A gastroenterologist treats diseases of the pancreas in Nizhny Novgorod.
The pancreas plays a huge role in the human body.
The pancreas is responsible for metabolic and digestive processes in the body.
The pancreas is the most important secretory organ of the human body.
Today, the most popular diseases of the pancreas are treated in Nizhny Novgorod - pancreatitis, pancreatic necrosis, cancer, cysts and diabetes.
Acute pancreatitis.
Acute pancreatitis is an acute inflammation of the pancreas.
Acute pancreatitis usually appears against the background of a person’s abuse of alcoholic beverages and previous alcohol poisoning.
Acute pancreatitis can also be caused by:
- improper or poor quality nutrition (eating fatty, spicy foods, frequent overeating);
- urolithiasis – the presence of kidney stones;
- heredity;
- trauma to the pancreas: previous operations, injuries, mechanical damage;
- uncontrolled use of medications, antibiotics;
- endocrine diseases, hormonal disorders.
- infections and viruses.
Symptoms of acute pancreatitis in Nizhny Novgorod.
The main symptom of pancreatitis is acute pain in the epigastric region, hypochondrium (right and left). Over time, the pain begins to become encircling, affecting the back, lower and lateral areas of the abdomen.
Detection of acute pancreatitis in Nizhny Novgorod.
If you suspect the development of pancreatitis in the body, the gastroenterologist prescribes the following set of examinations:
- a general blood test, which allows you to find out about the presence of an inflammatory process;
- Ultrasound of the abdominal cavity, which allows you to see changes in the internal organs;
- a general urinalysis to detect amylase in the urine, the presence of which indicates the development of pancreatitis;
- FGDS.
Classification
Depending on the predominance of damaging mechanisms, three forms of the disease are determined:
- Adipose – with increased lipase activity, pancreatic adipose tissue is destroyed. After lipase appears outside the pancreatic capsule, it acts, provoking the appearance of areas of necrosis in the layers of the peritoneum, the greater and lesser omentum, the mesentery, and internal organs. aseptic peritonitis and multiple organ failure subsequently develop .
- Hemorrhagic - with increased elastase activity, microcirculatory disorders predominantly develop, resulting in vasospasm . For a short time - several days, and sometimes hours - toxemia provokes paresis of the vascular wall, vasodilation, and blood flow in the gland tissues slows down. This leads to a sharp increase in the likelihood of blood clots and, later, ischemic necrosis . Initially, the vascular wall is destroyed thicker than the pancreas, and later in other organs. The consequence of all these processes is hemorrhage into the retroperitoneal tissue and internal organs. The main symptom that characterizes hemorrhagic pancreatic necrosis is effusion into the abdominal cavity with the presence of blood in it. The disease develops rapidly, so in doctors’ reports you can often see the conclusion: “The cause of death is hemorrhagic pancreatic necrosis.”
- Mixed - with approximately the same activity of elastase and lipase, the signs of fat necrosis and hemorrhagic imbibition are equally pronounced.
Depending on the prevalence of pathological manifestations, two forms are defined:
- local (one area affected);
- diffuse (two or more areas are affected).
Depending on the rate of progression:
- progressive;
- sluggish.
Depending on the depth of the lesion:
- surface;
- deep;
- total.
Depending on the course of the disease:
- recurrent;
- progressive;
- retrogressive;
- fulminant;
- abortive.
Depending on the severity of the manifestations of the disease, several of its degrees are determined:
- Mild degree - as a rule, this is edematous or diffuse necrosis with small foci.
- Medium degree - diffuse or local with more pronounced foci.
- Severe degree - diffuse or total with large foci.
- An extremely severe stage - pancreatic necrosis is accompanied by complications leading to irreversible consequences and death.
Chronic pancreatitis.
Chronic pancreatitis is diagnosed when the disease develops as a result of a protracted inflammatory process occurring in the pancreas. Men over 40 are most susceptible to the disease.
Symptoms and causes of chronic pancreatitis in Nizhny Novgorod.
The most common causes of chronic pancreatitis are the presence of cholelithiasis in the patient and excessive consumption of alcoholic beverages.
Eating fatty, low-quality foods, carbonated drinks, and alcohol also contributes to the development of chronic pancreatitis.
