Causes
The main causes of hypercalcemia are excess parathyroid hormone in the body (hyperparathyroidism), oncology and long-term use of calcium supplements. Hypocalcemia almost always develops against the background of parathyroid hormone deficiency, the production of which is responsible for the upper and lower parathyroid glands. By interacting with the hormone calcitonin (thyroid), the exchange of phosphorus and calcium in the body is regulated. Excess calcium, as well as deficiency, develops with deviations in the functioning of organs and systems.
Prognosis and prevention
Hypercalcemia is a severe and in some cases (especially in acute cases) a life-threatening pathological condition. In hypercalcemic crisis, the mortality rate is very high (60%). The frequency of deaths in chronic cases averages 20-25%. However, the prognosis is largely determined by the cause of the increase in Ca levels.
Prevention of this pathology consists in timely diagnosis and proper treatment of the diseases against which it develops. Before starting to take vitamin D or other medications that may increase Ca levels in the blood, a blood test should be performed to assess Ca levels.
Symptoms
The first signs of hypercalcemia may not be noticeable, and only a random blood test will indicate problems. The appearance of obvious symptoms of increased calcium in the blood depends on the duration of this condition, the rate of development, and the severity of the underlying disease. These symptoms manifest themselves in the main systems of the body: nervous, muscular, digestive, urinary, cardiovascular, eye and skin diseases. The patient's memory deteriorates, lethargy, drowsiness, depression, weakness and muscle pain, restless leg syndrome at night, loss of appetite, constipation, nausea, gag reflex and belching appear. Possible weight loss due to pancreatitis, cholelithiasis, stomach ulcers with high acidity. Arthritis, arthrosis, and gout develop. Hypocalcemia is often combined with a lack of potassium, which leads to excessive excitability of neurons. As a result, muscle spasms occur (shoulders, hands, larynx, facial muscles). Skin sensitivity is also impaired, and a burning sensation or numbness occurs. Hemorrhagic syndrome develops, which is manifested by increased bleeding. Blood clotting decreases. Dystrophic changes in tissues, dental defects, brittle nails, dull hair, dry skin occur, heart rhythm is often disturbed, and cataracts develop.
Diagnostics
The profile of a medical specialist supervising a patient with this pathology is determined by the cause that caused this condition. Most often, such patients are seen by endocrinologists, nephrologists, and oncologists. When interviewing the patient, it is necessary to clarify what medications he is taking. During the examination, the doctor pays attention to symptoms such as decreased muscle tone and suppressed tendon reflexes. An additional examination is prescribed, including:
- Laboratory research.
A biochemical blood test measures the level of albumin, urea, and creatinine. Of the electrolytes, in addition to total and ionized Ca, the concentration of phosphorus and chlorides is determined. The content of vitamin D (25OH-D) is studied. PTH, PTH-like peptides. Daily urinary Ca excretion is checked. If thyrotoxicosis or hypocortisolism is suspected, a blood test for hormones (TSH, free T4, cortisol) is performed. - Functional tests.
Special provoking tests provide invaluable assistance for differential diagnosis of the causes of this disorder. These include tests with native vitamin D, thiazide diuretics, and calcitonin. A steroid suppression test with prednisolone can be used to exclude a process not associated with increased PTH secretion. - Instrumental research.
To search for adenoma or hyperplasia of the parathyroid glands, ultrasound, computed tomography, and scintigraphy are performed. Densitometry is performed to determine bone mineral density, and renal ultrasound is performed to diagnose nephrolithiasis. If there are symptoms that raise suspicion of an inflammatory process in the lungs or a malignant neoplasm, radiography, CT scan of the lungs, abdominal organs, and mammography should be prescribed to identify them.
Differential diagnosis must be made based on the predominant symptoms. Insipidal syndrome must be differentiated from diabetes mellitus and diabetes insipidus. Muscle weakness and hypotension should be distinguished from that with muscular dystrophies, myasthenia gravis, and polymyositis. Neuropsychiatric symptoms require the exclusion of psychiatric diseases.
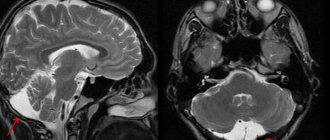
Scintigraphy. Parathyroid adenoma
Treatment
The initial stage of hypercalcemia, which is caused by excessive consumption of foods and medications containing calcium, can help solve the problem of a slight increase in the amount of calcium in the human body: changing the diet towards reducing the amount of foods containing large amounts of calcium. Dose adjustment, replacement or refusal of medications containing calcium. For healthy kidneys, sufficient consumption of water, preferably distilled (no more than 2 months). If hypercalcemia develops against the background of serious illnesses, then treatment is aimed at the underlying disease and cleansing the body of excess calcium. When the kidneys are functioning normally, calcium is usually washed out with the help of diuretics and intravenous saline. In severe conditions, hemodialysis is performed (cleansing the blood of waste products). If the process of increased removal of calcium from the bones cannot be stopped, then hormonal drugs are used. The main task of hypocalcemia is to compensate for calcium deficiency in the body. In addition, treatment is aimed at eliminating the cause of the disease. So, for hypoparathyroidism (lack of parathyroid hormone), hormonal therapy is prescribed. Chronic hypocalcemia is treated by regularly taking calcium tablets and vitamin D. In addition, measures are taken to normalize the levels of magnesium, potassium and protein in the blood.
