Rheumatoid arthritis
is a chronic inflammatory disease of connective tissue that most often manifests itself in the small joints of the hands and feet.
The danger of the disease lies in its systematic nature and high degree of disability. Being an autoimmune disease, rheumatoid arthritis can affect almost any joint in the body
, and also often leads to
polyarthritis
(affecting 4 or more joints). It can also manifest itself in the organs of the body - the heart, lungs, eyes, kidneys, blood vessels and others. As a result, up to 70% of patients partially or completely lose their ability to work and the ability to self-care, and in especially severe cases left without treatment, even death is possible.
Rheumatoid arthritis affects 1 to 5% of people over 45 years of age, with women getting sick on average 3-5 times more often than men due to their naturally high immunity. Therefore, it is important to be attentive to the slightest manifestations of the disease, diagnose it in time and choose good drugs for rheumatoid arthritis in accordance with the doctor’s prescriptions.
Rheumatoid arthritis is a chronic inflammatory disease of connective tissue
The mechanism of development and causes of rheumatoid arthritis
The onset of the disease is often associated with a viral infection, injury, stress on a particular joint, hormonal imbalance, and renal failure. The joints most susceptible to damage are the knees, feet, wrists and fingers. When exposed to certain factors, the human immune system triggers an erroneous reaction: it mistakes a normal part of the body for a foreign object. As a result, substances begin to be produced that destroy the synovial membrane of the joints.
Currently, the reasons for the overactivity of the immune system leading to RA are unknown. The main suspected causes:
- Genetic factor
. A number of studies have revealed a high percentage probability of RA manifestation in close relatives in several generations. - Infectious agents
. There is reason to believe that the cause of the disease may be its infectious nature. This is most likely the Epstein-Barr virus, which causes rheumatoid manifestations. Other infectious causes may be: rubella virus, cytomegalovirus, mycoplasma, retroviruses, parovirus B19. Viral RA is acute and rarely becomes chronic. - Emotional stress
. There is a version that the development of the disease begins after a serious psychological shock. This explains the fact that women get sick 4 times more often than men.
General clinical recommendations
To prevent exacerbations of rheumatoid arthritis, it is necessary to reduce the activity of the pathological process. This can be achieved if:
- Lead a healthy lifestyle, follow a daily routine, avoid stress and high loads.
- Do not smoke, do not drink alcohol.
- Regularly perform exercises agreed upon with your physical therapy doctor.
- Follow the recommended diet.
- Treat concomitant diseases in a timely manner and eliminate foci of infection.
- Conduct courses of anti-relapse treatment for rheumatoid arthritis in a timely manner.
Rheumatoid arthritis requires a serious approach to treatment not only on the part of the doctor, but also on the part of the patient, who must follow all medical recommendations. At the Paramita clinic you will find such a serious approach to business. The main thing is not to delay your visit to the doctor!
Literature:
- Rheumatology: national guidelines. / Ed. E.L. Nasonova M.: GEOTAR-Media, 2008. 720 p.
- Karateev D.E. Retrospective assessment of long-term basic therapy in patients with rheumatoid arthritis // Scientific and practical rheumatology. 2003. No. 3. pp. 32–36.
- Chichasova N.V., Brodetskaya K.A., Igolkina E.V. et al. 18-month use of leflunomide - clinical effectiveness, tolerability and effect on the progression of erosive arthritis in patients with RA // Scientific and Practical Rheumatology. 2004, No. 2. Theses “School of Young Rheumatologists. No. 11, p. 124.
- Smolen JS, Landeve R, Breedveld FC et al. EULAR recommendation for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs // Ann. Dis. 2010, 69: 964–975.
- Emery P., Breedveld F.C., Hall S. et al. Comparison of methotrexate monotherapy with a combination of methotrexate and etanercept in active, early, moderate to severe rheumatoid arthritis (COMET): a randomized, double-blind, parallel treatment trial // Lancet. 2008, 372: 375–382.
- Dougados M., Emery P., Lemmel EM et al. When a DMARD fails, shoud patients switch to sulfasalazine or add sulfasalazine to continuing leflunomide? //Ann. Dis. 2005, 64: 44–51.
