© Author: Z. Nelly Vladimirovna, laboratory diagnostics doctor at the Research Institute of Transfusiology and Medical Biotechnology, especially for SosudInfo.ru (about the authors)
Previously, when counting platelets according to Fonio, a laboratory diagnostic doctor measured only the diameter of these cells, distinguishing 4 groups of blood platelets (or Bizzocero plaques). Now there is no need to devote so much time to such calculations, if automatic hematological systems with software are put into the service of laboratory work, which will count the number of all formed elements separately, including platelets (PLT).
The device will not ignore the particular characteristics of blood cells - erythrocyte (MCV, RDW, HCT) and platelet indices: MPV (mean platelet volume), PDW (platelet distribution width), PCT ( platelet crit - thrombocrit). Upon completion of the work, the machine itself will draw a histogram curve in order to guide the doctor along the true path in the diagnostic search.
In this publication we will try to understand in detail what the MPV platelet index is.
Different characteristics of platelets
Fragments of megakaryocytes, giant bone marrow cells, anucleate blood plates - platelets (PLT - platelet), circulating in the blood, look like biconvex disks with a diameter of 1.8 microns to 4 microns. Young blood platelets are larger in size than mature cells, aged platelets are the smallest. In blood smears, platelets appear pale blue or lilac in color and are often collected in groups.
In an inactive state, platelets have a round or oval shape, but as soon as they “sense” a violation of the integrity of blood vessels and bleeding, they almost instantly change shape, increase up to 10 times in size, “acquire” pseudopodia and begin to stick together (platelet aggregation) . The blood platelets perform all these actions in order to rush in the form of a conglomerate to the scene of the accident, where the platelets that arrived earlier are already waiting.
Therefore, platelets are very prone to change their size , since they have a very important function in the human body - participation in vascular-platelet hemostasis or, more simply, these blood platelets help blood clotting in case of various damages in the microcirculation zone.
Platelet aggregation
Aggregation is the gluing of platelets together to form a plug (closes the wound). So, thanks to aggregation, the blood stops within 15 seconds. Therefore, the main function of aggregation is to stop bleeding by protecting the damaged vessel.
There are 5 types of aggregation, namely:
- Spontaneous - determined using venous blood, which must be placed in a special device where the blood is heated to 37°C.
- Moderate – must be determined during pregnancy.
- Induced - to obtain results, it is worth adding 4 substances to the plasma, namely adrenaline, collagen, ristomycin, ADP (adenosine diphosphate).
- Low – observed during menstruation, as well as with diseases of the circulatory system.
- High – associated with the formation of blood clots. Manifests itself in the form of numbness of the extremities and swelling.
Promotion
level of aggregation (hyperaggregation) occurs when blood moves poorly through the vessels, but quickly clots. This deviation occurs with the development of diabetes mellitus, oncology, hypertension, leukemia, sepsis, and atherosclerosis. In addition, this condition can lead to stroke, myocardial infarction, and thrombosis.
Hypoaggregation
(reduced level of aggregation) leads to poor blood clotting. As a result, small cuts can cause heavy bleeding. Most often, a decrease in aggregation should be observed in leukemia, oncology, anemia, and renal failure.
Aggregation during pregnancy
The normal aggregation value during gestation is 30-60%.
An increased level of aggregation can lead to miscarriage or spontaneous abortion. The main causes of hyperaggregation are severe toxicosis and dehydration.
A significant decrease in aggregation can lead to uterine bleeding both during childbirth and after the birth of the child. In this case, bruises occur on the body, gums bleed profusely, and nosebleeds also appear. So, the reasons for such a decrease may be: taking medications; toxicosis; allergy; lack of vitamins C, B12; poor nutrition.
To carry out the analysis, a device called the PLT aggregation analyzer is used. When collecting blood, venous blood is used (3 hours after waking up and on an empty stomach).
In the end, it is worth noting that in order to identify pathologies associated with blood clotting, it is worth taking into account not only the total level of platelets, but also the average volume, the coefficient of large platelets and other indicators, which are discussed in more detail in this material.
The large platelet ratio is a test that must be performed to determine the condition of the blood. Deviations from normal indicators can indicate various diseases. In this case, the level can either increase or decrease depending on the reason. A change in the level of cells in the blood indicates the presence of pathological changes in the human body. To understand what p lcr or large platelet ratio is responsible for and how to bring it back to normal, you need to learn more about these blood cells.