The presence of chronic pancreatitis is indicated by cutting pain. Also, belching, vomiting, bloating, problems with bowel movements, lack of appetite, weight loss are symptoms of chronic pancreatitis.
Methods for diagnosing chronic pancreatitis at Only Clinic.
If chronic pancreatitis is suspected, a gastroenterologist at the Only Clinic prescribes the following set of examinations to the patient:
General blood test: with chronic pancreatitis, there is an increase in the concentration of leukocytes in the blood, an increase in the erythrocyte sedimentation rate, and an increase in amylase levels.
- General urinalysis: shows an increase in amylase.
- Ultrasound of the abdominal cavity and pancreas.
- CT, MRI to identify foci of disease and the presence of stones.
For what reasons can pancreatic necrosis develop?
Pancreatic necrosis develops for the same reasons as acute pancreatitis. People who regularly break their diet are considered to be at risk. For example, they eat a lot of fried and spicy foods, and also abuse alcoholic beverages. In particular, many people suffering from alcoholism are at risk of developing chronic pancreatitis, which will ultimately be complicated by destruction of the pancreas, that is, pancreatic necrosis.
A provoking factor for the development of the disease is the consumption of alcohol or, in more rare cases, fatty foods. This is due to the fact that alcohol provokes increased secretion of pancreatic hormones. The pressure in the ducts of the organ increases, which provokes tissue swelling and destruction. As a result, the enzymes secreted by the gland are activated without leaving the organ, which leads to self-digestion of the pancreas.
Destroyed tissues enter the blood, causing the patient to develop symptoms of intoxication. The liver, heart and kidneys suffer from breakdown products. Encephalopathy often occurs as a complication of pancreatic necrosis.
Pancreatic necrosis.
Pancreatic necrosis is a severe form of pancreatitis, which results in changes in the parenchyma of the pancreas that are degenerative and destructive in nature.
Pancreatic necrosis is more common at a young age, women are most susceptible to it.
Causes of pancreatic necrosis.
Among the causes of pancreatic necrosis, gastroenterologists most often name cholelithiasis, cholecystitis, unhealthy diet, complications after surgery or injury, abuse of alcohol, nicotine, drugs, infections, viruses.
Symptoms of pancreatic necrosis.
Symptoms of pancreatic necrosis are pain in the abdominal area.
Repeated vomiting, attacks of nausea, constant dry mouth, skin pigmentation, attacks of shortness of breath, even at rest, may also indicate pancreatic necrosis; feeling of weakness, mental restlessness and tension.
Methods for diagnosing pancreatic necrosis.
To diagnose pancreatic necrosis, the same studies and tests are used as for pancreatitis.
Publications in the media
Regarding the treatment of this disease, you can contact the Department of X-ray surgical methods of diagnosis and treatment of the Clinic of Faculty Surgery named after. N.N. Burdenko
Acute pancreatitis is an inflammatory-necrotic lesion of the pancreas caused by enzymatic autolysis caused by various reasons. Etiology • Diseases of the biliary tract (cholelithiasis, choledocholithiasis, stenosis of the papilla of Vater) • Alcohol excess and rich fatty foods • Surgical interventions on the pancreas and adjacent organs, abdominal trauma with damage to the pancreas • Acute circulatory disorders in the gland (vessel ligation, thrombosis, embolism) • Severe allergic reactions • Diseases of the stomach and duodenum (peptic ulcer, parapapillary diverticulum, duodenostasis) • Endoscopic retrograde cholangiopancreatography • Viral infections (mumps) • Drugs (azathioprine, estrogens, thiazides, furosemide, sulfonamides, GC and valproic acid) • Hypercalcemia, hyperparathyroiditis, uremia • Kidney transplantation.
Pathogenesis • Enzymatic autolysis of gland tissue with the development of a demarcation inflammatory reaction and the formation of microthrombi • The progressive course of the disease is characterized by pancreatogenic toxemia, hemodynamic disturbances, inhibition of the activity of parenchymal organs and post-necrotic complications. Pathomorphology. Autolysis, interstitial edema, hemorrhages, cellular and fat necrosis are noted in the pancreas.