Themes
Joints, Pain, Treatment without surgery Date of publication: 03/26/2020 Date of update: 11/17/2020
Reader rating
Rating: 5 / 5 (2)
Types of rheumatoid arthritis
There are several types of RA:
- Seropositive
- rheumatoid factor (RF) is found in the patient’s blood - antibodies with which the body fights its G class immunoglobulins, which have undergone changes under the influence of infection. Antibodies group together and damage the joints. In this case, the disease progresses rapidly. - Seronegative
- RF is not found in the blood, the disease begins suddenly and sharply. - Systemic is
a very severe disease process that affects internal organs. Almost always leads to disability. - Juvenile or youthful
is a form of RA that affects children from 4 to 16 years of age. Large joints of the limbs are destroyed, significant growth retardation occurs, and internal organs are affected. - Still's disease
is a rare form of RA. The course of the disease occurs against a background of high temperature with damage to internal organs. In a third of cases, patients unexpectedly recover.
Medical Scientific and Practical Center for Vertebrology and Neuroorthopedics, Professor M.L. Kurganov
Rheumatoid arthritis is a systemic disease of unknown etiology with widespread damage to connective tissue, mainly in the joints, with erosive changes in them, with a chronic, often relapsing and progressive course. The trigger can be an infection, a cold, or an injury. The pathogenesis is also not fully understood, but it has been established that RA is caused by a pathology of immunity: the formation of autoantibodies to the f-fragment of immunoglobulin IgG, the circulation of immune complexes IgG-IgM-complement, which are fixed in the joint tissues and cause destruction of the synovial membrane. Neutrophils phagocytose immune complexes with the subsequent release of lysosomal enzymes and other inflammatory mediators, resulting in the development of synovitis. Continued inflammation stimulates the proliferation of the synovial membrane with the formation of pannus (granulation tissue), which creeps onto the cartilage and destroys it. Extra-articular changes may be caused by the penetration of immune complexes into the circulation, causing damage to other organs. In addition to external factors, in the occurrence of the disease, importance is attached to congenital and acquired internal factors, insufficiency of macrophage function. Some authors recognize the polygenic inheritance of predisposition to a number of related diseases. In this case, there is an inferiority of enzyme systems involved in the metabolism of phenylalanine, tyrosine, histidine and tryptophan. The culprit of primary immune changes may be congenital inferiority of the immune systems.
The assertion of the autoimmune nature of RA is based on the following:
1). Detection of manifestations of immunological reactivity in RA, including rheumatoid factor (RF) in the blood and synovial fluid, various categories of autoantibodies and immunocomplexes;
2). Negative results of the search for infectious origin;
3). Pathological studies have revealed similarities between the processes in the foci of inflammation in RA and the manifestations of autoimmune inflammation;
4). The clinical picture of the disease is chronic and progressive, characteristic of allergic and immune diseases, and in some cases responds well to immune therapy;
5). Pathologically, RA is characterized by progressive disorganization of connective tissue and the occurrence of synovitis.
As RA progresses, rheumatoid granulomas appear, consisting of a central zone of fibrinous necrosis surrounded by histiocytes. The proliferating synovium causes erosion of the articular cartilage, which begins to gradually deteriorate, leading to erosion of bone tissue. Subsequently, the articular capsule proliferates and the well-known picture of a rheumatoid joint develops (osteoporosis, usuration of articular surfaces, subluxations, ankylosis, etc.). Synovitis is often accompanied by tendovaginitis and bursitis, and sometimes the disease can begin with damage to the tendon-ligamentous apparatus.
RA varies widely in severity and degree of damage to various systems and organs.
When parenchymal organs are affected, articular-visceral forms of RA are diagnosed, usually developing in severe cases of the disease.
RA is also characterized by the development of vasculitis associated with immunological disorders. Vasculitis can occur with varying intensity, from clinically mild to pronounced forms, leading to damage to vital organs - kidneys (nephritis), lungs (pneumonia), eyes (iridocyclitis, uveitis). A very common complication of RA is amyloidosis, primarily of the kidneys, as well as the liver and adrenal glands.
RA affects people in their prime, most working age (20-45 years). The process in the joints continuously progresses, leading to ankylosis and complete immobility in the joints. Therefore, a large percentage of sick people lose their ability to work (15-20%). Based on this, it becomes clear how important early diagnosis of articular syndrome in RA is for the prognosis of the disease, since modern complex therapy in the early stage of the disease makes it possible to delay the progression of the process.
