- Home /
- Branches /
- Ophthalmology /
- Dacryoadenitis
11/03/2021 The article was checked by ophthalmologist A.A. Nazyrov. , is for general informational purposes only and does not replace specialist advice.
For recommendations on diagnosis and treatment, consultation with a doctor is necessary. Dacryoadenitis is inflammation of the lacrimal gland. This is usually a one-way process. There are acute and chronic dacryoadenitis.
Causes
When dacryoadenitis develops, the causes of this condition are varied. Conventionally, ophthalmologists divide them into 2 groups:
- Infectious;
- Non-infectious.
Infectious dacryoadenitis in children and adults is caused by the following groups of pathogens:
- Viruses:
- Herpes;
- Infectious mononucleosis;
- Corey;
- Flu, etc.
- Bacteria:
- Staphylococcus;
- Pneumococci;
- Streptococci;
- Mycobacterium leprosy and tuberculosis;
- Gonococci.
- Mushrooms.
- Parasites.
Non-infectious dacryoadenitis in children and adults is causally associated with 2 factors:
- Systemic pathologies (sarcoidosis, blood and lymph diseases);
- Pseudotumors of the lacrimal gland, which are of an autoimmune nature (glandular tissue is damaged by its own immune cells).
Symptoms of dacryoadenitis
Acute dacryoadenitis is manifested by the following symptoms:
- Soreness and redness of the skin over the lacrimal gland. It is located above the upper eyelid at the outer corner of the eye.
- Swelling and drooping of the upper eyelid, which occurs as a result of an increase in the size of the gland.
Chronic dacryoadenitis has slightly different symptoms:
- Double vision;
- Shift of the eye to the side;
- Swelling over the upper eyelid (redness, as a rule, is absent; it can appear only during an exacerbation).
Long-term chronic dacryodenitis changes the symptoms of inflammation to the symptoms of a lacrimal gland cyst, which gradually forms:
- Discomfort and feeling of pressure;
- Impaired tear formation.
Prevention
Considering that in most cases these diseases are caused by bacterial flora, the main method of prevention is:
- Maintain personal hygiene, first of all, clean hands, through which infectious agents are introduced into the eyes. Following this rule will protect adults and children from bacterial conjunctivitis and blepharitis, which cause inflammatory diseases of the lacrimal apparatus.
- Compliance with occupational hygiene at work - wearing protective glasses in conditions of increased gas and dust. Wearing safety glasses is also necessary when performing gardening work (treating plants with insecticides and fungicides), since chemicals often cause irritation of the conjunctiva, which becomes a breeding ground for bacterial inflammation.
- When inflammatory processes appear in the eye, timely treatment is important to prevent complications from the lacrimal apparatus.
- Sanitation of existing foci of infection in nearby organs (nose, paranasal sinuses, nasopharynx).
Complications
If treatment is not carried out, the risk of infectious complications increases:
- Abscess of the upper eyelid;
- Orbital phlegmon.
Symptoms of an abscess are as follows:
- Severe bursting pain;
- Headache;
- Severe swelling and redness of the eyelid, which causes it to close (narrow eye);
- Skin tension and redness, but in some cases it may become jaundiced;
- Zone of fluctuation (softening) in the area of the upper eyelid (its appearance is associated with purulent melting of subcutaneous fat);
- Body temperature rises, but visual functions do not decrease.
Orbital phlegmon is a more dangerous complication and is manifested by other signs:
- Rapid development in a couple of hours;
- Intense pain in the eye;
- Red-violet widespread swelling of the eyelids;
- Pronounced narrowing of the eyelids;
- Infringement of the conjunctival membrane in a sharply narrowed palpebral fissure;
- Double vision and severe decreased vision (a person may go blind);
- Almost complete immobility of the eyeball;
- Intense headache;
- Fever and chills.
Clinical observation
Patient B., born in 1986 (34 years old), resident of the Sverdlovsk region. I went to the clinic of UNIIF, a branch of the Federal State Budgetary Institution "NMITs FPI" of the Ministry of Health of Russia on December 12, 2019.
Complaints at the time of treatment: double vision, which intensified when looking up, to the left and when working close, decreased visual acuity of the left eye, narrowing of the palpebral fissure, drooping of the upper eyelid on the left.
Medical history: the presence of chronic diseases, tuberculosis, denies contact with tuberculosis patients. According to the results of the examination, viral hepatitis, HIV infection, and sexually transmitted diseases were not detected. Doesn't smoke, doesn't take drugs, doesn't abuse alcohol. Fluorography in 2021 - without pathology.