Hypercalcemia
The first step in any unclear case of hypercalcemia is to measure PTH to confirm or rule out the diagnosis of pHPT. Along with the determination of iPTH, new measurement methods using specific amino-terminal antibodies have recently emerged. (Biointact-PTH, whole PTH). Application of PTH-Fragment-Assays obsolete. Other conditions that support the diagnosis of pHPT are hypophosphatemia, high-normal or elevated 1,25(OH)2D3 (with normal 25(OH)D3), elevated bone alkaline phosphatase, decreased to low-normal renal calcium excretion (as a result of increased renal PTH action and increased renal "calcium-Loads") and high renal excretion of phosphate (however, largely dependent on diet). Diagnosis of the localization of enlarged epithelial bodies before the first parathyroidectomy may be limited to ultrasonography of the neck, which in two thirds of cases determines the indicating condition. FHH (heterozygous inactivating mutation Calcium-sensing-Rezeptors) occurs with a frequency of 1: 15,000-20,000. Based on laboratory chemical results, it cannot be reliably distinguished from pHPT. The typical conditions for FHH are mild hypercalcemia and severe hypocalcemia; specificity is however limited. Family member screening for hypercalcemia and hypocalciuria can help make the diagnosis. The diagnosis can be made with confidence only at the present moment when the question is posed scientifically using Calcium-Sensing-Rezeptor-Gens sequencing. The distinction from pHPT is therefore important because FHH can generally be considered a non-therapeutic abnormality and unnecessary parathyroid surgery is not performed on affected patients.
It is assumed that about 70-80% of tumor-associated hypercalcemia are humorally mediated. The basis of most of these forms of hypercalcemia is the secretion of PTHrP from tumor tissue (often squamous cell carcinomas, such as renal carcinoma, bronchial carcinoma, and others). In the diagnosis of unclear hypercalcemia, one of the subsequent steps is also the measurement of PTHrP. Hematological malinomas (plasmacytoma, lymphoma), as a rule, do not produce PTHrP. In case of unclear hypercalcemia, using appropriate diagnostic measures (immunoelectrophoresis, as a mandatory study for any hypercalcemia, bone marrow puncture, radiological examination of the skeleton), plasmacytoma should be excluded. Plasmacytomas and lymphomas secrete cytokines (interleukin-1, tumor necrotizing factor a), which through the activation of osteoclasts lead to hypercalcemia. Systematic detection of these cytokines has no clinical significance.
If a tumor is suspected, a search program should be carried out with a thorough clinical examination (eg lymphoma, suspected skin changes, breast tumor, prostate enlargement), serological tumor markers, Haemoccult, chest X-ray (mass process), abdominal sonography (metastases) liver, kidney tumors) and radiological studies of the skeleton (scintiography, X-ray targeted images, detection of bone metastases, osteolysis, DD to pHPT, Morbus Paget). To diagnose unexplained hypercalcemia, a 1.25 (OH)2D3 measurement is performed. In rare cases, hypercalcemia may be caused by elevated levels of 1,25(OH)2D3. This most often indicates granulomatous diseases (most often sarcoidosis, less often tuberculosis and other diseases, see Table 2). Very rarely, ectopic lymphomas secernate 1,25 (OH)2D3.
Hypocalcemic crisis
An exacerbation of calcium deficiency is characterized by a decrease in plasma minerals to less than 2.25 mmol/l. A hypocalcemic crisis is also dangerous.
The attack can occur suddenly, but, as a rule, it is preceded by a number of symptoms:
- feeling of "goosebumps";
- tingling feeling throughout the body;
- limbs and part of the face go numb;
- severe muscle weakness;
- sudden muscle pain;
- depression;
- change in skin color.
Gradually, loss of sensitivity and other signs are replaced by muscle twitching. Initially, the patient feels only mild and isolated spasms, but quickly enough the condition develops into attacks of severe convulsions.
Muscle tone is expressed by characteristic manifestations:
- “the hand of the obstetrician”;
- "horse foot";
- "fish mouth";
- and others.
The danger arises when spasms affect the muscle tissue of internal organs: renal/liver colic, laryngospasm or bronchospasm. Impaired breathing can cause asphyxia.
At the moment of crisis, the patient feels unbearable pain, from which he loses consciousness and the ability to rationally perceive what is happening.
A little more about the symptoms
The clinical picture in both cases is pronounced. The main area of damage is the skeletal system, which contains more than 90% of the total calcium content in the body.
Symptoms of hypercalcemia, regarding bone tissue:
- pseudo- and simple form of gout;
- deformation;
- pain;
- muscle weakness and atrophy;
- fractures even with simple bruises;
- cystic bone formations.
In the severe stage, there is a sensation of “pins and needles”, numbness and burning in certain parts of the body, and temporary paralysis of the pelvic muscles may occur.
Hypocalcemia is characterized by seizures that can affect not only the limbs, but also the muscles of the chest. The danger comes from a hypocalcemic crisis, which causes serious complications.
What complications can it lead to?
When high calcium levels are accidentally detected, immediate action must be taken to avoid complications. Ignoring metabolic disorders can lead to:
- Osteoparosis. Lack of adequate treatment leads to calcium being released from the skeleton into the bloodstream. This becomes the main cause of thinning of bones and joints, which means bone fragility increases. Spinal curvature is observed in 85% of patients with hypercalcemia.
- Formation of kidney stones. The kidneys are a paired filtering organ that purifies the blood, which means they also accumulate calcium. Unfortunately, it is impossible to identify stones at an early stage. They make themselves felt when the situation has already started and blockage of the ducts or the movement of stones through the ureters begins, which is always associated with unbearable pain.
- Dementia and other central nervous system disorders.
- Heart rhythm disturbances.
The musculoskeletal system and kidneys are usually the first to suffer. If you have a frequent urge to urinate, you need to check not only your bladder, but also your blood for calcium levels.