What does the MPV index mean?
When automatically processing blood samples, platelets are counted in the same channel with red blood cells - erythrocytes, so the hematology analyzer can separate particles by signal height in accordance with volume, which allows the device to immediately differentiate them:
- Macroplatelet cells (this group includes elements from 1.8 to 30 femtoliters - in principle, these are the cells that are currently interesting to us);
- Microerythrocytes;
- Fragments of red blood cells - schizocytes;
- Remains of the cytoplasm of white cells - leukocytes or, as it is called, cellular debris.
a – normal platelets b – platelets of different volumes (pronounced anisocytosis) c – huge macroplatelets
Meanwhile, this information alone is very little to characterize the state of platelets. At other times they would have been seen on a stained slide, but now most automated hematology analysis systems provide the various indicators present in the hemogram - mean platelet volume (MPV) and other platelet indices. The average volume of blood platelets is calculated by the automatic hemoanalyzer program using the formula:
MPV = [PCT,% x 1000] /
In addition, the device also includes a histogram for its calculations, which is subsequently studied by the doctor when deciphering the results.
Features of a blood test for platelet bodies
The platelet count is determined during a general clinical blood test. In modern times, this indicator is not calculated manually, but is used by automatic hematological analyzers - devices that simultaneously determine up to two dozen blood parameters, including the number and average size of platelets.
The device can draw a line of distribution of platelet bodies by volume. If there are predominantly young cells in the blood, then the graph shifts to the right. The more old elements in the plasma, the more pronounced the left side of the graph will be.
A few decades ago, equipment could only determine platelet levels. Modern diagnostics have much broader capabilities, including the ability to calculate the average platelet volume.
The device produces results in an unusual form - each indicator is represented by several letters of the Latin alphabet.
The vast majority of patients and even some providers do not understand what is printed on the study form.
Only a few drops of blood are required to determine MPV. The test allows you to determine the concentration and average volume of platelet elements.
A special feature of the platelet test is its speed - the study must be carried out no later than 2 hours after collecting the material. If you do this later, the test result will not be considered reliable.
Normal platelet bodies should be:
- in children in the first weeks of life (99 – 421)*10 9 /l;
- in adults (180 – 320)*10 9 /l.
If the average platelet volume is increased, this means that the bone marrow produces platelet bodies in excess, and they do not have time to be eliminated from the body. An excess of platelet elements in the plasma makes the blood thick and viscous.
If the analysis shows that the average platelet volume is increased, then you cannot independently draw conclusions about the presence of the disease.
When analyzing blood counts, you need to rely on many parameters. This work can only be done by a specialist. If necessary, the doctor will prescribe additional examinations and drug therapy.
MPV norm in general blood test
The average platelet volume - MPV is expressed in femtoliters - fl, fl (1 femtoliter = 1 cubic micron - µm2), depends on the age of the person (data are given in the table below) and normally ranges between 7.0 - 10.0 femtoliters. And in children from one to three years of age (on average), MPV in a general blood test performed by an automatic device gives higher values.
Table: Normal intervals for the MCV platelet index depending on age
| Age, years | Norm MPV, fl |
| Infants up to one year | 7,1 – 8,0 |
| Children from 1 year to 5 years | 8,1 – 8,9 |
| Children, teenagers and adults from 5 to 60 years old | 7,4 – 12,0 |
| Over 60 years old | 9,5 – 12,0 |
Meanwhile, all these norms and the table are very conditional. The reader can verify this for himself by looking for the boundaries of normal values in other sources. The whole point, as always, is in the reference intervals, which vary noticeably in different laboratories, where the norm falls within the range of 6.0 - 13 femtoliters, somewhere narrows its limits (7.4 - 10.4), so before you start worrying Regarding your own analyses, it is useful to ask what values are used by the CDL, which calculated these indicators.
Preparing and taking a blood test
General clinical and biochemical tests are taken in the morning, on an empty stomach. No special preparation required. The last meal should take place 10–12 hours before sampling. For 1–2 days, it is recommended to give up fatty foods, alcohol, and the use of medications that affect hematological parameters. If it is impossible to cancel therapy, you must notify the laboratory employee.
You cannot smoke on the day of the test. It is important to avoid stress before taking the test.
Both capillary and venous blood are used for MPV testing
The material for a hematological test can be capillary or venous blood. MPV is assessed within 2–3 hours after sampling. A later study may lead to false results.
