relieve headaches, and normalize sleep. For this purpose, analgesics and sedatives (usually in tablet forms) are used.
First aid for traumatic brain and spinal injuries
Traumatic brain injuries and traumatic injuries of the spinal column not only occupy one of the leading positions among the consequences of road traffic accidents, accidents, falls from heights, extreme sports, criminal cases and domestic incidents, but are also considered the most severe and dangerous to health .
All injuries are usually divided into open, in which the integrity of the skin is damaged, and closed, without visible damage to the soft tissues.
Traumatic brain injuries
The human brain is protected by fairly strong skull bones, but at the same time they can cause severe damage. Traumatic brain injuries include mechanical damage to the head, bone structures and soft tissues (skin, blood vessels, nerve endings, meninges or medulla).
When you hit your head, even without open injuries, the brain also gets bruised by hitting the skull, which doctors call a concussion. As a rule, it is accompanied by dizziness, headache, pallor of the scalp, vomiting, sometimes loss of consciousness, cold sweat, and temporary memory loss. Open head injuries are combined with damage to the integrity of the skin, skull fractures, and bleeding and/or cerebrospinal fluid from the nose and ears. Sunken orbital sockets and subcutaneous hemorrhages in the periorbital area may develop.
In addition, it should be remembered that all of the above symptoms may not appear immediately after the incident, but several hours or even days later. Therefore, even with a minor head injury, it is advisable to contact a traumatologist and conduct the necessary examinations to rule out a concussion or bruises.
Vertebral and spinal injuries
This category includes injuries to the back: soft tissues, muscle structures, the spinal column, tendons, ligaments, blood vessels and nerve fibers intertwining the spine, the spinal cord itself. It should be remembered that a fracture of the cervical or upper thoracic vertebrae can lead to immediate death.
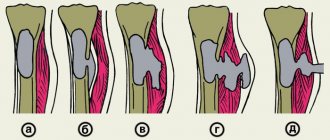
Closed injuries, concussions or compression of the spinal cord can be caused by compression of the brain by dislocations, subluxations or fractures of the vertebral bodies, displaced intervertebral discs, hernias, hematomas, inflamed tissues, etc. Accompanied by complete or partial dysfunction of internal organs, loss of sensitivity, impaired reflex reactions, paresis or paralysis of parts of the body located below the site of injury. Severe injuries are fraught with abscesses, hemorrhages of the spinal cord, necrosis of nerve cells and brain matter.
Open injuries of the spinal column with damage or rupture of the spinal cord are accompanied by spinal shock, loss of motor and sensory capabilities, autonomic functions, disturbances or cessation of the functioning of internal organs. In addition, there may be a significant decrease in temperature, blood pressure, and circulatory disorders. Recovery lasts from several weeks to several years.
First aid for head injuries
- They check whether the victim has a pulse, is breathing, and is conscious.
- An ambulance is called.
- If the victim is conscious and does not experience nausea, he must be laid on his back with a fairly hard cushion under his head (no more than 15° from the horizontal surface).
- The victim should not be given anything to drink, much less eat. This may cause severe vomiting.
- If the victim feels sick and vomits, he is laid on his side and a small cushion is also placed under his head.
- If there are no visible serious damage to the skin and skull, then cold is applied to the site of the injury. This will help relieve the pain a little and reduce the hematoma.
- For a bleeding head wound, apply a sterile bandage. The victim is not allowed to sit up and move independently and is transported to the hospital in a supine position.
First aid for back injuries
Signs of spinal injury:
- sharp pain in the neck or back;
- weakness in the lower or upper extremities;
- lack of motor abilities (paralysis of the body below the affected area);
- loss of sensitivity of the skin below the affected area;
- dysfunction of internal organs (for example, urinary or fecal incontinence).
Actions:
- They check whether the victim has a pulse, is breathing, and is conscious. Under no circumstances should you attempt to shift, turn over, or lift a person on your own. This can dislodge damaged vertebrae and cause even more harm to the body.
- The position of the victim is fixed, not allowing him to move, much less stand up. They try to stop visible bleeding, then wrap them up to prevent hypothermia, constantly monitoring breathing and pulse.