Rheumatoid Arthritis Clinic
When studying patient complaints, special attention is paid to:
1) pain in the joints, their nature (aching, gnawing), intensity (strong, moderate, weak), duration (periodic, constant), connection with movement;
2) morning stiffness in the joints, its duration;
3) appearance of joints (swelling, redness, deformation);
4) persistent limitation of joint mobility;
When examining a patient with RA, attention is paid to changes in the configuration of the joint in the form of swelling, deformation, and deformation.
Swelling is a uniform increase in joint volume, smoothing of their contours. This is due to effusion into the joint cavity and swelling of the periarticular tissues.
Defiguration is an uneven increase in the shape of a joint. The joint has an irregular shape due to a combination of exudation and proliferative phenomena.
Deformity is a gross violation of the shape of a joint due to bone changes (subluxations, contractures, ankylosis).
In a patient with RA, one can also note the presence of hyperemia of the skin over the inflamed joints, atrophy of the adjacent muscles, and subluxations. With subluxations in the proximal interphalangeal joints, the hand has the appearance of a “swan neck”, with subluxations in the metacarpophalangeal joints – “walrus flippers”.
Upon palpation you can detect: an increase in skin temperature over the surface of the joints; soreness of the affected joints; “lateral compression” symptom; muscle atrophy and skin thickening; subcutaneous formations in the joint area, most often the elbow, so-called rheumatoid nodules; Patellar balloting symptom to determine the presence of fluid in the knee joint.
The “bulge sign” is used to detect mild joint effusion. The knee joint should be fully extended and the muscles relaxed. The doctor presses with one hand on the joint from the medial side, towards the head end, expelling synovial fluid from this area. With the other hand, he applies pressure from the lateral side at the level of the middle of the patella. Even with a small amount of fluid, a protrusion soon appears on the medial side between the patella and the thigh. During valvation, crepitus in the joints is determined. It occurs when deformed articular surfaces rub against each other during active movement. After palpation, active and passive movements in the joints and mobility in various parts of the spine are examined. Muscle strength is determined using a dynamometer.
After a thorough examination of the joints, the condition of the internal organs is examined in detail to exclude or confirm visceral lesions. To confirm the activity of articular syndrome in RA, the following additional studies are used:
general blood test (leukocytosis, accelerated ESR), biochemical studies (CRP, sialic acids, protein fractions, dermatol test),
determination of RF (this is an antibody to the patient’s own globulin, changed in this disease, i.e. auto-antigen),
examination of synovial fluid,
X-rays of symmetrical joints.
Methods of morphological and radioisotope diagnostics of joint inflammation are also used.
The clinical picture of RA should include persistent arthritis. The inflammatory process primarily affects the metacarpophalangeal, proximal interphalangeal and metatarsophalangeal joints. Almost all joints can be affected. However, L.V. Ievleva and co-authors identified several clinical variants of the initial forms of the disease:
1) mono- and oligoarthritis with predominant damage to large joints, which in most patients over time turns into polyarthritis;
2) polyarthritis with persistent symmetrical damage, most often to small joints of the hands and feet. This option is the most common and does not present diagnostic difficulties;
3) polyarthritis, reminiscent of reactive infectious-allergic with transient exudative phenomena, easily treatable with non-steroidal anti-inflammatory drugs. As a rule, these arthritis are benign. However, long-term observation of patients showed that subsequently the patients develop either a typical picture or mono-oligoarthritis;
4) polyarthritis with fever and pain, morning stiffness, multiple and symmetrical damage to the joints with an inflammatory reaction in them, followed by a classic outcome;
5) polyarthritis with the presence of visceritis (carditis, nephritis, pleurisy, iritis, neuropathy, etc.). With this option, as a rule, persistent articular changes with a predominance of the exudative component are observed.