OU - high myopia since school age, scleroplasty was performed in 1995, complete vision correction (OD with sph -14.0 diopters, OS with sph -9.0 diopters), and the patient saw better with the left eye.
For the first time in March 2021, the patient noticed double vision and decreased vision predominantly in the left eye, narrowing of the palpebral fissure, drooping of the upper eyelid on the left with a gradual deterioration in the condition of the eyes. I contacted an ophthalmologist at my place of residence. In May 2021, he was consulted at the State Autonomous Institution of Social Institution "Social Clinical Clinical Hospital No. 1", diagnosis: "High myopia of both eyes, suspicion of a neoplasm of the orbit on the left." Recommended: MRI of the orbits, consultation with a hematologist. According to MRI of the brain, the orbital conclusion: pseudotumor of the orbit? left. Consultation with a hematologist on June 10, 2019, diagnosis: “Diffuse non-Hodgkin’s lymphoma, unspecified, neoplasm of the left orbit of unknown origin.” Sent for positron emission tomography and CT on July 12, 2019, the results of which revealed changes in the lower lobe of the left lung, subpleurally - two compactions with increased metabolic activity, adenopathy of the intrathoracic lymph nodes of all groups up to 24–19 mm.
In August 2021, the patient noticed a lump in the area of the right collarbone. On November 5, 2019, a biopsy of the right subclavian lymph node was performed at the oncology clinic. Conclusion: granulomatous lymphadenitis. The morphological picture is most consistent with sarcoidosis in the granulomatous-sclerotic phase. For a reliable diagnosis, clinical and laboratory exclusion of tuberculosis is necessary.
Fluorography dated November 28, 2019 - diffuse changes in both lungs like small-focal dissemination. Diffuse strengthening and deformation of the pulmonary pattern according to the mesh type.
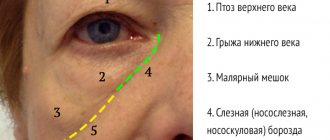
The general condition of the patient at the time of treatment on December 12, 2019 was satisfactory. Ophthalmological status: Vis OD=0.1 with sph -14.0 diopters=0.8; Vis OS=0.1 s sph -10.0 D=0.5; IOP OU=18 mm Hg. Art. (according to Maklakov). Visual fields and color perception are within normal limits. OD - correct position, full mobility. OS - downward displacement of the eyeball, limitation of its mobility in all directions and increased diplopia during abduction. Narrowing of the palpebral fissure on the left, ptosis (Fig. 1 A). Increased size of the lacrimal gland on the left (Fig. 1 B). Biomicroscopy and examination of the fundus of both eyes revealed no signs of an inflammatory process (uveitis).
Optical coherence tomography (OCT) and photofixation (iVue-100 v3.2, Optovue, USA) were performed. OCT data revealed a thickening of the layer of nerve fibers in the peripapillary region and thinning of the retina in the macular zone of the right eye, which was due to the presence of high myopia in both eyes.
With a preliminary diagnosis of “Unspecified interstitial pulmonary disease (sarcoidosis? tuberculosis?). Suspicion of sarcoidosis of the orbit, lacrimal gland on the left,” the patient was hospitalized in the differential diagnostics department of the UNIIF, a branch of the Federal State Budgetary Institution “National Medical Research Center for Physical Pedigrees” of the Ministry of Health of Russia, where he was from December 16, 2019 to February 28, 2020.
Examination data: CT scan of the chest dated December 16, 2019 - focal dissemination throughout all pulmonary fields on both sides. Adenopathy of the upper central mediastinum. Dynamics: from July 12, 2019 to December 16, 2019, according to PET and CT data, an increase in the pulmonary component. Conclusion: disseminated lung disease, progressive course. Adenopathy of the intrathoracic lymph nodes (Fig. 2 A, B).
MRI of the brain, orbit 12/24/2019 - in the area of the thickened tendon of the superior rectus muscle on the left, an area with a hypo-isointense signal is visualized, the soft tissues of the eyelid, the areas around the lacrimal gland are thickened, the signal is not changed. No pathology of the optic nerves was noted. Conclusion: suspicion of myositic pseudotumor of the left orbit (Fig. 3 A).
On December 19, 2019, fiberoptic bronchoscopy with trans-bronchial lung biopsy and forceps biopsy of the bronchus was performed. Histological conclusion: epithelioid cell granulomatous lesion of respiratory tissue with necrosis in the center of one of the granulomas. First of all, it is necessary to differentiate between productive tuberculosis and sarcoidosis with a necrotic tissue reaction. Microscopy of bronchial lavage water using the Ziehl-Neelsen method from 12/19/2019, 12/20/2019, 12/23/2019 - no acid-fast mycobacteria were detected.
