CC dossier
Inna Wilhelmi
operating obstetrician-gynecologist of the Center of Urology and Gynecology of the ANO Clinic NIITO, Novosibirsk
Areas of interest: genital prolapse, urogynecology, aesthetic gynecology, laparoscopy, endometriosis
Every tenth patient who consults a gynecologist complains of chronic pain [1]. The term “pelvic pain” refers to pain localized in the lower abdomen, lumbar region and sacrum, as well as in the perineum, external genitalia, vagina and rectum.
Usually this is a symptom of an underlying disease, but chronic pelvic pain syndrome (CPPS) itself is also distinguished. Currently, there is no uniform terminology, and increasingly, instead of the term CPPS, the term “chronic perineal-pelvic pain and dysfunction syndrome” is used, which better reflects the essence of this disease.
Definition
Chronic pelvic pain syndrome is a condition characterized by:
- nonspecific pelvic pain of uncertain onset, present for at least 6 months
- absence of changes in organs and tissues that can explain the severity of the pain syndrome
- significant decrease in quality of life [4].
About 15–30% of all medical consultations are carried out for pain symptoms that are not medically explained [2, 3]. Often, thorough studies conducted by doctors of related specialties: gynecologist, urologist, proctologist, neurologist, show the absolute norm.
Types of lower abdominal pain
The nature of the pain may vary:
- pulling;
- pricking;
- aching;
- cramping;
- bursting;
- blunt;
- cutting;
- encircling;
- burning, as if burning from the inside.
Unpleasant sensations can begin abruptly and intensely, increase gradually, disturb the right, left or middle, radiate to the lower back and other areas. It can last for several minutes or days, stop intermittently or be constant.
The causes of lower abdominal pain in women can be divided into several main categories:
- physiological, caused by changes in the body;
- gynecological diseases;
- problems in the urinary system;
- disorders of the functioning of the intestines and diseases of the digestive system;
- other pathologies and conditions.
In choosing specific research methods and making the correct diagnosis, clarifying the nature, duration, and intensity of pain is of great importance. By studying the symptoms, doctors can assume a certain disease and outline the necessary direction in examining the patient.
Pathogenesis
The pelvic organs are closely interconnected, have a common afferent and efferent innervation, and blood circulation, so damage to one organ often involves neighboring organs in the pathological process [5, 6]. However, initially, women with chronic pelvic pain syndrome turn primarily to gynecologists. Sometimes, after an incorrect diagnosis, surgical treatment of pelvic pain is performed (hysterectomy, presacral neurectomy, dissection of the uterosacral ligaments), which leads to aggravation of the clinical picture.
A risk factor for chronic pain syndrome is previous ineffective treatment of the underlying disease. In case of untimely and insufficient relief of acute pain, the pain sensitivity threshold decreases, persistent generators of pathological impulses arise, and the nociceptive system is activated. Chronic pain loses its connection with damage to the pelvic organs and is maintained through complex central mechanisms, acquiring the status of a disease itself. Constant pain leads to the formation of psycho-emotional disorders, which, in turn, further stimulate the process of chronic pain syndrome [7].
Not all patients with predisposing factors develop chronic pelvic pain. What matters is the woman’s personality type, lifestyle features, social status, level of intelligence, marital status, etc. Thus, single women with a low income, low social status, prone to depression, neuroses are typical patients at the appointment of a gynecologist, neurologist, urologist with complaints of pain of an unspecified nature.
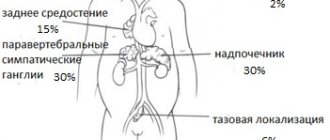
In chronic pelvic pain syndrome, the autonomic nervous system plays a major role in conducting and intensifying pain impulses. Irritation of sensitive receptors of the autonomic nervous system is perceived as a diffuse pain sensation, of unclear localization, with blurred boundaries.
Overview of Chronic Pelvic Pain
The cause of pain can be organic or infectious diseases, then they talk about chronic pelvic pain.
In some cases, no pathology is detected or the severity of pain does not correspond to the severity of the proven changes. In this case, a diagnosis of chronic pelvic pain syndrome (CPPS) is made.
Impaired blood microcirculation and increased excitability of the nervous system play a role in the development of CPPS. In conditions of lack of oxygen and nutrients, nerve endings transmit impulses that are perceived by the brain as pain.