When diagnosing RA, you should pay attention to the following characteristic symptoms:
gradual or subacute onset of the disease with wave-like fluctuations in the severity of symptoms, slow but steady progression of arthritis, and involvement of new joints in the process;
feeling of morning stiffness; change in the shape of the joints (swelling, deformation, deformation) and hyperthermia of the skin over them, symmetry of arthritis. Typical deformities of the metacarpophalangeal (flexion contractures, subluxations), proximal interphalangeal (rheumatoid hand) and metatarsophalangeal joints with the formation of hammer-shaped fingers, their subluxations, flat feet (rheumatoid foot). As the disease progresses, extra-articular manifestations arise in the form of subcutaneous rheumatoid nodes, cutaneous vasculitis, and peripheral polyneuropathies. With a long course of the disease, many patients develop trophic changes in the skin, especially near the affected joints (thinning), atrophy of regional muscles, fragility and striation of nails, hyperhidrosis of the palms and soles, palmar erythema. The frequency of visceral manifestations ranges from 12 to 30%. This is heart damage in the form of myocardial dystrophy or myocarditis, pericarditis, and rarely endocarditis with subsequent formation of heart disease. Vascular damage is manifested by vasculitis involving small-caliber vessels. The kidneys change according to the type of focal nephritis, amyloidosis, nephrotic syndrome with renal failure. In addition, visceral lesions manifest themselves as acute pneumonia, chronic interstitial pneumonia with the development of focal and diffuse fibrosis. The liver may be enlarged as a result of amyloidosis, fatty degeneration, and reactive hepatitis. Common symptoms include increased fatigue, increased sweating, decreased appetite, and weight loss.
Laboratory test results are non-specific. In 70-80% of patients, rheumatoid factor is detected in the blood serum using the Waller-Rose reaction, latex test, and dermatol test. This form of RA is classified as seropositive. This arthritis is persistent, with relapses, in contrast to seronegative arthritis, which has a more favorable course. Accelerated ESR, increased fibrinogen, dysproteinemia, the appearance of CRP, altered sialic acid levels and other laboratory tests reflect the degree of activity of rheumatoid inflammation. But often the ESR accelerates over the course of months and even years.
All these symptoms are reflected in the classification of RA, where, in addition to clinical and anatomical manifestations (articular, joint-visceral, combined forms), clinical and immunological changes (seropositive, seronegative), course (slowly progressive, rapidly progressive), degree of activity (minimal, medium, high); X-ray stage, depending on the severity of bone changes from osteoporosis to the formation of ankylosis, as well as the functional ability of the patient.
Clinical and anatomical characteristics:
1. Rheumatoid arthritis:
- polyarthritis
- oligoarthritis
- monoarthritis
2. Rheumatoid arthritis with visceritis and lesions
- reticuloendothelial system of serous membranes, lungs, heart, blood vessels, eyes, kidneys, NS, amyloidosis of organs, pseudoseptic syndrome, Felty's syndrome.
3. Rheumatoid arthritis in combination:
- with DOA
- with diffuse connective tissue diseases.
- juvenile arthritis (including Still's disease)
Immunological characteristics:
- Seropositive
- Seronegative
Course of the disease:
- Rapidly progressive
- Slowly progressive
- No noticeable progression
Activity level:
- I Minimum
- II Average
- III High
- Remission
X-ray stage:
- I Periarticular osteoporosis
- II Osteoporosis + narrowing of the joint space (there may be isolated lesions)
- III Same + multiple patterns
- IV The same + bone ankylosis
Functional ability of the patient:
- I Professional ability to work is preserved
- II Professional ability to work is lost
- III Lost ability to self-care
Differential diagnosis.
Articular syndrome in RA must be differentiated not only from other inflammatory arthritis, but also from arthrosis, as well as from articular syndrome associated with other diseases. The doctor must be able to freely navigate among this vast labyrinth of diseases, in the clinic of which joint pathology is of no small importance.
Quite often, RA, which begins acutely or subacutely, resembles rheumatoid arthritis.
Articular syndrome in RA often has to be differentiated from articular syndrome in primary deforming osteoarthritis (especially in the presence of secondary synovitis). It is extremely important to carry out a differential diagnosis with articular syndrome in specific arthritis: tuberculosis, brucellosis, gonorrhea, dysentery. Tuberculous arthritis. Unfortunately, a patient with RA is sometimes mistakenly diagnosed with osteoarticular tuberculosis and then a plaster cast is applied, which leads to ankylosis and the joint loses mobility. To avoid mistakes in diagnosing tuberculous arthritis, it is necessary to clarify the following points:
1) a history of contact with tuberculosis patients;
2) signs of general tuberculosis intoxication (weakness, sweating, weight loss);
3) tuberculosis is characterized by a monoarthritis-like course of the disease, marked swelling of the joint covered with pale, stretched skin (“white tumor”);
4) the presence of leaky abscesses and fistulas with purulent discharge, in which tubercle bacilli can be detected;
5) positive Pirquet and Mantoux tests;
6) negative reactions to rheumatoid factor;
Brucellosis arthritis is established based on the following data:
1) the disease develops mostly in persons who have contact with animals infected with brucellosis (milkmaids, cattlemen, butchers) or with products obtained from sick animals (milk, meat, cheese, wool, leather);
2) the sacroiliac joint is relatively often affected with the appearance of a characteristic symptom of a “ripe watermelon”: when moving the legs apart in a bent position with active resistance to this from the patient, who is in a horizontal position on the back, a crunch appears in the sacroiliac joint;
3) positive tests (reactions) of Wright-Heddelson and Berne;
4) characteristic undulating fever;
5) involvement in the process of the liver and spleen (hepato- and splenomegaly), peripheral nerves (radiculoneuritis), joint capsules (bursitis), tendon sheaths (tenosynovitis).
