From this article you will learn:
- causes of rosacea on the face,
- what role does the solarium play here?
- symptoms, effective medications,
- reviews of rosacea treatment with laser and IPL.
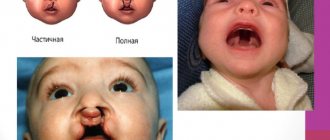
Rosacea is a chronic skin disease that manifests itself in the form of erythema (redness) of the skin, telangiectasia, as well as papules and pustules resembling regular acne. Due to the latter, this disease is also called “acne rosacea”. Rosacea occurs mainly in the middle third of the face, as well as in the forehead, nose and chin. In rare cases, it can occur outside the face - mainly on the neck, chest, scalp or ears.
Typical locations of Rosacea are:
A predisposing factor to the appearance of rosacea is considered, for example, to be exposure to solar UV radiation, which stimulates the production of vascular endothelial growth factor and leads to the appearance of networks of small capillaries, i.e. telangiectasia. Accordingly, rosacea can easily appear after tanning. Another factor is genetic predisposition (associated with the lability of the walls of blood vessels), as well as a person’s individual tendency to redness of the skin, which is also associated with the superficial location of the vessels.
In addition to these factors, the influence may be exerted by: 1) parasitic skin disease caused by Demodex folliculorum mites, as well as the bacteria Staphylococcus epidermidis, 2) gastrointestinal diseases associated with infection of the intestines by the bacterium Helicobacter pylori. Studies have found that in the presence of intestinal inflammation and Helicobacter pylori, hypersensitization of sensory neurons in the facial area occurs (through the synthesis of bradykinin, which is a powerful vascular dilator).
Most often, the disease is detected in patients 30-50 years old, and according to statistics it occurs in 10% of the population. It has been noted that rosacea occurs more often in people with fair skin who blush easily. Most often these are women with fair skin, blond hair and blue eyes. In men, the disease develops less frequently, but phymatous changes develop more often. Depending on the clinical manifestations, rosacea is usually divided into 4 types, which we will discuss below.
Rosacea on the face: photos, symptoms
Symptoms of rosacea usually begin with erythema, a persistent, temporary redness on the cheeks, nose, forehead or chin. Or another option - redness can be observed in the form of frequent, rapidly passing outbreaks of facial redness, which are usually called the term “hyperemia”. In both cases, the resulting redness may be accompanied by a feeling of warmth or burning. Over time, periods of skin redness become longer and more intense.
Rosacea on the face: photos, symptoms
In parallel with this, visible small blood vessels appear on the skin of the face, which are commonly called telangiectasia or spider veins. In the absence of treatment, inflammatory elements begin to appear - papules or pustules (they look like ordinary purulent pimples). In severe cases, the skin may gradually begin to thicken, in which case it also becomes loose. This can lead to facial disfigurement. If this process occurs on the nose, then it is called “rhinophyma”.
Rosacea affects the eyes in about 50% of patients, causing them to appear irritated, puffy, or bloodshot. If not treated promptly, such inflammation can lead to damage to the cornea and loss of visual acuity. All of the above symptoms are the main ones.
Secondary signs – researchers also identify secondary signs of rosacea, which, however, do not appear in isolation, but in combination with one or more main signs. This may be a feeling of burning or itching of the skin on the face. Or it may be red spots (in the form of plaques) that rise slightly above the surface of the skin. Or the skin in the middle third of the face may look dry, rough, and flaky.
Next, we move on to treatment regimens for various forms of rosacea. And here it must be remembered that when rosacea occurs on the face, the causes and treatment will always be closely interrelated, and therefore it is especially important at the first stage to identify the causative factor, as well as triggers leading to an exacerbation of the disease.
Erythematotelangiectatic subtype
Subtype I rosacea is characterized by damage to the facial skin in the form of erythema, which is localized on the cheeks and sides of the nose. At first it is transitional in nature, and then becomes stable. Its color can vary from bright pink to bluish-red, the shade depending on the duration of the disease.
Patients often develop spider veins (telangiectasia), and the face becomes slightly swollen. There may be a burning sensation, tingling sensation in the erythema area.
The manifestation of rosacea intensifies with a decrease or increase in air temperature, consumption of spicy foods, alcoholic beverages, and emotional stress.
The skin is sensitive to UV irradiation and topical medications. Even neutral cosmetics and products with UV filters can cause increased inflammation.16
Erythematous-telangiectatic form -
Clinical features - this type is characterized by either the appearance of persistent erythema (i.e. redness) in the middle third of the face, or frequent but quickly passing attacks of hyperemia. Hyperemia differs from erythema primarily in its duration - it tends to pass quickly, while the severity of redness during hyperemia can be from moderate to very intense. In addition, patients often complain of small blood vessels visible through the skin (telangiectasia), as well as swelling of the face, roughness of the skin or peeling, and a feeling of tightness.
