Fenistil is a children's drop that has an antihistamine effect. This remedy is usually prescribed by doctors for allergic reactions in children. The popularity of the drug is due to the fact that it can be given almost from the first days of a baby’s life. The result of use can be observed within 15 minutes. It has a dispenser that allows you to measure the required dose. The drops have a pleasant taste and can be given undiluted.
Indications for use
The product for internal use is indicated in the following cases:
- allergies (urticaria, year-round allergic runny nose, allergic reaction to medications and food);
- itching of the skin caused by eczema, rubella, dermatoses, insect bites;
- for preventive purposes.
The drug in the form of an emulsion and gel is used for:
- itchy skin;
- various burns.
Despite the fact that the medicine can be bought without a prescription from a specialist, it should only be used as prescribed by a doctor.
Prevention
Atopy is translated from Latin as strangeness. The causes of the disease cannot always be determined. But long-term observation of patients and members of their families has revealed that it develops more often:
- with a genetic predisposition - if the parents are healthy, the probability of developing dermatitis in the child is 20%, if one of them is sick - 50%, if both are sick - 80%;
- in case of unfavorable pregnancy, active or passive smoking of the expectant mother, consumption of food that provokes allergy attacks, use of certain medications;
- when a newborn is in a dusty room, insufficient care for his personal hygiene;
- with prolonged exposure to allergens that enter the child’s body with food through the respiratory tract.
Breastfeeding for up to 6 months and avoiding allergy-provoking foods reduces the likelihood of developing atopic dermatitis.
Contraindications and negative reactions
The drug in any form is contraindicated for the following conditions and problems:
- bronchial asthma;
- babies up to 1 month;
- in the first trimester of pregnancy;
- during breastfeeding;
- hypersensitivity to the constituent components.
Can be used with caution in chronic obstructive bronchial diseases.
After using the product, undesirable effects may occur:
- from the central nervous system: lethargy, dizziness, headache, drowsiness;
- from the gastrointestinal tract: nausea, vomiting;
- from the respiratory system: problems with external respiration;
- other reactions: skin irritation, muscle spasms.
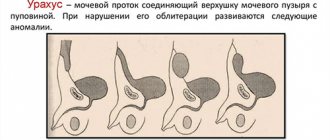
Overdose
Possible overdose of the drug. Manifested by dry mouth, urinary retention, arterial hypotension. An adult may experience symptoms of central nervous system depression, lethargy and drowsiness. On the contrary, the child shows signs of excitation of the central nervous system. Convulsions and hallucinations are possible.
There is no specific antidote. The therapy aims to support the functioning of the respiratory system, heart and blood vessels.
In case of overdose, you should take activated charcoal or a laxative in the form of a saline solution.
How to take Fenistil
Drops are intended for oral use. Children over 12 years of age and adults can be given up to 120 drops per day (40 drops per dose). Infants are given up to 10 drops 3 times a day. From 1 year to 12 years – up to 15 drops 3 times a day.
Gel. Designed for outdoor use. Can be applied to problem areas of the skin no more than 4 times a day. Avoid exposure to direct sunlight. If allergies are pronounced, you should additionally use drops.
Emulsion. Intended for local application. You can treat the affected skin up to 4 times a day.
Pills. Do not give to children under 12 years of age. It is prescribed to take 1 tablet per day, since the duration of action of the active substance is 24 hours. It is best to take the tablet before bed to avoid daytime sleepiness. The tablet should be swallowed whole with plenty of water. The course of treatment lasts up to 25 days.
Poisoning in children
All over the world, the number of acute poisonings is steadily increasing, this situation is called a “creeping disaster.” Due to the wide distribution of various chemical and pharmacological drugs in the environment, more and more children are admitted to toxicology departments with a diagnosis of acute exogenous poisoning.
Another, even more serious, reason is the mother’s frivolous attitude towards the health of her own child, her inattention and reliance on the Russian “maybe”.
The one-year-old baby woke up early and climbed out of the crib. Mom dressed him and let him “free-graze”, and she went to bed to get some sleep.
You say: this can’t happen? Unfortunately, it can, like all other cases from personal medical practice.