- If the victim is conscious and feels well, you can try to place him on a hard, flat surface with additional support for the head and entire body. This will require the help of several people who will synchronously perform the movement, holding the victim by the head, shoulders, pelvis and legs.
- Some cases require placing the victim on his stomach, but this action is performed only by the ambulance team.
- It is not recommended to give the victim anything to drink or eat until a full examination of the body has been carried out.
Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Brain contusion
Symptoms
A mild brain contusion is characterized by loss of consciousness after injury of up to several tens of minutes. After regaining consciousness, complaints of headache, dizziness, and nausea appear. Retrograde, congrade, and anterograde amnesia are noted. Vomiting is possible, sometimes with repetitions. Vital functions are usually preserved. Moderate tachycardia or bradycardia and sometimes increased blood pressure are observed. Body temperature and respiration without significant deviations. Mild neurological symptoms regress after 2-3 weeks.
Loss of consciousness with a moderate brain contusion can last from 10-30 minutes to 5-7 hours. Retrograde, congrade and anterograde amnesia are strongly expressed. Repeated vomiting and severe headache are possible. Some vital functions are impaired. Bradycardia or tachycardia, increased blood pressure, tachypnea without respiratory distress, and increased body temperature to subfebrile are detected. The manifestation of meningeal signs, as well as stem symptoms, is possible: bilateral pyramidal signs, nystagmus, dissociation of meningeal symptoms along the body axis. Pronounced focal signs: oculomotor and pupillary disorders, paresis of the limbs, speech and sensitivity disorders. They regress after 4-5 weeks.
Severe brain contusion is accompanied by loss of consciousness from several hours to 1-2 weeks. It is often combined with fractures of the bones of the base and vault of the skull, and profuse subarachnoid hemorrhage. Disorders of vital functions are noted: respiratory rhythm disturbances, sharply increased (sometimes decreased) blood pressure, tachy- or bradyarrhythmia. Possible blockage of the airways, intense hyperthermia.
Focal symptoms of hemispheric damage are often masked behind stem symptoms that come to the fore (nystagmus, gaze paresis, dysphagia, ptosis, mydriasis, decerebrate rigidity, changes in tendon reflexes, the appearance of pathological foot reflexes). Symptoms of oral automatism, paresis, focal or generalized seizures can be detected. Restoring lost functions is difficult. In most cases, gross residual motor and mental disorders remain.
Diagnosis
The method of choice for diagnosing a brain contusion is a CT scan of the brain. A CT scan reveals a limited area of low density, possible fractures of the calvarial bones and subarachnoid hemorrhage. With a brain contusion of moderate severity, CT or spiral CT in most cases reveals focal changes (non-compactly located areas of low density with small areas of increased density).
In case of severe contusion, CT scan reveals areas of heterogeneous increase in density (alternating areas of increased and decreased density). Perifocal cerebral edema is severe. A hypodense track is formed in the area of the nearest section of the lateral ventricle. Through it, fluid with breakdown products of blood and brain tissue is discharged.
There are five gradations of the condition of patients with TBI
Satisfactory condition. Criteria:
- clear consciousness;
- absence of violations of vital functions;
- absence of secondary (dislocation) neurological symptoms; absence or mild severity of primary focal symptoms.
There is no threat to life (with adequate treatment); the prognosis for recovery is usually good.
Moderate condition. Criteria:
- state of consciousness - clear or moderate stupor;
- vital functions are not impaired (only bradycardia is possible);
- focal symptoms - one or another hemispheric and craniobasal symptoms may be expressed, often appearing selectively.
The threat to life (with adequate treatment) is insignificant. The prognosis for restoration of working capacity is often favorable.
Serious condition. Criteria:
- state of consciousness - deep stupor or stupor;
- vital functions are impaired, mostly moderately according to 1–2 indicators;
- focal symptoms:
- stem - moderately expressed (anisocoria, decreased pupillary reactions, limited upward gaze, homolateral pyramidal insufficiency, dissociation of meningeal symptoms along the body axis, etc.);
- hemispheric and craniobasal - clearly expressed both in the form of symptoms of irritation (epileptic seizures) and loss (motor disorders can reach the degree of plegia).