Clinical and morphological classification • Edematous form of pancreatitis • Fatty pancreatic necrosis • Hemorrhagic pancreatic necrosis. Clinical picture • Constant severe girdling pain and pain in the epigastric region, accompanied by nausea and vomiting • The abdomen on palpation is painful, tense and moderately swollen • Positive symptoms of Shchetkin-Blumberg, Voskresensky, Mayo-Robson, Razdolsky. The severity of symptoms depends on the form of the disease, the degree of intoxication and complications • The skin and mucous membranes are often pale, sometimes cyanotic or icteric. Mondor's syndrome, Gray Turner's symptom, and Cullen's symptom appear. The body temperature with edematous pancreatitis is normal. • With pancreatic necrosis, pain is most pronounced in the epigastric region. With the progressive course of pancreatic necrosis, on the 7th–10th day of the disease, abdominal pain decreases due to the death of sensory nerve endings in the pancreas. Also characteristic is a serious condition, vomiting, increased body temperature (37.7–38.3 °C), cyanosis of the skin, tachycardia, arterial hypotension, oliguria, and symptoms of peritonitis. Symptoms of Grunwald and Davis are characteristic. Often, symptoms of intoxication prevail over local manifestations of the disease • With parapancreatic phlegmon and abscess of the pancreas, deterioration of the condition is noted: increased body temperature, chills, inflammatory infiltrate in the upper floor of the abdominal cavity, leukocytosis with a shift in the leukocyte formula to the left • Severe inflammation and necrosis of the pancreas can cause bleeding into the retroperitoneal space, which can lead to hypovolemia (arterial hypotension, tachycardia) and accumulation of blood in soft tissues. Laboratory tests • CBC - leukocytosis (10–20109/l) with a shift of the leukocyte formula to the left • Biochemical blood test •• Increased content of α-amylase - 95% of cases (decreases with pancreatic necrosis) •• Increased ratio of amylase to creatinine clearance (higher 5%), which is normally 1–4% •• Increase in Ht to 50–55% •• Moderate increase in ALT and/or AST with concomitant alcoholic hepatitis or choledocholithiasis •• Moderate increase in ALP concentration with concomitant alcoholic hepatitis or choledocholithiasis •• Hyperbilirubinemia - in 15–25% of patients •• Increased levels of serum lipase •• Hyperglycemia in severe cases •• Hypocalcemia on the first day of the disease.
Special studies • Plain radiography of the abdominal organs - signs of dynamic intestinal obstruction, accumulation of gas in the area of the lesser omentum (abscess inside or near the pancreas); displacement of the abdominal organs (exudation and swelling of the lesser omentum and organs adjacent to the pancreas); blurred shadows of the iliopsoas muscles with retroperitoneal necrosis of the pancreas • X-ray contrast study with a barium suspension is used to diagnose pathology of the upper gastrointestinal tract: an increase in the radius of the horseshoe of the duodenum due to edema of the pancreas is possible; with relaxation duodenography, a pillow symptom can be detected • X-ray examination of the chest organs - pleural effusion (rare) • Ultrasound of the pancreas - decreased echogenicity, edema, thickening in the anteroposterior direction, virtual absence of tissue between the pancreas and the splenic vein • CT scan of the pancreas (high resolution) • Selective celiacography: with edematous pancreatitis - increased vascular pattern; with pancreatic necrosis - narrowing of the lumen of the celiac trunk, deterioration of the blood supply to the gland with areas of vascular bed exclusion • Radioisotope study with pancreatic necrosis - lack of fixation of the isotope in the pancreas, decreased excretory function of the liver • Endoscopic retrograde cholangiopancreatography • Laparoscopy - foci of fat necrosis, hemorrhage and edema of the gastrocolic ligaments, exudate in the abdominal cavity (serous or hemorrhagic), assess the condition of the gallbladder.
Differential diagnosis • Penetrating or perforating gastric and/or duodenal ulcer • Acute cholecystitis • Choledocholithiasis • Mesenteric vascular obstruction and/or infarction • Perforation of internal organs • Obstructive intestinal obstruction • Aortic aneurysm • Pancreatic cancer • Acute appendicitis • Ectopic pregnancy • Posterior MI • Hematoma of the muscles of the anterior abdominal wall • Blunt trauma or penetrating injury to the spleen.