Telangiectasia with rosacea: photo
In this form, most patients associate a sharp deterioration in their condition with exposure to irritating factors - drinking hot drinks, spicy food, exposure to the sun, heat, etc. As a rule, these patients have sensitive skin and therefore, in response to the application of various products to the surface of the skin, they develop There is often a burning and tingling sensation in the skin. Many patients with this type of rosacea do not believe that they are sick with anything and do not seek qualified help (24stoma.ru).
Treatment regimens for erythematotelangiectatic form –
| Expressiveness | Treatment |
| Mild course - characterized by weak persistent erythema or not too frequent mild short-term outbreaks of hyperemia. There are rare telangiectasias. |
|
| Moderate course - moderate persistent erythema or frequent unpleasant outbreaks of hyperemia are observed. There are several well-defined telangiectasias. | In addition to the above:
|
| Severe course - pronounced persistent erythema or frequent severe hyperemia is observed. There may be tissue swelling in the area of redness. There are many well-defined telangiectasias. Patients may complain of burning, tingling, skin peeling, or plaque formation. | In addition to the above:
|
* The effectiveness of drugs with brimonidine was confirmed in clinical studies “Fowler J, Jackson M, Moore A, published in the journal Drugs Dermatol 2013; 12: 650-656."
Rosacea on the face: treatment of the erythematotelangiectatic form (before and after photos)
Mechanisms of rosacea development
There are several pathogenetic theories for the occurrence of rosacea227:
- Disorders of the innate immune response. This function provides protection to the body from microbial infections. When the innate immune system is activated, antimicrobial molecules and cytokines are secreted. In rosacea, the production of catelacid (one of the antimicrobial molecules) is increased.
- Vascular changes. With rosacea, there is increased blood flow to the affected areas, which is why patients often turn red, especially when exposed to heat. The expression of lymphatic endothelial markers is also increased.
- Exposure to ultraviolet radiation. UV stimulates angiogenesis - the formation of new blood vessels. Ultraviolet radiation also damages the intercellular substance of the dermis and blood vessels, increasing the production of chemically active oxygen particles.
- Violation of the epidermal barrier. Transepidermal water loss occurs and the skin irritability threshold decreases.
- Bacteria. In rosacea, there is an increased colonization of Demodex mites. Staphylococcal microflora also plays a role in the development of the disease.
- Neurogenic inflammation. Sensory nerves in areas of inflammation produce neurotransmitters, which leads to vasodilation and release of plasma proteins into the subcutaneous tissue.
For treatment to be effective, it is necessary to reduce the severity of symptoms, prolong remission and prevent exacerbations of the disease. However, each type of rosacea has its own symptoms.
Papulopustular form -
The papulopustular form of rosacea manifests itself as persistent erythema in the middle third of the face, against which there are single or multiple papules or pustules (they look like pimples). Some patients may have plaques that rise above the surface of the skin. When treating this form at the first stage, the most important thing is to remove the inflammatory component, and only after that proceed to the correction of erythema or telangiectasia.
Treatment regimens for papulopustular form –
| Expressiveness | Treatment |
| Mild course - there are several papules or pustules without plaques; moderate persistent erythema is observed. |
|
| Moderate course - from several to numerous papules or pustules (but without plaques); moderate persistent erythema is observed. | |
| Severe – numerous papules or pustules with or without plaques; there is severe persistent erythema; Possible burning and tingling. | In addition to the above:
|
* The effectiveness of drugs with Ivermectin was confirmed in clinical studies “Stein Gold L, Kircik L, Fowler J, published in the journal Drugs Dermatol 2014; 13: 316-323."
Rosacea: treatment of papulopustular form (before and after photos)
Acne and rosacea: how to treat?
The approaches to treating acne and rosacea are different, although they can sometimes overlap. For example, in both cases, azelaic acid preparations can be prescribed.
Azelik gel contains 15% azelaic acid. It can be prescribed for the treatment of mild to moderate acne, as well as rosacea. It should be applied 2 times a day to cleansed skin.5
Along with drug treatment for rosacea, it is important to exclude exposure to triggering factors. For example, before going outside, it is imperative to apply a product with a high level of SPF, if possible, avoid being in severe frost or leaving the house in windy weather. Patients need to reconsider their diet, excluding too spicy, hot foods, and carbonated drinks. You should stop using abrasive cosmetics. Stress and strong emotional overexcitation can trigger the appearance of erythema.16
Treatments for acne and rosacea overlap not only in terms of prescribing medications. Laser therapy can be prescribed for both diseases9,16.