Gonorrheal arthritis develops in individuals suffering from acute or chronic gonorrhea. It can be serous and purulent. Acute gonorrheal arthritis is of practical importance, since at first it is similar to acute RA, and in the later stages, like RA, it tends to ankylosis.
For the differential diagnosis of gonorrheal arthritis with rheumatoid arthritis, the following signs are important: anamnestic connection with gonorrhea, symptoms of urethritis, more often it is monoarthritis (gonitis), a positive Bordet-Hangu reaction, the presence of gonococci in the joint effusion. Dysenteric arthritis develops 6-8 weeks after dysentery and is characterized by a persistent and long-term course with a pronounced tendency to ankylosis of the joints.
Rheumatoid arthritis must be differentiated from Reiter's disease, which is characterized by a triad: urethritis, conjunctivitis, polyarthritis, but unlike RA, large joints of the lower extremities (knees, ankles) are affected, and arthritis, although it is long-lasting and persistent, rarely leads to ankylosis.
Articular syndrome in RA must be differentiated from psoriatic arthropathy, which is characterized by damage to the distal interphalangeal joints of the hands, the metacarpophalangeal joint of the first finger of the hand, the presence of psoriatic plaques, and damage to the nails. X-ray reveals an osteolytic process with different axial mixing of bones, periosteal overlays, absence of periarticular osteoporosis, signs of damage to the sacroiliac joint, paravertebral calcification. In addition, RA is also differentiated from gout, which is characterized by paroxysmal development of pain in the metatarsophalangeal joint of the big toe. The pain is accompanied by severe swelling of the joint, its hyperemia, and high temperature. Along the edge of the auricles, on the back of the joints of the fingers, and less often on the scalp, single, less often multiple tubercles (tophi) can be found due to the deposition of uric acid salts. The level of uric acid in the blood is increased to 0.5-1.2 mmol/l (normal 0.24-0.42 mmol/l). The patient’s lifestyle is also important for the diagnosis: inactivity, passion for rich food, meat foods, and alcoholic beverages.
The clinical diversity of RA variants creates significant difficulties in the differential diagnosis of the disease and similar syndromes, since many of them, especially at an early stage of development, can manifest predominantly as rheumatoid-like joint syndrome.
Sjögren's syndrome is a companion to a number of autoimmune conditions. It is more common with RA (7.4% and systemic lupus erythematosus (30%), and also occurs as an independent manifestation of autosensitivity (Sjögren's disease). Clinically manifested by polyarthritis with damage to the seretor glands (salivary, lacrimal, gastric). It is also called dry syndrome. In this case, dysphagia, achylia are observed, the absence of saliva and tears leads to the development of stomatitis, glossitis, conjunctivitis and keratitis.
Felty's syndrome. The main symptoms of the disease are rheumatoid arthritis, leukopenia and splenomegaly. In addition, hepatomegaly, lymphadenopathy, as well as anemia, lymphocytopenia and thrombocytopenia, and pulmonary fibrosis are often detected.
Still's syndrome is a kind of continuously relapsing disease in children aged 4-7 years with multiple symmetrical damage to the joints, involving internal organs in the process and a significant impairment of the general condition. The diagnosis is based on the following symptoms: polymorphic multiple erythema, polyarthritis similar to RA, carditis, splenomegaly, muscle atrophy, lymphadenopathy, severe anemia, hyperleukocytosis over 20,000, ESR up to 70-80 mm/hour, exhaustion.
Treatment.