TREATMENT Diet. Fasting is prescribed for up to 7 days; after reducing the severity of pain, you should eat small meals with a high carbohydrate content, limiting fats and proteins (to reduce the secretion of pancreatic enzymes). Expansion of the diet in accordance with the patient's condition. Management tactics • For edematous form of pancreatitis •• Nasogastric tube and gastric drainage - for vomiting, nausea •• IV solutions of glucose, Ringer-Locke (1.5–2 l), rheopolyglucin (lowers blood viscosity, prevents the aggregation of formed blood elements, leading to improved microcirculation and reduced swelling of the pancreas), hemodesis (binds toxins and quickly removes them in the urine) •• Lytic mixture: trimeperidine, atropine, diphenhydramine, procaine •• Protease inhibitors: aprotinin •• Moderate forced diuresis •• To relieve spasm of the sphincter of Oddi and blood vessels - papaverine hydrochloride, atropine, platyphylline, drotaverine, aminophylline •• Antihistamines (promethazine, chloropyramine, diphenhydramine) - to reduce vascular permeability, analgesic and sedative effects •• Perinephric procaine blockade and splanchnic nerve blockade for relief inflammatory process and pain reaction, reducing the external secretion of the pancreas, normalizing the tone of the sphincter of Oddi, improving the outflow of bile and pancreatic juice. These manipulations can be replaced by the administration of 0.5% procaine solution intravenously •• On 3–5 days, patients are discharged, as a rule, in satisfactory condition.
• For pancreatic necrosis (treatment of fatty and hemorrhagic pancreatic necrosis is carried out in the intensive care unit) •• For rapid restoration of blood volume and normalization of water and electrolyte metabolism - intravenous administration of solutions of glucose, Ringer-Locke, sodium bicarbonate, as well as rheopolyglucin, hemodez, and then plasma, albumin with simultaneous stimulation of diuresis •• Lytic mixture, protease inhibitors, cytostatics •• Cytostatics (for example, fluorouracil) have an anti-inflammatory, desensitizing effect and (most importantly!) inhibit the synthesis of proteolytic enzymes •• Protease inhibitors (aprotinin) suppress the activity of trypsin, kallikrein, plasmin, forming inactive complexes with them. They are administered IV every 3–4 hours in loading doses (for example, aprotinin up to 80–320 thousand units/day) •• To force diuresis - IV mannitol 15% solution 1–2 g/kg or furosemide 40 mg •• For an infectious process (for example, in the lungs, bile ducts or urinary tract) - broad-spectrum antibiotics. Data on the effectiveness of antibiotics for the prevention of purulent complications in the pancreas are contradictory. In case of an infectious lesion of the pancreas, antibiotic therapy is necessary •• To reduce the external secretion of the pancreas, cold applied to the epigastric region, aspiration of gastric contents, intragastric hypothermia are indicated •• UV laser irradiation of blood (15 min each, 2-10 sessions) relieves pain and inflammation , improves the rheological properties of blood and microcirculation •• Extracorporeal detoxification methods (plasmapheresis, lymphosorption) are aimed at removing pancreatic enzymes, kallikrein, toxins, and cellular decay products from the body •• Close-focus radiation therapy has an anti-inflammatory effect. 3–5 sessions are performed •• In case of progression of signs of peritonitis, surgical drainage of the cavity of the lesser omentum and abdominal cavity is indicated.
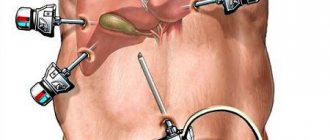
Surgical treatment is carried out in case of • Ineffectiveness of conservative therapy - drainage of the omental bursa and abdominal cavity, necrectomy • Inability to exclude acute surgical disease of the abdominal organs • Symptoms of diffuse peritonitis • Combination of acute pancreatitis with destructive cholecystitis • Pancreatitis caused by an impacted gallstone - endoscopic retrograde cholangiopancreatography , sphincterotomy and stone removal • Severe blunt trauma or penetrating injury to the abdomen.