Phymatous form (rhinophyma) –
Phymatous changes are called thickening of the skin (mainly in the nose area) - with the appearance of roughness, irregularities, and nodules on it. The thickening can be pronounced and then it leads to partial disfigurement of the face. Occurs more often in men, because they are less likely to seek medical help in the early stages of the disease. Thickening of the skin of the nose is called rhinophyma. Rarely, the phymatous form can be observed on the chin, forehead, cheeks, ears and eyelids.
Also, with this form, telangiectasia and hyperplasia of the sebaceous glands can occur. In the dermal layer of the skin, a dense inflammatory infiltrate is observed, in place of which then, for example, tissue proliferation and fibrosis occurs with the formation of nodes. There are several histological types of rhinophyma, for example, fibrous, glandular, fibroangiomatous, etc.
Treatment regimens for the phymatous form –
| Expressiveness | Treatment |
| Mild course - an increase in skin thickness, but without changes in contours |
|
| Moderate flow - there is a change in contours, but without a nodal component | In addition to the above:
|
| Severe flow - there is a change in contours with a nodal component |
Rhinophyma: removal of excess tissue with a CO2 laser
Ophthalmic rosacea –
In this form of rosacea, patients' eyes have a puffy or bloodshot appearance. Patients complain of a sensation of a foreign body in the eye, burning, tingling, dryness, itching, photosensitivity, blurred vision, telangiectasia of the eyelid margins, erythema around the eyes, blepharitis, recurrent conjunctivitis, iritis... With this form, a decrease in visual acuity may also occur, for example, due to corneal keratitis.
With ophthalmic rosacea, many patients mistakenly treat their eyes on their own, mistaking the onset of the disease for symptoms of an allergic reaction. As a result, patients most often end up seeing an ophthalmologist with moderate to severe forms of the disease.
Treatment regimens for ophthalmic rosacea –
| Expressiveness | Treatment |
| Mild course - redness of the conjunctiva of the eyelids and dysfunction of the meibomian glands. |
|
| Moderate course - redness of the conjunctiva of the eyelids, telangiectasia of the edges of the eyelids or conjunctiva of the eyeball, erythema around the eyes, impaired secretion of tear fluid, initial forms of corneal damage. | In addition to the above:
|
| Severe course - severe inflammation of the conjunctiva of the eyelids and eyeball, resistant to treatment; episcleritis, iritis or keratitis in addition to corneal damage and visual impairment. | In addition to the above:
|
Diagnostics
Rosacea is diagnosed based on a collected medical history and visual examination of clinical manifestations. Dr. Zhurbina notes that the difficulty of diagnosis lies in the fact that there are no specific diagnostic tests. The age of onset of the disease and the absence of comedones (nodules formed as a result of blockage of the ducts of the sebaceous glands and looking like black or white dots) allow you to distinguish rosacea from acne.
In addition, the disease is distinguished by the presence of hyperemia - pronounced blood flow to the tissues, the patient's complaints of burning and hot flashes, as well as constant peeling and dry skin. Another distinctive feature of the problem is the fact that rosacea “attacks” the face, avoiding the rest of the body.
When diagnosing and choosing treatment tactics, it is important to differentiate rosacea from acne vulgaris, systemic lupus erythematosus, sarcoidosis, photodermatitis, drug-induced and perioral dermatitis, and skin granulomas.
If an illness is detected, it is advisable for the patient to undergo a series of additional examinations in order to identify the possible presence of concomitant diseases that could become a trigger for the development of rosacea, and to begin complex therapy as soon as possible. The following studies are recommended:
— analysis of hormone levels in the blood;
— FGDS or radiography of the stomach;
- tests for the state of the immune system as a whole.
pixabay.com/Kjerstin_Michaela
Factors that trigger rosacea outbreaks –
The following list of triggers that can lead to rosacea flare-ups was compiled based on clinical research and published by the National Rosacea Society (USA).
| Factors that can cause rosacea flare-ups | ||
| Products - liver, yogurt, sour cream, cheese (except cottage cheese), chocolate, vanilla, soy sauce, yeast (bread is fine), vinegar, eggplant, avocado, spinach, beans and peas, citrus fruits, tomatoes, bananas, red plums, raisins or figs, spicy and too hot foods. Emotional states – stress, anxiety. | Medicines – some analgesics, vasodilators, steroids. Skin care products – cosmetics and hair sprays containing alcohol, witch hazel, fragrance, menthol, peppermint, eucalyptus oil, or any substance that causes redness or burning. Beverages - any alcohol (especially red wine), hot drinks, hot chocolate, coffee or tea. | Weather – exposure to the sun, strong wind, cold, high humidity. Temperature – sauna, hot baths, simple overheating, excessively warm environment. Medical conditions – menopause, cough, caffeine withdrawal syndrome. Exercise stress - active sports, work with a load, work in an incline. |
Importance of various factors –
Below we will divide these factors by strength (from the strongest to the weakest). Next to each factor, you will see the percentage of people for whom this factor was significant and almost certainly led to the development of a rosacea outbreak. This list is based on a survey of more than a thousand patients, and is also published by the National Rosacea Society.