Therefore, the treatment plan includes:
- therapy of the underlying disease;
- physiotherapy - improves blood circulation;
- decreased excitability of the nervous system - affects the peripheral and central parts of the nervous system responsible for the perception of pain.
Chronic pelvic pain syndrome in women: symptoms
Women suffering from pelvic pain typically have complaints such as:
- heaviness, discomfort, pain in the lower abdomen or lumbar region
- painful menstruation (dysmenorrhea)
- dyspareunia (pain during, immediately before, or after sexual intercourse)
- vulvodynia (burning or stabbing pain in the perineum and vestibule of the vagina)
The pain can be cyclical or constant. A connection with the menstrual cycle most likely indicates a gynecological pathology (often endometriosis or inflammatory diseases). Ovulatory pain regularly appears in the middle of the menstrual cycle, dysmenorrhea is sometimes so severe that it deprives a woman of her ability to work these days. However, due to the presence of viscero-visceral connections, the cyclic nature of pain does not always exclude pathology of neighboring organs.
Particular attention is paid to the patient’s lifestyle, social status, financial situation, obstetric history, surgical interventions, sexual disorders. With prolonged existence of pelvic pain, women become irritable, sleep disturbances appear, performance decreases, and ultimately they lose interest in life, up to the development of depressive, hypochondriacal conditions, decreased quality of life and social maladjustment [8, 9]. Therefore, in case of pronounced affective symptoms of chronic pelvic pain, it is advisable to immediately schedule a consultation with a medical psychologist, psychiatrist or psychotherapist.
Treatment
Pre-hospital assistance
Patients with pelvic fractures are placed on a backboard and given an anesthetic. In other cases, rest is recommended, sometimes taking analgesics, using local warming and anti-inflammatory drugs is acceptable. Pain in the pelvic bones often indicates the presence of serious pathologies that require prompt diagnosis and early treatment, so if this symptom is present, you should immediately seek professional help.
Conservative therapy
Patients with fractures undergo an intrapelvic block, apply skeletal traction, or are prescribed bed rest using a special position. Therapeutic tactics for other lesions depend on the characteristics of the disease. The following methods are used:
- Protective mode
. Patients are advised to limit physical activity. Sometimes it is necessary to use crutches or a cane. - Drug therapy
. Taking into account the characteristics of the pathology, antibiotics, NSAIDs, analgesics, chondroprotectors and other drugs can be prescribed. - Physiotherapy
. UHF, drug electrophoresis, magnetic therapy and other techniques are indicated. Exercise therapy, massage, and manual therapy are prescribed.
For malignant neoplasia, radiation therapy or chemotherapy may be used.
Diagnostics
There is no single algorithm for the examination and treatment of patients with CPPS. A diagnostic search always begins with a thorough collection of complaints and anamnesis of the disease and life.
According to the International Association of Chronic Pelvic Pain, there are 6 obligate signs for this disease:
- duration of pain syndrome is at least 6 months
- low effectiveness of therapy
- discrepancy between the intensity of the patient's pain and the severity of tissue damage
- presence of signs of depressive disorder
- progressive limitation of physical activity
- presence of depression, hypochondria
The complex of basic examinations for CPPS includes:
- A thorough examination with bimanual vaginal and rectal examination, general clinical examination.
- Screening for STIs (especially herpes and chlamydial infections).
- Ultrasound of the pelvic organs, kidneys, bladder, abdominal cavity, including assessment of blood flow in the pelvic vessels with the Valsalva maneuver and changing body position; in some cases, MRI or MSCT of the pelvis is justified.
- X-ray examination of the lumbar, sacral spine, pelvic bones in two projections, irrigoscopy, urography, densitometry.
- Endoscopic examination methods: hysteroscopy, cystoscopy, fibrogastroscopy, colonoscopy.
- Consultation with related specialists: therapist, urologist, neurologist, surgeon, gastroenterologist, proctologist, psychologist.
- Diagnostic laparoscopy if less invasive diagnostic methods are unsuccessful.