What will the doctor think?
Having familiarized himself with the first results (calculation of platelet indices), the doctor can already imagine different situations regarding the behavior of representatives of the platelet unit in the bloodstream, the state of hemostasis and bone marrow hematopoiesis, taking into account only one indicator - the average platelet volume:
- MPV is within normal limits. In the circulating blood: cells that have not changed in volume, mature, but not old, full-fledged cells capable of performing their functional tasks at the proper level. The coagulation system and bone marrow are functioning normally.
- MPV increased. In the bloodstream, along with normal platelets, circulate young blood platelets, increased in size, and giant platelets, which, although they try, but, not having the qualities of full-fledged mature cells, have not acquired their capabilities, and therefore are not able to fully take assume the responsibilities of “healthy” elements of the platelet unit. There is a rush in the bone marrow, blood clotting is impaired.
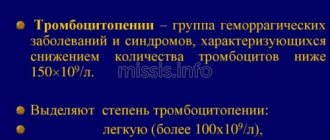
- MPV is below normal. In the blood: there are practically no cells of normal size; the platelet link in the bloodstream is represented by small aged platelets that have lost their functions. There are obvious deviations from the norm in hemostasis, bone marrow hematopoiesis is suppressed. Thrombopathy?
Based on studies of the morphological features of blood platelets, as well as on calculations of an automatic analyzer and a histogram, it is possible to discover the relationship between their volume and functional abilities (the adhesive-aggregation function of platelets, due to the content of biologically active substances in their granules).
With “growing up and aging,” the volume of plates decreases, which can be seen in the histogram recording. The presence of the overwhelming majority of young forms in the circulating blood causes the histogram to shift to the right, and the predominant distribution of old blood platelets in the bloodstream shifts to the left.
Platelets, their types and functions
Platelets (PLT, platelets) are blood cells with a diameter of 2-4 microns that provide blood clotting. The functions of platelets include angiotrophic (the ability to maintain the structure and functions of the walls of microvessels), adhesive-aggregation (formation of a primary platelet plug in damaged blood vessels), platelets are also involved in fibrinolysis, maintaining vasospasm, and blood clot retraction. These blood cells have the ability to transport circulating immune complexes on the membrane.
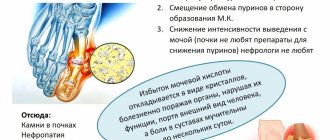
An increase in MPV may indicate the presence of thrombocytopenia, myeloproliferative diseases, posthemorrhagic anemia, hyperthyroidism, and diabetes mellitus.
There are five forms of platelets: young, mature, old, irritable and degenerative.
Platelets, like other blood cells, are produced in the bone marrow. Approximately two-thirds of the total number of platelets is in the bloodstream, and one-third is in the spleen. The precursors of platelets are megakaryocytes - giant cells with a large nucleus, from which platelets are released. Platelets are fragments of the cytoplasm of megakaryocytes surrounded by a membrane. They do not have a nucleus and their lifespan is approximately ten days. Platelet granules contain clotting factors, serotonin, calcium ions, adenosine diphosphate, peroxidase, platelet growth factor, von Willebrand factor, etc.
Platelets are round or oval in shape. When a blood vessel is damaged, they are activated, the cells flatten, form pseudopodia (long outgrowths) and acquire the ability to stick to other platelets (aggregation) and the walls of the damaged vessel (adhesion). A blood clot forms, which blocks the damaged area and thereby stops bleeding. Stimulators of platelet aggregation include serotonin, thrombin, collagen, and adrenaline. In a normal (inactive) state, the platelet membrane does not support coagulation reactions. There is a connection between the size of platelets and their functional activity, the content of biologically active substances in their granules, and their tendency to adhere.
Normally, the number of platelets in the blood is 180–320 × 109/l, varying depending on the time of year and time of day (daily fluctuations can reach 10%). A physiological increase in the number of platelets in the blood occurs when rising to altitude, in winter, after injury or exhausting physical activity. A physiological decrease in platelet count is observed before and during menstruation (up to 25–50%), as well as during pregnancy.
A significant decrease in MPV in the blood of a pregnant woman indicates a threat of miscarriage.
When the balance between the formation and destruction of platelets is disturbed, a tendency to thrombosis or increased bleeding occurs. With an increase in the number of platelets and the development of thrombosis, there is a risk of pulmonary embolism, stroke, myocardial infarction, and blockage of blood vessels in other organs by clots. A decrease in the number of platelets leads to hemorrhages and bleeding, which can also cause the development of life-threatening conditions.