In what percentage of cases do factors lead to exacerbations -
- sun exposure – 81%,
- emotional stress – 79%,
- hot weather – 75%,
- wind – 57%,
- heavy exercise – 56%,
- alcohol consumption – 52%,
- hot baths – 51%,
- cold weather – 46%,
- spicy food – 45%,
- humidity – 44%,
- high body temperature – 41%,
- some skin care products – 41%,
- hot drinks – 36%,
- certain cosmetics – 27%,
- medicines – 15%,
- medical conditions (see above) – 15%,
- some fruits – 13%,
- marinated meat – 10%,
- some vegetables – 9%,
- dairy products – 8%,
- other factors – 24%.
Skin care and cosmetics –
Gentle skin care and effective use of cosmetics can improve the appearance of your skin, but you should use products that are suitable for sensitive skin. Avoid any products that cause burning, redness or irritation. It is worth abandoning chemical and mechanical peeling products. In addition to irritants, components that provoke outbreaks of rosacea include:
- alcohol,
- witch hazel,
- flavorings,
- menthol,
- peppermint,
- Eucalyptus oil.
Try to use products that do not contain fragrances or strong preservatives. Always read the ingredient list carefully. Do not use many different products at once. Before using the product on your face, test it on your neck. In addition, please note that patients with rosacea, especially in winter (as well as in dry air indoors or outdoors), need to regularly use skin moisturizing creams. This will reduce skin irritation and reduce the risk of flare-ups.
Men's shaving and aftershave products – Shaving can be a big challenge for men with rosacea, so one option is to use an electric razor. You should also avoid using any shaving or aftershave lotions or products that contain alcohol, menthol or other irritants. Use gentle aftershave balms to soothe and hydrate your skin.
Sun protection –
Exposure to active solar radiation is the main factor causing flare-ups of rosacea and the appearance of telangiectasia. There are 2 types of damaging sun rays – UVA radiation and UVB radiation. Solar radiation consists of approximately 96.5% radiation of the first type, and 3.5% of the second type. UVA rays penetrate deeper into the skin, they lead to skin aging, the development of melanomas and affect the skin throughout the day.
Despite the fact that UVB rays are small (only 3.5%) they contribute to the development of skin cancer. Patients with rosacea need to choose sun protection products that protect against two types of radiation at once, with an SPF of 15 or higher. Sunscreens with mineral rather than chemical components will have minimal irritating effects on the skin. These components include zinc oxide and titanium dioxide. Apply these products every day when you go outside.
If you plan to stay in intense sun, apply the cream every 2 hours, and also every time immediately after swimming or heavy sweating. But even following these recommendations, you should limit your exposure to the sun in the summer, and try not to stay in the sun for long periods between 10 a.m. and 4 p.m. Our article: Facial Rosacea Causes and Treatment is based on clinical studies published by the National Rosacea Society (USA), and we hope you found it useful!
Sources:
1. Textbook of dermatology “Fitzpatrick's Dermatology” (8th edition), 2. American Academy of Dermatology (USA), 3. National Rosacea Society (National Rosacea Society, USA), 4. “Comparative assessment of the effectiveness of various methods of treating rosacea” (Pearl).
Modern methods of treating rosacea
Numerous methods of treating rosacea are determined by the variety of etiological and pathogenetic factors, stage, and variety of clinical forms of the disease. Therapy for patients with rosacea is a difficult task, since the use of any of the currently proposed treatment methods in the form of monotherapy does not lead to complete recovery, but only has a temporary effect. The presence of many aspects of the etiology and pathogenesis of rosacea that are still unclear, and the lack of reliable treatment methods make the problem of developing new approaches to the treatment of this pathology extremely relevant for modern dermatology.
The therapeutic effect of some drugs is aimed at reducing inflammatory phenomena, while others are aimed at correcting various somatic disorders of the digestive tract, central nervous system, vascular reactions, etc. [1]. The main treatment involves the elimination of predisposing and provoking factors, diet, and photoprotection [2].
Classic general therapy for rosacea includes antibiotics, metronidazole and topical therapy. During periods of severe exacerbation, antihistamines are added. However, antibiotics are still the basic therapy for rosacea, while tetracyclines remain the most effective antibacterial drugs in the treatment of this dermatosis [3–6]. Treatment with tetracyclines is usually long-term - up to 12 weeks [3], which undoubtedly entails the formation of side effects, such as the development of candidiasis, pigmentation disorders of the skin and teeth. Currently, antibiotics from the macrolide group are used - erythromycin, clarithromycin, josamycin, etc. [3, 7, 8].