How do you find out the cause of pain? Diagnostics
A diagnostic search for the causes of pelvic pain is impossible without a thorough analysis of the woman’s complaints and medical history . Everything is important here: the nature (pulling, cutting, pressing, etc.) and localization of pain (in the middle, right, left, in the sacrum, rectum, bladder), its duration, in case of unstable pain - the frequency of its occurrence, connection with provoking factors (movement, body position, diet, urination, sexual contact).
the menstrual cycle (during menstruation, after, between menstruation, before it) and data on previous pregnancies or concomitant infertility is extremely important . Clarification of this connection often provides the key to understanding the causes of the disease. In addition, the doctor must know everything about the characteristics of the menstrual cycle and sex life of a woman, as well as about any sexually transmitted diseases and vaginal discharge.
Since pain is often associated with other organs, the doctor should ask in detail about the function of the intestines and urinary organs, concomitant diseases of the musculoskeletal system, and previous operations.
A general and gynecological examination is required . Already at this stage, it is possible to exclude the possibility of a major pelvic pathology (tumor), as well as establish the localization of painful sensations.
Based on the survey and examination, the doctor will be able to identify some types of pain syndromes, which significantly narrows and facilitates the further search for the cause. These syndromes include:
- Dyspareunia - painful sexual intercourse
- (Algo)dysmenorrhea - painful menstruation
- Ovulatory pain is cyclical pain in the middle of the menstrual cycle associated with ovulation.
- Pain in the vagina, external genitalia, and perineum (may be associated with infection, tumor, neuropathy, vulvodynia)
- Painful bladder (causes: infectious process, interstitial cystitis, bladder stones and tumors, consequences of previous surgeries)
- Pain associated with filling and bowel movement
- Neuropathies of the sciatic and pudendal nerves
Additional research.
The doctor takes vaginal and cervical discharge for analysis to rule out the possibility of an infectious disease. It is recommended to conduct a cytological examination of a scraping from the cervix. An ultrasound examination of the pelvic organs is always performed In some cases (suspicion of endometriosis of the recto-vaginal septum, retroperitoneal tumors, suspicion of pathology of the pelvic lymph nodes), magnetic resonance imaging .
Most patients with pelvic pain require diagnostic laparoscopy. Laparoscopy is the most useful minimally invasive examination method, allowing direct examination of the pelvic organs and the entire abdominal cavity. Laparoscopy is the only reliable method for identifying foci of endometriosis in the peritoneum, as well as adhesions. If during a laparoscopic examination formations of the appendages, foci of endometriosis, and adhesions are detected, then during the same intervention they are surgically treated. That is why laparoscopy is an indispensable research method and the first (and sometimes sufficient) method of treating identified diseases.
If corresponding diseases of related organs are suspected, examination and treatment is carried out by a urologist, gastroenterologist, proctologist, neurologist, or psychotherapist. Accordingly, depending on the expected diagnosis, the doctor will prescribe an additional examination.
Digestive problems
Pain in the lower abdomen may also occur due to problems with the intestines or existing diseases of different parts of the digestive system:
- Poisoning from low-quality food contaminated with bacteria. For example, with shigellosis, eschirichiosis and other infections, the pain is paroxysmal and pronounced.
- Hernias of inguinal, Spigelian and white lines. When they are pinched, acute painful sensations occur in the abdominal cavity.
- Pancreatitis. When the pancreas is inflamed, the left side of the lower abdomen and chest hurts, and jaundice may occur.
- Intestinal colic. Characterized by spasm of the large or small intestine. It can be the result of helminthic infestation, food poisoning, or severe stress.
- Cholecystitis. When the flow of bile is disrupted, the risk of developing gallbladder inflammation is high. In this case, the pain spreads to the right side, shoulder or shoulder blade.
If pain occurs accompanied by diarrhea or constipation, changes in the color of stool, the appearance of blood or mucus in the stool, bloating, nausea, vomiting, frequent bowel movements, chills or fever, the cause of such symptoms may be a disorder of the digestive function, organ diseases Gastrointestinal tract.
Gastrointestinal pathologies
There are many diseases of the gastrointestinal tract that require treatment for pelvic pain
, along with eliminating the root cause that caused them.
| Disease | Clinical manifestations | Diagnostics | Treatment |
| Adhesions due to surgery, inflammatory processes, injuries | Painful pulling sensations in the abdomen, radiating to the pelvis and lower back. |
|
|
| Irritable bowel syndrome |
|
|
|
| Chronic colitis |
|
|
|