Intradermal test with tuberculosis allergen dated December 20, 2019 - negative result.
Clinical blood tests and general urine analysis are within normal limits.
Consultation with a neurologist 01/13/2020 - no pathology was detected.
Taking into account the clinical picture and examination data, a clinical diagnosis of “Multiorgan sarcoidosis” was established: sarcoidosis of the lungs, intrathoracic and peripheral lymph nodes, orbit, and lacrimal gland on the left.
The patient was prescribed treatment: aminophylline 2.4% 5.0 ml, dexamethasone 8 mg, NaCl 0.9% 200 ml intravenous drip No. 5. High-protein diet. Start of systemic therapy with GCS on December 26, 2019 - methylprednisolone 28 mg/day, from February 10, 2020 - 27 mg/day, then reduce the dose by 1 mg every 10 days until complete withdrawal.
On CT on February 25, 2020 (Fig. 2 C, D), in comparison with the data from December 16, 2019, there is an almost complete regression of small elements of diffuse lung damage evenly in all sections, as well as a decrease and normalization of the size of the lymph nodes of the paratracheal groups and the aortopulmonary and bifurcation groups.
As a result of therapy for 2 months. Significant positive clinical and radiological dynamics in the patient’s condition were noted. During the control MRI of the brain and orbits dated 02/06/2020 (Fig. 3 B), in comparison with the MRI dated 12/23/2019, normalization of the thickness of the tendon of the superior rectus muscle on the left is noted; soft tissues of the eyelid, the areas around the lacrimal gland are comparable in intensity to the opposite side, some thickening of the upper eyelid remains.
Ophthalmological status 02/26/2020: the patient notes improvement in vision, but discomfort and double vision persist when working near. Vis OD=0.1 s shp -14.0 D=0.9 Vis OS=0.1 s shp -9.0 D=0.9; IOP OU=19 mm Hg. Art. (according to Maklakov). Visual fields and color perception are within normal limits. Both eyes are calm, a slight narrowing of the palpebral fissure on the left remains. The left eyeball is in the correct position, with almost full range of motion, with slight restriction in downward gaze (Fig. 1 C). The left lacrimal gland has decreased in volume, its size and position correspond to the right one. Otherwise, the ophthalmological status and OCT data correspond to the indicators on December 12, 2019.
Final clinical diagnosis
: sarcoidosis of the lungs with sarcoidosis of the lymph nodes, acute course, phase of drug regression. Sarcoidosis of the orbit, dacryoadenitis on the left, phase of drug regression. High myopia in both eyes. Respiratory failure 0.
Recommendations for discharge: observation by a pulmonologist/therapist, ophthalmologist at the place of residence. Continue treatment of sarcoidosis with methylprednisolone - the course of treatment began on December 25, 2019 with 28 mg/day, from February 10, 2020, reduce the daily dose of methylprednisolone by 1 mg, once every 10 days, continue reducing the daily dose until complete cancellation.
The presented clinical observation demonstrates the development of multiple organ damage in sarcoidosis with initial complaints of impaired visual function and pathological changes in the left orbit. Sarcoidosis was suspected only after a biopsy and histological examination of an enlarged subclavian lymph node, although focal changes in the lungs and adenopathy of the intrathoracic lymph nodes, according to chest CT, had already occurred at an earlier stage of the process. Thus, verification of the diagnosis and start of systemic therapy for the disease occurred only after 10 months. from the moment the patient complains.
Modern diagnostics at NEARMEDIC
Acute or chronic dacryoadenitis is an indication for additional diagnostics. It allows you to clarify the cause of the disease, the presence of complications and the neglect of the process. All this data is necessary for adequate and successful treatment. That is why the issue of high-quality diagnostics is given special attention at the NEARMEDIC center. Our specialists:
- They work on modern diagnostic equipment, which makes it possible to identify even minimal deviations in the anatomy of the eyeball;
- They constantly improve their knowledge at international symposia and congresses, so they are aware of the latest achievements in ophthalmology;
- They answer all the patients’ questions so that the person understands why this or that examination is being carried out and how it will help solve the health problem.
The main diagnostic procedures that NEARMEDIC ophthalmologists recommend for suspected dacryoadenitis are:
- Visometry – determination of visual acuity. Sometimes its decrease and the fact of doubling are revealed when examining letters;
- Biomicroscopic examination - examination under magnification of the conjunctiva and other superficial structures of the eye. When the lacrimal gland is inflamed, doctors see redness and dilation of blood vessels, an enlargement of part of the lacrimal gland;
- Refractometry - the study of the refractive abilities of the eye;
- Perimetry – determination of visual fields;
- Ophthalmoscopy – examination of the fundus of the eye;
- Tonometry - measuring the pressure inside the eye, which is often elevated;
- Rinsing the lacrimal ducts to assess their patency;
- Ultrasound scanning of the eyeball, supplemented by Dopplerography (assessment of blood flow). It reveals the exact localization of the inflammatory process.