Complications • Toxic •• Pancreatic shock •• Delirium •• Hepatic-renal and cardiovascular failure • Post-necrotic •• Pancreatic abscess •• Phlegmon of the retroperitoneal tissue •• Peritonitis •• Erosive bleeding •• Cysts and pancreatic fistulas. Prognosis • Signs detected upon admission •• Age over 55 years •• Leukocyte count in peripheral blood more than 16109/l •• Fasting blood glucose concentration above 11 mmol/l •• LDH activity in the blood above 350 IU/l •• AST content more than 25 IU/l • Signs detected 48 hours after admission •• Drop in Ht by more than 10% •• Increase in blood urea nitrogen content to 1.8 mmol/l •• Serum calcium concentration below 2 mmol /l •• paO2 below 60 mm Hg •• Base deficiency more than 4 mEq/l •• Loss of fluids into the third space - more than 6 l • If less than 3 of the above signs are present, mortality is 1%, 3–4 - 16% , 7 - 90%, more than 7 - 99% • 85–90% of cases of edematous form of acute pancreatitis resolve spontaneously, mortality 3–5%.
ICD-10 • K85 Acute pancreatitis • K90.3 Pancreatic steatorrhea
Forecast
The prognosis for pancreatic necrosis is unfavorable. Even if a person receives timely treatment, this does not protect him from repeated attacks. And besides, as practice shows, with this disease the mortality rate is 60%, and among these patients there are those who underwent surgery to remove the affected areas of the gland.
The chances of overcoming this disease depend on several factors:
- age;
- degree of disease;
- the presence of other pathologies in the patient;
- the presence of postoperative complications if surgery was performed;
- the extent of gland damage;
- duration of pathological processes.
If a person still manages to overcome the disease, he receives disability. At the same time, he must be attentive to his health and adhere to a diet. Patients who have suffered pancreatic necrosis are prescribed some contraindications that are related to work activity. They cannot work in enterprises that require:
- physical fatigue;
- emotional stress;
- work with pancreatic and hepatotropic poisons.
They should also not work in organizations with irregular schedules that force them to violate their diet and nutrition regimen. In addition, those who have managed to recover will need to regularly visit the doctor and undergo preventive examinations every 3-5 months. Since even after complete cure of necrosis, the risks of its reoccurrence still remain.
2. Reasons
As a rule, among the main causes of pancreatic necrosis are alcohol abuse and cholelithiasis, and in the history of patients with established pancreatic necrosis, these factors occur in a proportion of approximately 60% to 40%, respectively. However, it would be wrong to consider these two reasons as exclusive: in some cases, neither the first nor the second is relevant. Other risk factors include:
- abdominal trauma (including due to surgery);
- bacterial, viral, fungal infections with severe course, parasitosis;
- peptic ulcer of the stomach and duodenum;
- specific diseases of the biliary system (eg, dysfunction of the sphincter of Oddi);
- significant errors and distortions in the diet (abuse of fried, spicy, fatty foods);
- intoxication (in particular, compounds of boron, phosphorus, etc.);
- long-term use of certain groups of medications and opiate drugs;
- hereditary predisposition, autoimmune disorders (hypothetically).
Some authors consider it necessary to emphasize that today not all causes and risk factors for the development of pancreatic necrosis may be known.
Visit our Gastroenterology page
4.Treatment
Therapy of pancreatic necrosis requires inpatient conditions, especially since in many cases patients are hospitalized urgently with an attack of acute pancreatitis and “acute abdomen” syndrome. Further, everything depends on the causes and dynamics of the process, the degree of damage and localization. In some cases, drug blocking of the self-destructive activity of the pancreas is sufficient to relieve acute symptoms, but more often (especially in emergency cases) the situation develops according to a resuscitation protocol and requires the intervention of a complex surgical team. The prognosis, as shown above, is not always favorable: some types of pancreatic necrosis are fatal or, at least, deadly. If the critical phase is overcome, long-term treatment is necessary with a number of strict restrictions, primarily regarding diet.
A factor of exceptional importance is the timeliness of seeking special help: in simple words, the pancreas is not to be trifled with, and at the first symptoms of its dysfunction, you should immediately and definitely see a gastroenterologist.
Types of necrotic processes
Like any other disease, pancreatic necrosis has its own classification. Depending on the extent of its spread, this disease is divided into:
- to focal (necrotic processes are observed only in certain areas of the pancreas, for example, in the tail or head);
- extensive (when most of the organ is affected).
According to the speed of development, necrosis can be:
- sluggish (develops slowly);
- progressive (develops very quickly).
Extensive pancreatic necrosis
Based on the type of pathological process, this disease is divided into:
- to hemorrhagic;
- hydropic;
- hemostatic;
- destructive;
- functional.