The threat to life is significant and largely depends on the duration of the serious condition. The prognosis for restoration of working capacity is sometimes unfavorable.
Extremely serious condition. Criteria:
- state of consciousness - coma;
- vital functions - gross violations in several parameters;
- focal symptoms: stem - expressed roughly (plegia of upward gaze, severe anisocoria, divergence of the eyes along the vertical or horizontal axis, a sharp weakening of the pupils' reactions to light, bilateral pathological signs, hormetonia, etc.); hemispheric and craniobasal - pronounced.
The threat to life is maximum and largely depends on the duration of the extremely serious condition. The prognosis for restoration of working capacity is often unfavorable.
Terminal state. Criteria:
- state of consciousness - terminal coma;
- vital functions - critical impairment;
- focal symptoms:
- stem - bilateral fixed mydriasis, absence of pupillary and corneal reflexes;
- hemispheric and craniobasal - blocked by general cerebral and brainstem disorders.
Survival is usually impossible.
Diffuse axonal brain injury
Symptoms
Diffuse axonal brain damage is typically characterized by a prolonged coma after a traumatic brain injury, as well as pronounced brain stem symptoms. Coma is accompanied by symmetrical or asymmetrical decerebration or decortication, both spontaneous and easily provoked by irritations (for example, painful ones). Changes in muscle tone are very variable (hormetonia or diffuse hypotension). A typical manifestation is pyramidal-extrapyramidal paresis of the limbs, including asymmetric tetraparesis.
In addition to gross disturbances in the rhythm and frequency of breathing, autonomic disorders also appear: increased body temperature and blood pressure, hyperhidrosis, etc. A characteristic feature of the clinical course of diffuse axonal brain damage is the transformation of the patient’s condition from a prolonged coma to a transient vegetative state. The onset of this state is indicated by spontaneous opening of the eyes (with no signs of tracking or fixation of gaze).
Diagnosis
The CT picture of diffuse axonal brain damage is characterized by an increase in brain volume, as a result of which the lateral and third ventricles, subarachnoid convexital spaces, and also the cisterns of the base of the brain are under compression. The presence of small focal hemorrhages in the white matter of the cerebral hemispheres, corpus callosum, subcortical and brain stem structures is often detected.
Brain compression
Symptoms
Brain compression develops in more than 55% of cases of traumatic brain injury. The most common cause of brain compression is an intracranial hematoma (intracerebral, epi- or subdural). Rapidly increasing focal, brainstem and cerebral symptoms pose a danger to the life of the victim. Availability and duration of the so-called the “light gap” - expanded or erased - depends on the severity of the victim’s condition.
Diagnosis
A CT scan reveals a biconvex, less often a flat-convex, limited zone of increased density, which is adjacent to the cranial vault and is localized within one or two lobes. However, if there are several sources of bleeding, the area of increased density can be significant in size and have a crescent shape.
Diagnostics
When a patient with a traumatic brain injury is admitted to the intensive care unit, the following measures must be taken:
- Examination of the victim’s body, during which abrasions, bruises, joint deformities, changes in the shape of the abdomen and chest, bleeding and/or liquor leakage from the ears and nose, bleeding from the rectum and/or urethra, and a specific odor from the mouth are detected or excluded.
- Comprehensive x-ray examination: skull in 2 projections, cervical, thoracic and lumbar spine, chest, pelvic bones, upper and lower extremities.
- Ultrasound of the chest, ultrasound of the abdominal cavity and retroperitoneal space.
- Laboratory tests: general clinical analysis of blood and urine, biochemical blood test (creatinine, urea, bilirubin, etc.), blood sugar, electrolytes. These laboratory tests must be carried out in the future, daily.
- ECG (three standard and six chest leads).
- Testing urine and blood for alcohol content. If necessary, consult a toxicologist.
- Consultations with a neurosurgeon, surgeon, traumatologist.