Despite the controversial issue about the etiological role of Demodex folliculorum in the pathogenesis of rosacea, oral administration of metronidazole is an integral part of rosacea therapy [9]. Oral treatment with metronidazole lasts 4–6 weeks, in some patients up to 8 weeks, which also provokes side effects: nausea, headaches, dry mouth, vomiting, urticaria, etc. An effective alternative is metronidazole in the form of a 1% gel applied externally [3, 4, 7, 10]. Although in domestic dermatology these drugs are widely prescribed for the treatment of rosacea, the Food and Drug Administration in the USA has not approved their use. It is believed that Demodex spp. survive even at high concentrations of metronidazole [11].
The development of resistance of bacterial-parasitic flora to drugs of the imidazole group and tetracycline antibiotics leads to the need to improve treatment methods and search for new drugs. Recently, synthetic retinoids have been used to treat severe forms of rosacea. The high therapeutic effectiveness of the drug is associated with its influence on the processes of differentiation and keratinization of epidermal cells and sebaceous glands. The average duration of treatment with isotretinoin is 4–6 months [12]. This drug has side effects, the main of which is teratogenicity. Local use of synthetic retinoids eliminates the development of their systemic side effects, but also causes dry skin, peeling, and itching [3–7, 11, 13]. Recent studies have indicated a 20% increase in the duration of remission in patients with rosacea taking isotretinoin compared with patients receiving combination treatment (metronidazole and doxycycline) [14].
Traditionally, local therapy for rosacea consists of cold lotions with antiseptic solutions (1–2% boric acid solution, 1–2% resorcinol solution, chamomile decoction, etc.), ointments, pastes or creams with an antidemodex effect [1, 3].
Modern topical medications are used mainly in the form of creams containing azelaic acid, metronidazole 0.75% and 1%, adapalene 0.1% and metronidazole gel 1% [1, 3, 4]. Some authors insist on the particular effectiveness of azalaic acid in the treatment of rosacea [10]. However, this statement is also disputed. According to A. Parodi et al. (2011) and B. A. Yentzer et al. (2010), monotherapy with azelaic acid without the use of oral antibiotics leads to chronicity of the process and the absence of a visible effect [8, 15]. The most optimal is the combined use of azelaic acid, doxycycline (or clindamycin) and metronidazole [8, 11, 16].
Recent reports indicate the effectiveness of 1% pimecrolimus cream in the treatment of papulopustular rosacea. Pimecrolimus, a derivative of the macrolactam ascomycin, selectively inhibits the production and release of cytokines and mediators from T lymphocytes and mast cells. It has been proven that the use of this cream allows one to obtain clinical remission in 82% of patients [17, 18].
As various studies by domestic and foreign scientists show, a significant increase in the effectiveness of therapy can be expected when using combination therapy methods that combine medications and physiotherapeutic methods of treatment.
Physiotherapeutic methods used in the treatment of rosacea are cryotherapy, electrophoresis, and destructive techniques.
Cryotherapy is carried out every other day or daily until deep exfoliation. The method is indicated for patients regardless of the stage of the disease. Cryotherapy has anti-inflammatory, vasoconstrictor, and antiparasitic effects [4, 7]. Clinical recommendations also include electrophoresis (10–30% ichthyol solution 2–3 times a week, with lidase 2–3 times a week, 10–15 sessions) [4].
In the treatment of papulopustular, cystic and nodular forms of rosacea, destructive techniques such as electrocoagulation and dermabrasion are indicated. These methods, unfortunately, have a number of disadvantages: postoperative infection, leukoderma, the formation of epidermal cysts and scars [3, 4, 7].
In recent years, combination treatment methods have been considered the most successful. For example, some researchers have successfully used a combination of isotretinoin and dermabrasion with good results [5]. Combining various external drugs, such as azalaic acid, metronidazole and clindamycin, is effective [11].
However, all these methods are gradually losing their relevance not only due to the existing side effects, but also due to their low efficiency compared to laser radiation [19].
One of the most significant scientific achievements of practical medicine of the twentieth century was the formation of an independent field - laser medicine. The first studies on the practical use of laser radiation were devoted to various areas of surgery, where laser devices were used as universal destructors and coagulants. The discovery of biochemiluminescence provided the prerequisites for the development of a new direction in laser medicine - the therapeutic effect of low- and high-energy laser radiation on cellular and intracellular processes. Scientific achievements have made it possible to substantiate not only symptomatic, but also pathogenetic use of laser in the treatment of skin diseases [2]. Before the advent of laser therapy, the ability to improve facial skin conditions in patients with rosacea was very limited. Thus, electrocoagulation and cryotherapy were mainly used to treat facial telangiectasia. However, these methods are characterized by the risk of developing various complications (hyperpigmentation, atrophy) and a high rate of relapses [10, 19, 20]. Therefore, today, according to most authors, laser therapy is the method that provides the most effective and long-lasting results in the treatment of rosacea [2–5, 7, 11, 19, 20].