The therapeutic aspects of RA are extremely diverse and include anti-inflammatory, immunosuppressive treatment and immunostimulation, as well as surgical and rehabilitation measures. The arsenal of drugs that have anti-inflammatory and at the same time analgesic activity is extremely wide, which makes it possible to successfully carry out this type of treatment in all patients, alternating and selecting the drugs that are most effective in each case. Of this group of nonsteroidal anti-inflammatory drugs (NSAIDs), the most widely used are:
a) derivatives of salicylic acid – acetylsalicylic acid (aspirin), salicylamide. They influence the bioenergetics of inflammation, have antipyretic and anti-inflammatory effects;
b) pyrazolone derivatives - butadione, rheopyrin, pyrabutol - inhibit the activity of proteolytic enzymes (plasmin), normalize permeability;
c) indole acid derivatives - indomethacin (metindole), usually used in doses of 0.025 g 3 times a day;
d) derivatives of alkanoic acids – brufen (ibuprofen) 0.2 g 3-6 times a day, voltaren (ortofen) 0.025 g 3-6 times a day. However, this therapy is more symptomatic than pathogenetic, so so-called basic therapy should become increasingly important. Basic drugs include:
a) gold preparations (sanacrisin, niocrisin, Salganal-B, domestic preparation krizanol). 1 ml of 5% crizanol contains 17 mg of gold. For the course of treatment, the patient should receive 1-1.5 g of metallic gold: one intramuscular injection per week, 10 times; 17; 34 and 50 mg (but no more) until the patient receives 1-1.5 grams of gold. It is necessary to pay attention to early signs of gold intoxication (occur in 30-60% of patients), which are expressed in the development of gold dermatitis, ulcerative stomatitis, nephropathy and thrombocytopenic purpura. In this case, it is necessary to attach importance to such signs as the appearance of itching in the interdigital folds, slight eosinophilia, which may be harbingers of the listed complications.
For mono- and oligoarthritis, radioactive gold is used by intra-articular injection. Gold salts suppress immunopathological reactions by inhibiting excess production of immunoglobulins, enzyme activity and redox processes in cells.
b) aminoquinoline agents (delagil, rezoquin, plaquenil). Due to their ability to inhibit the activity of plasma cells, these drugs have a weak immunosuppressive effect and can also inhibit the proliferative component of inflammation. They are used 0.2-0.25 g after dinner for a year. These drugs have a weaker effect on the course of the disease than all other means of “basic” therapy and are usually used in the early phase of the disease in the articular form with minimal and moderate activity of the process. If leukopenia, dermatitis, or symptoms of seasickness appear, it is necessary to reduce the dose of drugs or interrupt treatment.
c) immunosuppressants - used in severe torpid RA - generalized articular-visceral forms. pseudoseptic syndrome, in a variant bordering on systemic lupus erythematosus. Immunosuppressants are capable of suppressing the formation, development and function of immunocompetent cells and have a pronounced antiproliferative effect. Either antimetabolites that block the synthesis of nucleic acids (methotrexate, azathioprine) or alkylating agents (cyclophosphamide, chlorobutin, etc.) that have the ability to denature nucleoproteins are used. Immunosuppressive drugs are used in the following doses: azathioprine and cyclophosphamide 100-150 mg/day, maintenance dose 50 mg/day; chlorbutine (leukeran) 2 mg 3-4 times a day, maintenance dose 2 mg/day. Methotrexate 2.5 mg 2 days in a row (1st day 1 time, 2nd day 2 times a day) with a break of 5 days, only 7.5 mg per week, long-term.
Experience shows that the therapeutic effect of immunosuppressants, which usually occurs after 2-3 weeks, is not persistent, as a result of which, after improvement of the patient’s condition, the patient must (up to 1 year) be on maintenance doses. The therapeutic effect can be achieved in 60-70% of severe patients who are resistant to all other treatment methods. However, 40-50% of patients experience side effects of immunosuppressants - a decrease in the body's resistance to infections, dyspeptic disorders, significant leukopenia, thrombopytopenia, herpes zoster, progression of amyloidosis and renal failure. The immunostimulant levamisole (Dekaris) turned out to be insufficiently effective, and the possibility of developing serious side effects, especially agranulocytosis, serves as a basis for refraining from its widespread use in RA.
d) D-penipillamine (cuprenil). This drug has indirect immunosuppressive and anti-inflammatory effects. The effect occurs in 60-80% of patients after 8-12 weeks of treatment. Treatment begins with a dose of 250 mg/day and, with good affect, the drug can be prescribed for several months or even years. Indications for the use of D-penicillamine are active forms of RA that are resistant to the action of anti-inflammatory drugs and corticosteroids, as well as patients intolerant to gold preparations.
