Lactation mastitis - symptoms and treatment
Which doctor treats mastitis?
A mammologist treats mastitis. In severe cases, the help of a surgeon may be required.
Drug treatment
Treatment of lactostasis and lactation mastitis in women in different clinical situations is not the same. After the diagnosis of “lactostasis” is established, an injection of antispasmodics (for example, Drotaverine) is performed to relax the smooth muscles of the milk ducts. In case of severe pain, retropectoral blockade is performed with a solution of local anesthetic (Novocaine) and NSAIDs are prescribed. Some authors[1] recommend injecting 0.5 ml of Oxytocin or Pituitrin before pumping. Then the milk is expressed by manual massage or using a pump.
When lactostasis is eliminated, the compaction in the gland disappears or decreases, as does the pain syndrome. If within 3-4 hours after pumping the pain syndrome has not decreased, then it is legitimate to change the diagnosis to “serous lactation mastitis”. In this case, it is necessary to perform a puncture of the lesion, perform an ultrasound, prescribe painkillers and begin empirical antibiotic therapy. When a diagnosis of mastitis is made, breastfeeding is stopped[8].
There are a number of indications for stopping lactation:
- rapid development of the inflammatory process;
- any recurrence of mastitis;
- long-term chronic course of mastitis;
- infiltrative purulent, abscessing, phlegmonous and gangrenous mastitis.
To interrupt the process of milk synthesis, prolactin secretion inhibitors (Bromocriptine)[6] and dopamine antagonists (Cabergoline, Pergolide) are used. Non-drug methods of stopping lactation (bandaging the mammary glands, limiting drinking, refusing to pump) are not recommended in the treatment of mastitis.
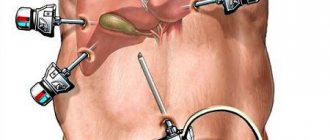
Surgery
Indications for urgent surgical treatment of mastitis: the presence of a purulent cavity, the rapid development of inflammation, the onset of destructive changes in the mammary gland. In this case, the purulent cavity is opened, pus and a mass of dead tissue are removed, after which the patient requires long-term dressings and washing of infected surgical wounds. It is also necessary to conduct a microbiological study of the nature of the wound microflora and its sensitivity to antibiotics[4].
Depending on the severity of the patient’s condition, infusion, detoxification, and restorative therapy may be performed. With the development of sepsis or septic shock, mediastenitis, inflammation in the pleural cavity, additional operations may be required to drain the corresponding cavities and spaces. Treatment of such patients continues in intensive care units.
Is it possible to breastfeed with mastitis?
Breastfeeding during mastitis can and should be done, because adequate emptying of the mammary glands is the main method of treating the disease.
But it's important! Before starting drug treatment with antibiotics, painkillers, etc., breastfeeding should be completely stopped so that drug metabolites do not enter the baby’s body along with the milk.
Is it possible to make compresses for mastitis?
For mastitis (not to be confused with lactostasis), thermal procedures are contraindicated. You can make applications with medications, for example Levomekol, as prescribed by your doctor.
Traditional methods of treating mastitis are not very effective. Without timely and adequate treatment, dangerous complications can develop, such as inflammation of the lymph nodes and sepsis.
How to distinguish lactostasis from mastitis?
Differential diagnosis is the most important point in choosing treatment for mastitis. In order to treat mastitis in a nursing mother, it is necessary to be able to distinguish it from lactostasis.
The main diagnostic sign of mastitis is the development of intoxication and flu-like syndrome, an increase in temperature above 38 C, axillary lymphadenopathy, and severe pain. With lactostasis, the state of health does not change much, since there is no intoxication, and the temperature rises to 38 C.
What are the different forms of mastitis?
There are several classifications; when making a diagnosis, the doctor identifies the type of pathology depending on the conditions of its occurrence. This gradation includes two forms of mastitis:
- Non-lactational – rare and not associated with breastfeeding. Usually it is predisposed to injury, hypothermia, and infection entering the gland through the blood or lymph.
- Lactation - most diseases are represented by this form. It develops after childbirth, is acute and requires immediate treatment.
The doctor indicates the type of mastitis in the medical history. This classification is paid attention to when prescribing therapy. If a non-lactational form is diagnosed, testing may be expanded to look for the cause.
According to the clinic, several types of mastitis are distinguished:
- infiltrative - when swelling of local tissues is noted, compactions appear;
- serous - with this form, fluid accumulates in the intercellular space, symptoms are moderate;
- abscess – characterized by limited purulent inflammation;
- phlegmonous – a diffuse purulent area is observed;
- gangrenous – accompanied by the death of glandular tissue;
- chronic infiltrative mastitis - accompanied only by local symptoms.
There is also a classification according to the prevalence of pathological changes - mastitis can be superficial and deep. The latter is divided into several forms, the most dangerous is panmastitis, in which the entire area of the gland is inflamed. When making a diagnosis, the classification of pathology is written in detail.
Diagnosis of the disease
Acute mastitis is diagnosed during a medical examination and tissue palpation. The procedure allows you to find out the localization of the inflammatory process, check for symptoms, and collect information on your medical history. The chronic form requires differential diagnosis with a tumor process, mastopathy and other diseases of the mammary glands. Based on the results of the preliminary diagnosis, the doctor will refer you for additional examination using instrumental and laboratory methods.