The kid, left unattended, happily ran the kitchen, scattered cereal, spilled oil, and then climbed onto a chair and took out his grandmother’s clonidine from the shelf. An hour later, when the mother woke up, the baby was already asleep, clutching a bottle of pills in his fist.
A friend came to visit her mother, whom she had not seen for a long time. There is so much news that requires immediate discussion over a cup of coffee and a cigarette. But passive smoking is harmful to children. Therefore, they left him in the room, and they retired to the kitchen. It is unknown how long the smoke break lasted. Mom claims that it won’t be long. But the baby had enough time to take birth control pills out of the guest’s bag and feast on them.
A two-year-old girl was playing on the floor with toys and suddenly fell asleep on the floor. Mom carried her to the crib and went about her household chores, happy that the child was not in the way. After some time, the mother noticed that the girl’s sleep was restless, she was crying without waking up, making random movements with her limbs, as if fighting off someone.
The emergency doctor suspected drug poisoning, and a bottle of amitriptyline (used for depression) was found on the floor among the toys. The child's restless behavior was explained by the occurrence of hallucinations.
Mom poured “Antinakipin” into the kettle and left it overnight so that all the sediment dissolved. When early in the morning the baby demanded a legitimate bottle, the half-asleep mother diluted the milk formula with water from the ill-fated kettle and gave it to the child. She came to her senses only after noticing that the mixture in the bottle had curled up into flakes. And during this time the baby had already taken a sip of a hefty dose.
Thousands of similar examples can be given.
But there are other cases when the mother exceeds the dose of the medicine with her own hands or mistakenly gives the child another medicine.
Every family has a first aid kit with a set of the most necessary and seemingly harmless medicines. But are they so harmless?
Back in the XYI century, the physician and naturalist Paracelsus said: “Only the dose distinguishes poison from medicine.”
Do you know that Calpol, Panadol, Tylenol and other paracetamol-based drugs, widely advertised and loved by parents, have a toxic effect on the liver even in a dose only twice as high as a single dose, and a tenfold excess of a single dose causes kidney failure? Isn't the penalty for uncontrolled consumption of “strawberry-flavored syrup” too heavy?
The familiar drugs diphenhydramine, suprastin, pipolfen, in addition to allergic ones, have a calming and hypnotic effect, which makes them very popular with some parents.
Wanting the child to sleep longer on a weekend or holiday, the mother gives the baby diphenhydramine in an increased dose.
Contrary to the expected result, the child does not fall asleep and receives another tablet. After this, the child not only does not calm down, but, on the contrary, becomes agitated, does not find a place for himself in the crib, fights off someone invisible with his hands, squirms, and cries. His skin turned red and dry, his pupils dilated, his heart beat faster. And the culprit was an overdose of diphenhydramine.
The baby has a runny nose. He cannot breastfeed and sleeps poorly. The doctor prescribed vasoconstrictor nasal drops for the baby: naphthyzin, galazolin or sanorin. After the first procedure, the baby breathed freely through his nose, ate well and fell asleep peacefully. The satisfied mother began to instill drops in him before each feeding, and then again before putting him to bed. By evening, the child seemed to have been replaced: he became lethargic, drowsy, refused to eat and asked to go to bed. The skin became pale, cold, and sweating increased. Having measured the temperature, the mother was horrified: 34.7 C. So intensive treatment of a runny nose led to poisoning of the baby.
Increasingly, vasoconstrictor drops are produced in plastic bottles equipped with a dropper spout. This is done for the convenience of consumers: remove the cap, press on the pliable walls, drop the medicine into the nose, and no fuss with the pipette. This method is not suitable for small children, since by applying force, you can inject the medicine in a stream, significantly exceeding the dose. Use a regular pipette, putting in as many drops as the doctor prescribed.
The child vomits repeatedly, and the mother, instead of inviting a doctor, gives him cerucal for two days in a row (“I know that it stops the vomiting”). And she has no idea about the side effects of this drug, as well as the undesirability of its use in children under 14 years of age. Therefore, when on the 3rd day the child began to experience violent movements in the limbs and neck muscles (hyperextension of the arms, involuntary turns of the head to the side) and convulsive twitching (grimaces) of the facial muscles, the mother was very surprised and called an ambulance. Having barely looked at the boy, the emergency doctor asked: “Did you give Cerucal?”, and, having received an affirmative answer, began to lavage the stomach through a tube.