e) corticosteroids (prednisolone, prednisone, triampinalone, dexamethasone). The mechanism of action of these drugs is complex. GCS normalize capillary permeability, stabilize lysosomal membranes, and have a rapid anti-inflammatory, antiproliferative and immunosuppressive effect. Due to the wide range of side effects and complications that arise when prescribing GKOs, their use in RA should be limited only to highly active forms occurring with visceritis, vasculitis, and Felty's syndrome. Average doses of prednisone and prednisolone tablets are 15-30 mg/day, triamcinolone 12-16 mg/day, dexamethaone 2-3 mg/day.
Wider indications are for intra-articular injections of corticosteroids (hydrocortisone, Kenalog, Depomedrol, etc.), which are combined with the use of NSAIDs. Hydrocortisone is injected at 50-125 mg into large joints, 25-50 mg into medium joints and 5-10 mg into small joints; Kenalog (triamcinolone acetonide) is administered once every 2-4 weeks at a dose of 20-80 mg, depending on the size of the joint.
In case of persistent chronic arthritis with the presence of progressive osteochondral destruction, intra-articular administration of radioactive drugs - gold or yttrium - is indicated. These drugs cause necrosis and almost complete destruction of the synovial membrane of the joint (physical synovectomy), as a result of which foci of formation of pathological immune complexes disappear and a stable and long-term remission of the local inflammatory process occurs. Typically, 5 microcuries of radioactive gold or 5 microcuries of radioactive yttrium are administered per injection. A total of 3 injections of the gold preparation (about a month apart). When using yttrium, one injection is sufficient.
In recent years, applications of dimethyl sulfoxide (DMSO) in the form of a 50% solution in distilled water, alone or in combination with analgin (0.5 g), heparin (8500 units), hydrocortisone (12.5 mg) have been used to influence the local inflammatory process. daily for 25-30 minutes, a total of 10-15 procedures per course of treatment.
The activity of the rheumatoid process can be reduced through the general and local use of physical factors that have a desensitizing (UVR, X-ray irradiation, hydrogen sulfide and radon baths), as well as a resolving and analgesic effect (ultrasound, phonophoresis with hydrocortisone, sinusoidal currents, UHF, mud and paraffin applications, etc.).
Restoring the functions of the affected joints is achieved through the use of the above-mentioned physical factors, therapeutic exercises, massage, as well as surgical and orthopedic treatment. Therapeutic gymnastics prevents the formation of fibrous adhesions and ankylosis and should be used daily, starting from the earliest phase of the disease, after pronounced exudative phenomena in the joints have subsided. Prevention of exacerbation of RA is carried out in the process of long-term systematic monitoring of patients during clinical examination in rheumatology offices of clinics. During this period, the patient’s reactions to the continued use of basic therapy, as well as corticosteroids, should be monitored, their timely withdrawal or dosage reduction should be carried out, preventive courses of drug and physical therapy (local and general), exercise therapy should be applied, foci of infection are sanitized, indications for spa treatment are determined. treatment.
All patients with RA should be systematically observed and examined by a rheumatologist at the clinic. Patients with a slowly progressive course without visceritis are examined in the rheumatology office once every 3 months. In the presence of visceritis, patients are examined by a rheumatologist once every 2-4 weeks. Patients with a mild course, without noticeable progression during an exacerbation, usually receive quinoline drugs in combination with NSAIDs. Twice a year, patients undergo a course of preventive treatment with exercise therapy, massage, and physiotherapy). It is advisable to take one of these courses at a resort (Sochi, Pyatigorsk, Nalchik, Tskaltubo, Evpatoria, Saki, Odessa, etc.)
Thus, the described complex staged therapy of patients with RA is carried out at the stages of hospital - clinic - resort. With its long-term use, 70% of patients remain able to work, and the number of exacerbations and progression of the rheumatoid process are significantly reduced.
Juvenile rheumatoid arthritis
Juvenile idiopathic (causeless) arthritis (JIA)
- a childhood disease that manifests itself as chronic inflammation of large joints. Occurs with a frequency of 1:1000 children.