Basic techniques:
- Ultrasound of the mammary glands - reveals characteristic thickening of the subcutaneous tissue, expansion of the milk ducts, shows the location of infiltration zones, abscesses and necrotic areas;
- aspiration biopsy of the breast with histological examination of the inflammatory infiltrate;
- collecting milk for bacteriological testing (for lactation mastitis);
- mammography (rarely prescribed, only in controversial cases of chronic disease).
Diagnostics
Diagnostics plays an important role, since timely identification of the problem will allow for effective therapy and quickly eliminate the inflammatory process. The patient must carry out the initial diagnosis independently. This will allow you to identify the first symptoms of mastitis, suspect the presence of the disease and seek help from specialists.
When visiting a doctor, an examination is carried out and complaints are identified. The specialist palpates the breast, which allows you to make a diagnosis and determine a list of further examinations to determine effective treatment tactics.
Depending on the situation, the patient may be prescribed the following tests:
- general blood analysis;
- discharge from the nipples, to identify the causative agent of infection and sensitivity to antibiotics;
- examination of milk for the presence of bacteria and leukocyte levels.
To accurately determine the location of inflammation, as well as its extent, an ultrasound examination is performed. If the clinical picture is questionable, a biopsy is prescribed to rule out the possibility of cancer. The list of studies may vary and depend on factors such as the presence of concomitant diseases, the stage of mastitis, and so on.
Treatment of mastitis
When treating acute mastitis in the infiltration (induration) stage, conservative methods are limited. The complex of therapeutic measures includes systemic drugs - antibiotics, analgesics, antihistamines, as well as local procedures - cold, compresses with antiseptics. Regular expression of milk from the affected gland is mandatory.
Surgeons treat purulent mastitis. Such patients are treated in a surgical hospital. The operation of opening a purulent focus is usually carried out under anesthesia. This allows the surgeon to fully inspect the abscess cavity, and if the process spreads deeper, to identify possible additional purulent cavities. In addition, general anesthesia allows you to take a sample of breast tissue for histological examination if the diagnosis is in doubt. Local anesthesia is allowed only when opening small, limited mastitis.
Prevention
It is almost impossible to completely exclude the possibility of the disease. However, you can reduce it to a minimum. To do this, it is enough to carry out a number of preventive measures:
- It is necessary to breastfeed regularly, as well as express the remaining milk after each procedure.
- When feeding, you need to properly attach the baby to the breast. The baby should be able to grasp the entire areola. This prevents damage to the delicate skin of the nipples.
- Timely treatment of inflammatory processes occurring in the body also reduces the chances of mastitis.
- Before and after each feeding, you need to prepare your breasts. The nipples are washed with warm water and then gently wiped with a clean towel.
Preventive measures also include self-examination of the mammary glands and regular visits to a specialist.
Mechanism of disease development
Pathogenic microorganisms enter the woman’s mammary gland through blood or microcracks in the nipples. After this, the pathogens begin to actively multiply and secrete waste products that have a detrimental effect on the human body. As a result, the first symptoms of mastitis appear in the form of fever and general malaise.
The immune system responds to the inflammatory process by producing white blood cells designed to suppress the source of infection. This is accompanied by dilation of blood vessels and the appearance of characteristic signs of mastitis.
Symptoms of mastitis
Unlike many diseases, mastitis is characterized by the appearance of pronounced symptoms even at an early stage. This allows you to consult a doctor in a timely manner and undergo a course of therapy to prevent further development of the infection. Among the main symptoms are:
- pain in the affected area;
- increase in breast size;
- breast lump;
- malaise and weakness;
- headache;
- increased body temperature;
- change in skin color in the breast area;
- deterioration of milk flow;
- swelling of the skin of the breast;
Each stage of the disease is characterized by certain signs of mastitis. At the initial stage, thickening of the mammary gland and an increase in body temperature appear. These symptoms are enough to suspect the disease and undergo a professional examination to make an accurate diagnosis.
Acute and chronic mastitis: causes of pathology
The main cause of the disease is an infectious process. The main culprit is Staphylococcus aureus, less often other types of bacteria (Staphylococcus epidermidis, streptococci, enterococci, E. coli). The infection is activated under the influence of unfavorable factors - both external and internal. Among them:
- Hormonal imbalance in the reproductive system weakens the body's defenses. Reason: prolonged mental and physical stress, treatment with hormonal drugs, steroid use (in particular among athletes), chronic endocrine diseases.
- Decreased immunity - gives the green light to various infections, including opportunistic microorganisms. Reason: hypothermia, poor diet, stress, lack of vitamins, microelements, fresh air.
- Stagnation (lactostasis in lactating women) - a violation of the outflow of milk creates a favorable environment for the development of bacteria. Reason: inept pumping of milk, improper attachment of the baby to the breast, tight bra, tight clothing, severe lack of physical activity.
- Various pathologies of the mammary glands (fibrocystic mastopathy, complications after plastic surgery, etc.).
Common provoking factors include poor ecology, stress, sudden climate change, and failure to comply with hygiene rules. In nulliparous women, the cause of the pathology can be unsuccessful piercing and too active sexual games with injury to the nipples.