Depending on the energy characteristics of the laser, low-energy lasers with a power density of less than 100 mW/cm2 and high-energy lasers with a power density of more than 10 W/cm2 are distinguished. The photobiological effects it causes directly depend on the laser power. Low-intensity laser radiation (LLR) is associated with photochemical reactions.
The photothermal effects of high-intensity laser irradiation (HILI) cause local tissue destruction in the form of photodynamic action, photocoagulation or photoablation [2].
The selective photothermal or photoacoustic effect of VLI is explained by the theory of selective photothermolysis (SPT), according to which, in order to damage or destroy the target chromophore, it is necessary that the absorption coefficient of the target and the surrounding tissue differ as much as possible, and the pulse duration is less than or equal to the thermal relaxation time [2].
The discovery of SFT justified the impact on specific skin chromophores without damaging surrounding structures by selecting the appropriate wavelength, pulse duration and energy density. In this way, laser parameters can be optimized to precisely target the target tissue with minimal collateral damage to other tissues. The chromophore targeted in the treatment of vascular formations is oxyhemoglobin [19]. The greatest absorption of radiation by oxyhemoglobin occurs at wavelengths of 18, 542, 577 nm. As a result of absorption of laser radiation by oxyhemoglobin, the vessel is exposed to energy and coagulates [19].
Various types of lasers have been used to treat vascular skin pathologies with varying degrees of effectiveness and safety. The first great achievement in laser therapy for vascular formations was the creation in 1970 of an argon laser with a wavelength of 488 and 514 nm. Unfortunately, the use of a laser device generating continuous radiation caused coagulative necrosis of the superficial layers of the skin, which often led to subsequent scar formation and depigmentation [19].
Modern authors for the treatment of facial telangiectasia suggest using mainly long-wavelength (577 and 585 nm) rays [3, 4, 7] and a pulsed dye laser (PDL) (585 nm) with a low energy density of 1.5 J/cm2 or 3. 0 J/cm2. One pass is performed per session, procedures are carried out once a week, for a course of 3–4 sessions [2, 5, 21]. Despite the fact that the wavelength of 595 nm penetrates tissue better than 585 nm, the degree of absorption of radiation by oxyhemoglobin decreases after 585 nm. Therefore, to increase the penetration depth of an ILC with a wavelength of 595–600 nm, an additional increase in the radiation flux density by 20–50% is required compared to an ILC with a wavelength of 585 nm [19]. Improving the cleansing of facial skin from telangiectasia and reducing the severity of erythema can be achieved by applying pulses with a lower luminous flux density, but with a longer duration, which also helps to avoid the appearance of purpura after treatment. According to Goldberg J. (2010), the degree of skin cleansing after one treatment session increased from 67% when using non-overlapping pulses to 87% after applying the pulse overlapping technique [19]. Complications after treatment of ILC, such as hyperpigmentation, atrophy, hypertrophic scar, eczematous dermatitis, are extremely rare [19]. Recent studies have proven the therapeutic effectiveness of VLI with a wavelength of 578 nm, which is 88% for the erythemato-telangiectatic form, 83.7% for the papular form, 76.3% for the pustular form, and 62.7% for the infiltrative-proliferative form. Long-term results of this study showed that after three years the achieved effect was maintained on average in 21% of patients [22].
However, according to Potekaev N.N. and Kruglova L.S. (2012), if telangiectasia predominates in the clinical picture, the method of laser non-contact coagulation using a diode or neodymium laser is indicated [2, 23]. According to the authors, generators of intense pulsed light (IPL) with a wavelength of 500–1200 nm and a maximum emission in the range of 530–700 nm are also effective in the treatment of rosacea. For superficial telangiectasia with a diameter of up to 0.3 cm, an effective effect was noted at a wavelength of 530–600 nm (yellow-green spectrum) [2, 21]. Having a wide range of wavelengths, radiation is able to reach target vessels located at different depths from the skin surface. Despite the fact that radiation with a long wavelength penetrates deeper, the level of energy absorption by oxyhemoglobin decreases. Therefore, to compensate for the decrease in energy absorption, an increase in the radiation flux density is required, which is what is used in this type of device. Thus, both superficial and deeply located vessels are effectively heated, and the size of the spot formed by the radiation is also quite large. Another likely advantage of IPL is that the laser energy is delivered to the target tissue using a longer pulse duration. This leads to more uniform heating and coagulation of the entire pathologically altered vessel [19, 21, 23].
Heavy metal vapor lasers have also been successfully used to treat telangiectasia, but in this case the laser energy is absorbed not only by oxyhemoglobin, but also by melanin contained in the epidermis and dermis. Therefore, metal vapor lasers are used to treat only patients with fair skin (Fitzpatrick types I and II). Patients with dark skin are at high risk of pigmentation disorders that appear following an inflammatory reaction, usually the formation of blisters and scabs [19, 23].