A mandatory method of examining victims with traumatic brain injury is computed tomography. Relative contraindications to its implementation may include hemorrhagic or traumatic shock, as well as unstable hemodynamics. Using CT, the pathological focus and its location, the number and volume of hyper- and hypodense zones, the position and degree of displacement of the midline structures of the brain, the condition and degree of damage to the brain and skull are determined.
If meningitis is suspected, a lumbar puncture and dynamic examination of the cerebrospinal fluid are indicated, which allows monitoring changes in the inflammatory nature of its composition.
A neurological examination of a patient with a traumatic brain injury should be performed every 4 hours. To determine the degree of consciousness impairment, the Glasgow Coma Scale is used (state of speech, response to pain and ability to open/close eyes). In addition, the level of focal, oculomotor, pupillary and bulbar disorders is determined.
Treatment of traumatic brain injury
Conservative therapy
For a victim with impaired consciousness of 8 points or less on the Glasgow scale, tracheal intubation is indicated, due to which normal oxygenation is maintained. Depression of consciousness to the level of stupor or coma is an indication for auxiliary or controlled mechanical ventilation (at least 50% oxygen). With its help, optimal cerebral oxygenation is maintained.
Patients with severe traumatic brain injury (hematomas, cerebral edema, etc. detected on CT) require monitoring of intracranial pressure, which must be maintained below 20 mmHg. For this purpose, mannitol, hyperventilation, and sometimes barbiturates are prescribed.
To prevent septic complications, escalation or de-escalation antibacterial therapy is used. For the treatment of post-traumatic meningitis, modern antimicrobial drugs approved for endolumbar administration (vancomycin) are used.
Patients begin feeding no later than 3 days after TBI. Its volume is increased gradually and at the end of the first week following the date of the traumatic brain injury, it should provide 100% of the patient’s caloric needs. The route of nutrition can be enteral or parenteral. To relieve epileptic seizures, anticonvulsants are prescribed with minimal dose titration (levetiracetam, valproate).
Surgery
The indication for surgery is an epidural hematoma with a volume of over 30 cm³. It has been proven that the method that provides the most complete evacuation of the hematoma is transcranial removal. Acute subdural hematoma with a thickness of more than 10 mm is also subject to surgical treatment. In comatose patients, acute subdural hematoma is removed by craniotomy, retaining or removing a bone flap. An epidural hematoma with a volume of more than 25 cm³ is also subject to mandatory surgical treatment.
Treatment of TBI and consequences of brain injuries
In the acute period, decongestant, neurometabolic, neuroprotective, symptomatic therapy is carried out, which consists of selecting several medications offered both in the form of tablets and in the form of injections (drip and intramuscular).
This treatment is carried out for about a month. After which the patient remains under the supervision of his attending physician, depending on the severity of the TBI, from six months to several years.
For at least three months after a TBI, drinking alcoholic beverages and strenuous physical activity is strictly prohibited.
In addition to traditional methods of treating TBI, there are no less effective methods:
- acupuncture,
- osteopathy.
In combination with drug therapy and physiotherapy, these techniques can have a more pronounced and faster effect. However, in some cases they are contraindicated for use.
Everyone knows the fact that treatment must be comprehensive, and the more techniques are used during treatment, the better.
After completing the course of treatment, the patient must be under the supervision of a doctor, and subsequently he may need repeated courses, usually once every six months.
Forecast
Concussion is a predominantly reversible clinical form of traumatic brain injury. Therefore, in more than 90% of cases of concussion, the outcome of the disease is the recovery of the victim with full restoration of ability to work. Some patients, after the acute period of concussion, experience certain manifestations of post-concussion syndrome: disturbances in cognitive functions, mood, physical well-being and behavior. 5-12 months after a traumatic brain injury, these symptoms disappear or are significantly smoothed out.
Prognostic assessment in severe traumatic brain injury is carried out using the Glasgow Outcome Scale. A decrease in the total number of points on the Glasgow scale increases the likelihood of an unfavorable outcome of the disease. Analyzing the prognostic significance of the age factor, we can conclude that it has a significant impact on both disability and mortality. The combination of hypoxia and arterial hypertension is an unfavorable prognosis factor.