The counting of platelets in the blood is carried out using an automatic hematological analyzer; in some cases, there is a need to determine the number of platelets and their sizes in stained blood smears under a microscope when calculating the leukocyte formula.
Platelet indices of a general blood test include:
- mean platelet volume (MPV);
- platelet distribution width by volume (PDW) – an indicator of platelet anisocytosis (depending on the predominance of young or old forms in the blood);
- thrombocrit (PCT) - indicates the proportion of blood volume occupied by platelets (depending on the total number of platelets and the MPV index).
Platelet indices allow you to assess the state of the blood coagulation system
Average platelet volume is increased
An increased average platelet volume can be a diagnostic sign of various (usually hematological) pathologies or act as a laboratory symptom accompanying certain diseases. For example, MPV is increased when:
- Idiopathic thrombocytopenic purpura (an autoimmune process that leads to massive death of blood platelets and intense bone marrow hematopoiesis) and other autoimmune diseases (SLE - systemic lupus erythematosus);
- Myeloproliferative processes;
- Hemorrhagic thrombocytodystrophy or Bernard-Soulier syndrome (rare hereditary disease, autosomal recessive transmission);
- Hereditary large-platelet thrombopathy (a disease characterized by large platelets, but their function is not impaired);
- May-Hegglin anomalies (familial thrombocytopenia, autosomal dominant inheritance);
- Anemic syndrome caused by acute blood loss;
- Thalassemia;
- Diabetes mellitus;
- Hypersplenism and enlargement of the spleen, which can be either isolated (rarely) or accompany various hematological pathologies, for example, myeloproliferative processes (massive death of blood platelets occurs in the spleen, and the bone marrow at this time works in emergency mode, releasing young cells into the bloodstream large sizes);
- Removal of the spleen (however, the MPV indicator in this case changes its values for a short time; soon after the operation it returns to normal);
- The first signs of the formation of a neoplastic process;
- Development of inflammatory reactions;
- Development and progression of the atherosclerotic process (especially in smokers);
- Thyrotoxicosis (high functional activity of the thyroid gland and an increase in the level of its hormones as a result).
An increased MPV is not always associated with the development of some pathology, for example, in people who actively puff on a cigarette, as well as on holidays and weekdays who drink strong drinks, the average volume of blood platelets is always increased.
What to do if MPV is higher or lower than normal
MPV is a marker for a number of serious diseases. If there is a deviation from the norm, additional tests may be prescribed: general urinalysis, biochemical blood test, coagulogram. If a myeloproliferative process is suspected, a bone marrow biopsy is performed. Patient management tactics depend on the etiological factor that caused the change in MPV levels.
Proper nutrition is one of the components of the prevention of blood coagulation disorders
Self-medication, in this case, is extremely dangerous, since some diseases progress quickly and pose a threat to life. Uncontrolled use of medications can lead to a deterioration in the patient's condition.
To prevent dysfunction of the coagulation system, you should:
- undergo regular preventive examinations;
- rational use of medications that affect the hematopoietic system;
- eat right, avoid consuming fatty foods;
- maintain proper drinking regime.
If the balance between the formation and breakdown of PLT is disturbed, the risk of blood clots or bleeding increases.
A blood test for MPV is taken in combination with other hematological parameters. Thrombocrit and other coagulation factors must be examined for the following symptoms:
- arterial hypertension;
- dyspnea;
- frequent nose and gum bleeding;
- the appearance of hematomas after minor mechanical impacts.
Timely consultation with a doctor prevents the development of severe forms of disease. Adults should have a hematology test at least once a year. Children are recommended to have their blood assessed twice a year.
Slightly low or low mean platelet volume?
A slightly reduced or even low average platelet volume is characteristic of a number of conditions that occur with inhibition of bone marrow hematopoiesis:
- Hypoplasia of the megalocaryocyte lineage (congenital pathology and acquired disease (this group of megalocarycytic hypoplasias also includes aplastic anemia);
- X-linked recessive thrombocytopenia with platelet microcytosis (Wiskott-Aldrich syndrome);
- Thrombocytopenia caused by septic conditions caused by various infectious agents (for example, thrombocytopenia in septic endocarditis);
- Myelodysplastic syndrome;
- Malignant processes localized in the bone marrow;
- Inflammatory diseases;
- Children have infectious diseases (measles, rubella, influenza), however, if adults are “lucky enough” to catch such an infection, then the MPV platelet index will react in a similar way;
- Myocardial infarction;
- Some kidney diseases;
- Severe damage to the liver parenchyma (cirrhosis).