Other systems used to treat vascular lesions are the potassium titanyl phosphate (KTP) laser, long-pulse neodymium yttrium aluminum garnet (Nd:YAG) laser, long-pulse alexandrite lasers (755 nm), and diode lasers (800, 810, 930 nm). nm). The CTF laser is a frequency doubled Nd:YAG laser that produces radiation in the 532 nm range (green light). The wavelength of 532 nm is close to one of the peaks of radiation absorption by hemoglobin, and therefore is well suited for the treatment of superficial blood vessels [19, 21]. At a wavelength of 1064 nm, the Nd:YAG laser allows for much deeper penetration into the dermis. In this case, coagulation of blood vessels can be achieved at a depth of 2–3 mm from the dermoepidermal junction. This allows for a deeper vasculature to be targeted that ILC may not be able to reach. These deep large blood vessels typically require pulse durations between 3 and 15 ms. Since the absolute absorbance of hemoglobin at 1064 nm is lower than at 585 nm, significantly higher fluences must be used at this wavelength. As a result, cooling comes first for this laser [20, 23].
Long-pulse alexandrite lasers (755 nm) and diode lasers (800, 810, 930 nm) generate longer wavelengths that correspond to the region of minimum absorption by hemoglobin, making them theoretically more suitable for treating large, deep vessels with a diameter of 0.4 mm [19].
According to J. Goldberg (2010), vascular formations in the wings of the nose pose certain difficulties in laser therapy for rosacea. To remove telangiectasias in this area, multiple treatment sessions and, possibly, a repeat course of treatment in the future are necessary [19]. Facial erythema responds equally well to treatment using both ILC and IPL [10, 20].
Modern laser therapy is on the threshold of combinations of various laser methods in the treatment of dermatoses. It is possible to optimize the clinical outcome and reduce the risk of side effects with the combined use of fractional non-selective laser and IPL; carbon dioxide (CO2) laser and radio frequency (Radio Frequency, RF) technology, laser and photodynamic therapy (PDT) [24, 25].
Today, one of the most controversial issues is the use of laser PDT. First of all, this is due to the limited number of studies with a sufficient evidence base for the effectiveness of PDT in the treatment of malignant and benign skin tumors. The therapeutic effect of PDT is based on photochemical reactions that occur during the interaction of porphyrins, laser radiation and oxygen. In this case, the laser is an activator of photochemical processes in cells and does not cause photothermal damage. For PDT, any laser with a wavelength of 400–800 nm can be used [2]. However, this method is also not without drawbacks. Side effects manifest themselves in the form of phototoxic reactions in the form of erythema, edema, crusts, erosions, vesicles, which, as a rule, is observed in most patients and is transitory. Among the long-term consequences of therapy, the possible occurrence of hyperpigmentation at the site of PDT is noted [2].
In the infiltrative-productive stage of rosacea, destructive methods are indicated, since the existing ultrastructural changes in the microcirculatory system of the facial skin are irreversible. In this situation, laser ablation is prescribed to remove hypertrophied tissue, for example, with rhinophyma [5]. Ablation is carried out until the level of the sebaceous glands is reached. In this case, it is possible to use a pulsed CO2 laser or a fractional erbium (Er: YAG) laser with a modulated pulse mode [2]. The use of these types of lasers remains the “gold” standard for ablative procedures, being an alternative to the traditional surgical approach to this problem [5, 7]. However, when treated with a CO2 or Er: YAG laser, prolonged healing of the wound defect is observed and the risk of developing phenomena such as delayed reepithelialization, persistent erythema, skin hypopigmentation, and in some cases, the formation of hypertrophic and keloid scars increases [26].
For all forms of rosacea, courses of low-energy laser treatment are recommended, which are carried out every other day (6 procedures), the average exposure time is 25 minutes [2].
Thus, despite some limitations, lasers and light source devices remain the best choice in the treatment of vascular skin lesions [10, 20].
Despite the fact that currently there is an extensive arsenal of medications and methods of treating rosacea, the effectiveness of treatment is directly dependent on the duration of therapy and the severity of side effects. The constant search for an optimal approach to the treatment of this dermatosis has led to advances in the field of laser technologies, which have made it possible to take a huge step in this direction.
Literature
- Volkova E. N., Osipova N. K., Rodina Yu. A., Grigorieva A. A. Rosacea: new approaches to old problems // Russian Journal of Skin and Venereal Diseases. 2010, no. 2. pp. 33–39.
- Potekaev N. N., Kruglova L. S. Laser in dermatology and cosmetology. M.: Ministry of Internal Affairs, 2012. 280 p.