Unfortunately, poisoning in children is not limited to drugs. In everyday life, we are surrounded by chemicals designed to improve and make our lives easier. How many troubles and misfortunes the vinegar essence, used in every family for home canning, has brought and will continue to bring to children! No country in the world produces acetic acid of such concentration for household purposes, but here, please drink, I don’t want it.
Neither a pedantic German woman, nor a frivolous French woman, nor a disciplined American woman would think of pouring a toxic substance into a Pepsi or Fanta bottle, and in our country, the cause of poisoning of children is often the neglect of the basic rules for storing detergents and disinfectants and household chemicals.
“How did this happen? - Mom laments, “after all, I wrote on the bottle that there is gasoline.”
But the baby doesn’t know how to read, but he remembers well that yesterday, during a walk, dad poured him some delicious water from such a bottle.
In children under one year of age, motor activity and field of activity are limited to a crib or playpen. They cannot obtain and swallow medications or toxic substances on their own. Therefore, the cause of poisoning in children in the first year of life is the inattention and carelessness of parents, when, having mixed up the dishes, they give the child alcoholic drinks or other toxic substances instead of water; instead of nasal drops, eye drops with clonidine are instilled; following doctor's prescriptions, they exceed the dose of medications, and often treat the child on their own, without consulting a doctor, relying on their own knowledge or the advice of friends.
The baby’s ability to move independently increases the risk of accidents, including poisoning. There are fewer and fewer inaccessible places for a child, and more and more attractive-looking objects and substances. Is it possible to pass by a bottle with such beautiful multi-colored tablets? You need to get them out and try them immediately. Oh, and they are also in a sweet shell, real candies!
Always remember that a child “learns the world through his mouth.” This circumstance explains the largest number of poisonings in the group of children 2 and 3 years of age.
Add here the mother’s carelessness in everyday life, the carelessness of adults when storing medicines and chemicals, and the picture will be complete.
The fate of a child with acute poisoning often depends on the correct behavior of the mother or others. What should a mother do if her child has taken a drug or chemical?
If the fact of ingestion of a toxic substance is established, immediately call an ambulance, and before the brigade arrives, free the child’s mouth from tablets that he did not have time to swallow, try to rinse his mouth and give him a large amount of water (up to 200 ml) with two crushed tablets of activated carbon or other adsorbent, for example, polyphepan (1-2 teaspoons).
Do not give milk to your child, as some poisons are fat-soluble, and the fat contained in milk will speed up the absorption of the poison.
Try to collect and count the remaining tablets, estimate how many tablets the baby managed to swallow. It is clear to everyone that the larger the dose, the more severe the poisoning, the more serious the prognosis.
But you shouldn’t calm down if you’re missing “just one” tablet. Some medications have such a strong and rapid effect that even one tablet can lead to severe impairment of vital functions. Such drugs include nitroglycerin, chlorpromazine, digoxin, gemiton, clonidine, amitriptyline.
Never induce vomiting in a child if poisoning occurs with concentrated acid or caustic alkali, which causes burns to the mouth, pharynx and esophagus. A caustic substance, when passing in the opposite direction, will inevitably increase the area and depth of the burn, and may also enter the respiratory tract. Try to give your child water (1.5 - 2 glasses) to reduce the concentration of the caustic substance in the stomach.
The popular opinion that in case of acid poisoning one should drink alkaline drinks, and in case of alkali poisoning - weakly acidic solutions, is incorrect, since the carbon dioxide formed as a result of such a reaction causes overdistension of the stomach and deterioration of the child’s condition.
If poisoning occurs due to gas or fumes of a toxic substance, the child should be urgently removed from the gas-polluted room, freed from restrictive clothing, and cleared of mucus and vomit from the airways.
If a toxic substance gets into the eyes, it is necessary to rinse the eyes with a stream of warm water using a syringe (without a needle) or a rubber bulb for 5 minutes.
If a toxic substance gets on the skin, the child should be undressed and the skin should be thoroughly washed with warm running water and soap, first treating the contaminated areas and then the entire surface of the body.