To clarify the nature of the disease, the following diagnostic tests are indicated:
- Bacterial culture of conjunctival contents to determine the causative bacteria and the degree of their sensitivity to modern antibiotics;
- C-reactive protein, rheumatoid factor, which change in autoimmune pathology;
- Detection of chlamydial antibodies;
- Computed or magnetic resonance imaging of the orbital region.
At NEARMEDIC, doctors individually approach each clinical case, so they do not prescribe uninformative tests - only what you need to provide effective assistance.
Sometimes consultation with related specialists (ENT, cardiologist, dentist, etc.) may be required. Only in our multidisciplinary center you will undergo it quickly and efficiently, without leaving the institution. We save your time!
Introduction
Sarcoidosis was first described by J. Hutchinson in 1877 as a skin disease.
In the second half of the 20th century. observation and treatment of patients with sarcoidosis was carried out by specialists from the phthisiology service, taking into account the similarity of the clinical picture of bronchopulmonary lesions with tuberculosis. According to modern concepts, sarcoidosis is a systemic inflammatory disease of unknown etiology, characterized by the formation of non-caseating granulomas, multisystem damage to various organs and activation of T cells at the site of granulomatous inflammation with the release of various chemokines and cytokines, including tumor necrosis factor α [1]. Sarcoidosis occurs in patients of different age groups, has a tendency to spontaneous remissions and relapses after treatment, and requires adequate therapy [1–3]. The progressive course of the disease according to X-ray monitoring and functional testing of breathing, extrapulmonary manifestations, including damage to the organ of vision with the threat of decreased visual functions, affecting the patient’s quality of life, determine the prescription of glucocorticosteroids (GCS) systemically as first-line drugs in the treatment of sarcoidosis [1, 3, 4].
The development of pathology of the organ of vision in patients with sarcoidosis is possible both before the manifestation of signs of systemic damage and during the course of the disease and varies, according to the literature, from 15% to 80% of cases [5, 6]. In the structure of ophthalmological pathology in sarcoidosis, uveitis undoubtedly leads, accounting for up to 30–77.8% of all identified localizations [6–8]. Involvement of the anterior part of the choroid is observed more often - in 52.5–75% of cases [5, 6], posterior uveitis - in 25.3–31.3% [5], it is more typical for patients in the older age group [6] .
Lesions of the orbit and adnexal apparatus of the eyes in sarcoidosis are somewhat less common, but also quite varied. The most commonly detected pseudotumor of the orbit involves the lacrimal gland, accounting for 27.7% of cases among patients with ocular sarcoidosis and 63% of cases among patients with orbital sarcoidosis [8, 9]. At the same time, the development of isolated dacryoadenitis is described in 14.8% and 55% of cases, respectively [8, 10]. The presence of granulomatous inflammation in the orbit without involvement of the lacrimal gland is somewhat less common - in 13–20% of cases, according to various authors [9, 10]. In addition, isolated cases of damage to the optic nerve in its retrobulbar region, as well as extraocular muscles [10], eyelids and lacrimal sac [9], have been described.
The manifestation of systemic manifestations of sarcoidosis by pathological changes in the organ of vision occurs in a fairly large number of cases - from 38% to 80% [8, 9].
At the same time, in patients with orbital sarcoidosis, further examination reveals other localizations of the disease in half of the cases [10]. According to the results of computed tomography (CT) of the chest, in the absence of clinical symptoms, lesions of the lungs and intrathoracic lymph nodes of varying severity, characteristic of sarcoidosis, were found in 10% of patients with granulomatous uveitis [11] and in almost all patients with orbital sarcoidosis [ 12–14].
The presence of space-occupying formations in the orbit requires a full examination in order to exclude the systemic nature of the process [5]. Ophthalmologists need to remember a multidisciplinary approach to the examination and treatment of this group of patients, involving specialists from different fields, depending on the identified pathological changes.
The article describes a clinical observation of a patient with multiple organ sarcoidosis and the onset of clinical manifestations of the disease in the form of visual impairment and pathological changes in the left orbit. It is presented to draw the attention of ophthalmologists to the importance of a multidisciplinary approach to the examination and treatment of patients with orbital pathology.