- Potekaev N. N. Rosacea. M.-SPb: ZASCH "BINOM Publishing House", "Nevsky Dialect", 2000. 144 p.
- Clinical recommendations. Dermatovenereology / Ed. A. A. Kubanova. M.: DEX-Press, 2007. 300 p.
- European guidelines for the treatment of dermatological diseases/Ed. A. D. Katsambasa, T. M. Lotti. M.: MEDpress-inform, 2008. 736 p.
- Kanada KN, Nakatsuji T., Gallo RL Doxycycline indirectly inhibits proteolytic activation of tryptic kallikrein-related peptidases and activation of cathelicidin // J Invest Dermatol. 2012, May; 132(5):1435–1442.
- Adaskevich V. P. Current dermatology. N.-Novgorod: Publishing house NGMA, 2000. 306 p.
- Parodi A., Drago F., Paolino S., Cozzani E., Gallo R. Treatment of rosacea // Ann Dermatol Venereol. 2011; 138, Suppl 3: S211–214.
- Djukic K. Recidivans Rosacea papulo pustulosa due to recidivans H. pylori. 9th EADV Spring Symposium, Verona, Italy. 2012, P. 183.
- Kennedy Carney C., Cantrell W., Elewski BE Rosacea: a review of current topical, systemic and light-based therapies // G Ital Dermatol Venereol. 2009; 144(6):673–688.
- Guide to dermatocosmetology / Ed. E. R. Arabian and E. V. Sokolovsky. St. Petersburg: Foliant Publishing House LLC, 2008. 632 p.
- Aksoy B., Altaykan-Hapa A., Egemen D., Karagoz F., Atakan N. The impact of rosacea on quality of life: effects of demographic and clinical characteristics and various treatment modalities // Br J Dermatol. 2010; 163(4):719–725.
- Nevoralova Z. A patient with steroid-induced rosacea, colitis ulcerosa and polymyositis successfully treated by oral isotretinoin-a case report. 9th EADV Spring Symposium, Verona, Italy. 2012, P. 179.
- Perlamutrov Yu. N., Saydalieva V. Sh., Olkhovskaya K. B. Comparative assessment of the effectiveness of various methods of treating rosacea // Bulletin of Dermatology and Venereology. 2011, no. 3. pp. 73–79.
- Yentzer BA, Fleischer AB Changes in rosacea comorbidities and treatment utilization over time // J Drugs Dermatol. 2010; 9 (11): 1402–1406.
- Zuuren EJ, Kramer S, Carter B, Graber MA. Fedorowicz Z. Interventions for rosacea // Cochrane Database Syst Rev. 2011; (3): CD003262.
- Dodina M.I. Clinical, immunological and morphological relationships in patients with rosacea during treatment with pimecroclimus. Author's abstract. for the job application Ph.D. honey. Sci. M., 2011. 25 p.
- Sparavigna A., Palmieri R., Caserini M. Derming SR l. Activity of P-3075, a new medical device based on potassium azeloyl diglycinate, on the microcirculation in patients with rosacea. 9th EADV Spring Symposium, Verona, Italy. 2012, P. 82.
- Goldberg J. David. Laser and light therapy. T. 1. M.: Reed Elsiver LLC, 2010. 187 p.
- Goldberg DJ Lasers and light sources for rosacea // Cutis. 2005; 75 (3 Suppl): 22–26; discussion 33–36.
- Dahan S. Laser and intense pulsed light management of couperose and rosacea // Ann Dermatol Venereol. 2011; 138, Suppl 3: S219–222.
- Dubrovina A. A. Correction of hemodynamic disorders in rosacea using high-intensity laser radiation. Author's abstract. for the job application Ph.D. honey. Sci. St. Petersburg, 2011. 20 p.
- Bernstein EF The pulsed-dye laser for the treatment of cutaneous conditions // G Ital Dermatol Venereol. 2009; 144(5):557–572.
- Bjerring P. Present and future trends of vascular and pigmented lasers. 9th EADV Spring Symposium, Verona, Italy. 2012, P. 157.
- Leonardo L. Combination treatments in laser dermatology. 9th EADV Spring Symposium, Verona, Italy. 2012, P. 128.
- Fratila A. Present and future trends in ablative and non-ablative fractional laser. 9th EADV Spring Symposium, Verona, Italy. 2012, P. 143.
I. Ya. Pinson*, Doctor of Medical Sciences, Professor I. V. Verkhoglyad**, Doctor of Medical Sciences, Associate Professor A. V. Semochkin***
*GBOU VPO First Moscow State Medical University named after. I. M. Sechenova Ministry of Health and Social Development of Russia, **GBOU DPO RMAPO Ministry of Health and Social Development of Russia, ***Clinic "Presidentmed", Moscow
Contact information for authors for correspondence