Sometimes the fact that a child is taking medications or chemicals remains unknown to the mother or other adult family members, which significantly complicates diagnosis, leads to untimely provision of assistance, and worsens the prognosis.
An alarming moment that makes a mother think about poisoning is a change in the child’s behavior: usually active and cheerful, he suddenly becomes lethargic, drowsy, and falls asleep at inopportune times. The sleep is so deep and sound that it is impossible to wake him up. Or, conversely, in a dream, a child makes active movements, crawls on the bed, fights off someone with his arms and legs, cries, screams, without waking up. This behavior indicates hallucinations. Convulsions and loss of consciousness may occur.
Consider poisoning if...
- your baby has a runny nose, and you, sparing no medication, instill vasoconstrictor drops into his nose, and the child becomes lethargic, refuses to eat and asks to sleep;
- the child suddenly becomes silly, funny for no reason, he is “stormy”, i.e. staggers to the sides when walking, he bumps into objects, stumbles out of the blue;
- in the midst of complete health, the child’s condition suddenly worsens, consciousness is impaired, convulsions appear, and there are no signs of an acute inflammatory disease.
Call an ambulance and tell your doctor about your observations and suspicions. The sooner you do this, the better for the child.
Is there really nothing that can be done to protect children from exposure to toxic substances? It is possible and even necessary!
Prevention of poisoning is extremely simple and does not require any moral or material costs from parents.
Medicines should be stored out of the reach of children. Periodically audit your home medicine cabinet and get rid of unnecessary, expired, or worn-out medications. Do not keep medications “on hand” in your cosmetic bag, pocket, or purse. Your young explorer will find them everywhere and try them out.
If you give your child pills or vitamins during illness, never call them “candy.”
Store cleaning agents and detergents, insect repellent aerosols, stain removers and solvents, and technical fluids indoors or in a locked cabinet.
Pouring potentially toxic substances into food containers is not permitted.
Nail polish remover, deodorants, and cosmetic lotions should be stored on a high shelf where a child cannot reach even from a chair.
Do not leave unfinished alcoholic drinks in glasses. While you are seeing off the guests, the children can continue the festive feast, following your example.
Do not keep poisonous plants in the house, and on a walk do not allow your child to try the “beautiful berries” from trees and bushes.
All of the above applies to a greater extent to children, whose poisoning is mainly accidental.
Fenistil Pentsivir for the treatment of herpes on the lips
Herpes is a disease that can appear in men and women regardless of age. A cold can get worse at any time if your immune system is weakened. Herpes usually appears in autumn and winter. Most often, the disease manifests itself on the lips, but there are also cases of herpes in the mouth and nose.
The drug Fenistil will help get rid of the rash faster and speed up the healing process. The product begins to act from the first minutes after application. Symptoms of the disease disappear within 3-5 days. Before use, you must read the instructions.
special instructions
If Fenistil is prescribed for infants, then the drops should be added to a bottle with warm food before feeding. The drops taste good, so children happily take them. You should strictly adhere to the prescribed dose, otherwise there is a possibility of adverse reactions.
Since absent-mindedness and weakness may occur after taking the drug, you should be careful when driving a vehicle or other machinery.
You should avoid taking it together with antihistamines and procarbazine.
Symptoms
The main and most obvious symptom of the pathology is a rash. Most often, rashes appear on the head, chest, back, groin, armpits, and buttocks. The rash appears as scattered blisters with clear, white or yellow contents, or as small grains with an inflammatory outline.
During the day, the rash may intensify or decrease, and the severity of its manifestation depends on changes in temperature and care for the baby’s skin. In some cases, the child does not show concern, but sometimes may experience itching, pain and demonstrate discomfort with whims, unstable sleep, and lack of appetite.
In mild forms of the disease, other symptoms may not occur. But in more advanced cases, which are accompanied by complications and infection, clinical manifestations may be supplemented by:
- elevated temperature up to 38 degrees;
- the appearance of light plaque, ulcers, ulcers;
- the formation of weeping cracks with an unpleasant odor;
- general deterioration of condition.
When assessing symptoms, it is important to prevent the development of advanced forms of prickly heat and consult a doctor promptly, without waiting for complications to develop. Source: Skin care for a newborn. Solntseva O.A. Medical Council, 2014. p. 35-39.