The MPV indicator may also be reduced when carrying out various types of therapeutic measures affecting neoplastic processes:
- Chemotherapy treatment;
- Irradiation;
- Cytostatic therapy.
A low average platelet volume may be a sign of pregnancy pathology and, if in this situation the content of blood platelets is simultaneously reduced, then the threat of miscarriage should be suspected. In addition, a reduced average platelet volume is observed when using certain medications.
“Reading” blood: what factors influence the test result?
Useful articles / July 25, 2017
- A person begins taking a general blood test (CBC) from birth. Based on its results, it is possible to obtain information for the diagnosis of many diseases, assess their severity and monitor the dynamics of the treatment.
To evaluate the results of the OAC, special standards are used, but there are factors that influence the indicators. Can a person independently decipher the numbers of a general blood test? And what influences the deviation from the norm?
Manually or automatically?
In modern laboratories, not everything is yet subordinated to artificial intelligence. Yes, the vast majority of laboratories use automatic hematology analyzers to conduct a general blood test. In just a few minutes, the analyzer performs complex calculations of erythrocyte, leukocyte and platelet parameters. However, some defective cells may be identified incorrectly - destroyed, immature and deformed cells. In this case, a microscope is needed - on it the doctor examines the blood smear after examination with a hematoanalyzer.
“It cannot be said that a manual or automatic method of studying a general blood test is better; they complement each other,” comments Yulia KOCHKALDA, leading specialist in medical diagnostics . – Doctors working in the laboratory compare the indicators from the hemoanalyzer and microscopy, and if there is the slightest doubt, they will ask the patient to repeat the study.
What influences the result of the analysis?
Sometimes it happens that the result of a blood test differs from the norms that the patient can independently find on the Internet. The numbers vary for various reasons and do not always mean deviations in the body’s functioning. Therefore, we recommend that you do not engage in “blood reading” on your own and guess what this or that indicator means. Entrust the interpretation of the analysis to doctors and do not jeopardize your own health. But be sure to remember four factors that can distort a general blood test:
Physical exercise . It doesn’t matter whether a person has been involved in sports or for how long. The main thing is to be at rest 30-40 minutes before the test. It is advisable to limit exercise the day before blood sampling. Eating. It is not recommended to eat food earlier than 8 hours before the test. The day before donating blood, we advise you to exclude fatty and spicy foods from your diet. Menstruation. During critical days, a woman’s platelet count decreases. To avoid getting a false test, reschedule your blood donation to another day of your cycle. Taking medications . Many drugs affect the test result. Therefore, on the day of donating blood, do not take any medications; it is recommended to give up even vitamins. Before taking blood, consult your doctor; some medications should not be taken several days before the test.
Alarm bell: what does blood “say”?
What do changes in the general blood test signal?
What diseases may this indicate? We do not recommend making a diagnosis yourself based on a blood test. However, after consulting with a doctor, you can give yourself a “tour” of your own body and pay attention to the processes occurring in it. erythrocytes
| COMPONENTS | INCREASE | DEMOTE |
| erythrocytes | polycythemia; stay in the mountains; heart diseases; tumors that produce erythropoietin; stress; smoking; blood concentration during dehydration. | anemia; hemolytic crisis; renal failure; blood loss; bone marrow aplasia; influence of toxic substances and medications. |
| HEMOGLOBIN | polycythemia; staying at high altitude; conditions associated with hypoxia; tumors producing erythropoietin; stressful conditions; dehydration. | for all types of anemia; hemolysis of red blood cells; renal failure; bleeding; red bone marrow aplasia; taking certain medications; pregnancy. |
| HEMATOCRIT | prolonged hypoxia, dehydration, leukemia, tumor processes in the kidneys. | anemia, hyperhydration, hyperproteinemia, pregnancy. |