Main types of JIA:
- Oligoarticular
– 1-4 joints are involved, most often the wrist, ankle and knee. One joint of the fingers or toes may be affected. - Uveitis
is an intraocular lesion. It is an intra-articular manifestation of the oligoarticular form. - Polyarticular
– damage to 5 or more joints, mainly symmetrical joints are affected. - Systemic
– the lymphatic, nervous systems, liver, skin, lungs, spleen are affected. - Psoriatic
– a symbiosis of arthritis and psoriasis. - Enthesitis
is an associated arthritis; inflammation in the joints is accompanied by pain in the tendons and ligaments. Typically the hip joints are affected.
Advantages of the laboratories of JSC "SZTsDM"
At the laboratory terminals of the Northwestern Center for Evidence-Based Medicine, you can take tests to diagnose rheumatoid arthritis and other autoimmune diseases. Among the advantages of SZTsDM JSC:
- New modern equipment,
- Qualified and friendly staff,
- Quick availability of results and convenient ways to obtain them.
Laboratories are located in Pskov, Veliky Novgorod, Kaliningrad, St. Petersburg and other cities of the Leningrad region. You can take tests at any of them without being tied to residence or registration.
Symptoms of rheumatoid arthritis
RA usually begins with vague symptoms, increased fatigue and weakness are felt, then some stiffness is felt in the joints in the morning, which disappears in the evening. These are already the first alarming signs of a disease that will soon make itself felt with severe pain in symmetrical joints (knees, hips, ankles, jaws). Swelling and swelling appears around the diseased joints.
In the absence of therapy, fever and muscle pain will be added to the above symptoms.
Stages of the disease
Seropositive rheumatoid arthritis has 4 stages of development:
- The initial stage
is the development of the disease lasting up to 6 months; The main symptom is morning stiffness. - Early stage
– from six months to a year; the symptoms of polyarthritis are more pronounced, significant swelling of the joint tissues appears. - Advanced stage
– from one to two years with all clinical manifestations. - The late stage
– more than two years, is accompanied by joint deformities, contractures, disability and complications from internal organs.
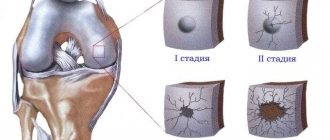
Radiological stages of seropositive arthritis:
- Development of osteoporosis of the articular surfaces of bones.
- Narrowing of the joint space, the beginning of the destruction of cartilage tissue.
- Significant destruction of cartilage and bone tissue of articular surfaces, deep erosion; subluxations;
- Closing of the joint space and the formation of ankylosis - immobility of the limb.
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
Diagnosis of rheumatoid arthritis
The symptoms of RA are similar to those of a number of other diseases (Lyme disease, gout, acute rheumatism, osteoarthritis), so diagnosing arthritis is quite problematic.
At the first appointment, the doctor will collect a clinical history and examine the patient. Then he will prescribe a series of tests, tests, and images. Will give directions for ultrasound and computed tomography. Based on the entire complex of studies, it is possible to make a diagnosis and prescribe treatment.
Forecast
Rheumatoid arthritis is a disease with a poor prognosis. This means that, despite the treatment, it is impossible to achieve a complete recovery. In addition, treatment drugs are extremely toxic.
The life expectancy of patients with rheumatoid arthritis is on average 5-10 years less than in the general population. In such patients, due to constant chronic inflammation, the risk of sudden cardiovascular death, internal bleeding, and infectious complications is increased.
Treatment of rheumatoid arthritis
Drug treatment
The use of medications is primarily aimed at eliminating pain and improving joint mobility. The following is used as symptomatic therapy:
- non-steroidal anti-inflammatory drugs;
- glucocorticosteroids;
- basic drugs.
Surgery
In case of untimely treatment and advanced types of RA, you will have to resort to surgical intervention. Which operation should be applied depends on each specific case. There are several methods of surgical treatment:
- endoprosthetics - replacement of the affected joint;
- arthrodesis – artificial immobilization of a destroyed joint;
- arthroplasty – replacement of destroyed articular surfaces with one’s own tissues or artificial pads;
- correction of the articular surface.
Physiotherapy
Physiotherapeutic procedures for RA will bring relief from severe pain and make periods of remission longer. At the time of exacerbation of the disease, the following are indicated:
- magnetotherapy:
- electrophoresis;
- laser therapy;
- ultraviolet.
During the period of remission:
- balneotherapy;
- UHF;
- ultrasound;
- mud therapy;
- sanatorium treatment;
- acupuncture.