| MCV (mean erythrocyte volume) | B12 and folate deficiency anemia, kidney disease, alcohol abuse, myxidema, bone marrow aplasia, reticulocytosis, use of anticonvulsants. | with iron deficiency; hemoglobinopathies (thalasemia); anemia in chronic diseases; sideroblastic anemia; lead poisoning. |
| MCH (hemoglobin content in red blood cells) | hyperchromic and megaloblastic anemia, hypothyroidism, liver diseases, cancer. | long-term lead intoxication, thalassemia, hypovitaminosis B12, chronic inflammatory processes, iron metabolism disorders. |
| RETICULOCYTES | anemia; acute blood loss; anemia treatment. | aplastic anemia; anemia due to impaired maturation of red germ elements; liver diseases; condition after blood transfusion; chemotherapy. |
| NEUTROPHILS | for all bacterial infections; acute and chronic myeloid leukemia; generalized tumors; stressful conditions; with tissue necrosis; vasculitis; decompensation of diabetes mellitus; acidosis; taking lithium, glucocorticoids; adrenaline; for leukemoid reactions, sepsis, endocarditis, miliary tuberculosis and tumor metastasis. | with viral infection, aplastic anemia, radiation, agranulocytosis, immunosuppression, taking certain antibiotics, chemotherapy drugs, thyreostatics, analgesics, psychotropics. With lymphocytic leukemia and monocytic leukemia, there is a relative decrease in neutrophils. |
LYMPHOCYTES
| COMPONENTS | INCREASE | REDUCTION |
| LYMPHOCYTES | for chronic infections, tuberculosis, chronic limadenopathy, infectious mononucleosis, Hodgkin's disease, Addison's disease, idiopathic thrombocytopenic purpura. | for AIDS and related diseases, bone marrow damage after chemotherapy and radiation therapy, steroid treatment, Cushing's disease, aplastic anemia, neurological diseases. |
| MONOCYTES | for viral, parasitic and protozoal diseases, sarcoidosis, Crohn's disease, tumors. | for aplastic anemia, chronic lymphadenopathy, treatment with glucorticoids. |
| EOSINOPHILES | allergic diseases, bronchial asthma, parasitic infections, collagenosis, angioedema, Hodgkin's disease, skin diseases. | general decrease in immunity, extensive burns, infectious diseases, dysentery, acute appendicitis, stress, prolonged pain, intoxication of the body. Source: https://womanadvice.ru/eozinofily-ponizheny |
| BASOPHILES | chronic myeloid leukemia, hypothyroidism, mastocytomas and systemic mastotosis. | Infectious diseases, stress, pregnancy, Cushing's disease, hyperthyroidism, regular stress conditions, allergies with severe manifestations, active thyroid function, pneumonia, adrenal diseases. |
PLATELETS
| COMPONENTS | INCREASE | REDUCTION |
| PLATELETS | acute inflammatory processes in the intestines, conditions after removal of the spleen, myeloproliferative diseases, infections, blood loss, sideropenia, pancreatitis. | with enlarged spleen, liver cirrhosis, bone marrow damage, alcoholism, Helicobacter pylori infection, collagenosis, DIC syndrome, coagulopathies, septic conditions. |
| MPV (mean platelet volume) | idiopathic thrombocytopenic purpura, thyrotoxicosis, diabetes mellitus, myeloproliferative diseases, atherosclerosis, smoking, alcoholism. | splenectomy, Wiskott-Aldrich syndrome. |
| PCT (thrombocrit) | myeloproliferative diseases, splenectomy, iron deficiency in the body, viral diseases and inflammatory diseases of other etiologies, atherosclerotic process, diabetes mellitus, smoking. | apastic anemia, myelodysplastic syndrome, megaloblastic anemia, collagenosis, hemoblastosis, ionizing radiation, the use of certain medications, hematopoietic tissue tumors, intoxication, chronic renal failure, liver cirrhosis. |
| PDW (platelet distribution width by volume) | inflammatory process, anemia, postoperative period, blood loss. | myelodysplastic syndrome, leukemia, bone marrow metastases, thrombocytopenia, radiation sickness, chronic hepatitis. |
What indicators to check if MPV is outside the norm
The MPV parameter is useful in diagnosing various diseases related to the system that is responsible for blood clotting processes. It is important, however, to keep in mind that MPV is not the only measure of these processes.
It is necessary to analyze it along with other indicators related to blood cells:
- PDW – level of platelet anisocytosis; informs about the percentage of platelets that deviate from the rest in volume;
- PLT – platelet count in blood serum;
- P-LCR – percentage of large platelets.
In most cases, if abnormalities in the blood picture concern only the MPV index and not other parameters, there is no cause for concern. However, any deviations in morphology should be consulted with a physician.