Lymphogranulomatosis is a malignant neoplasm of the lymphatic system, the distinctive feature of which is the presence in the lymph nodes affected by the tumor of special giant cells derived from B lymphocytes, which are called Berezovsky-Sternberg-Reed cells.
- Causes of lymphogranulomatosis
- Classification of lymphogranulomatosis
- Symptoms of lymphogranulomatosis
- Diagnosis of lymphogranulomatosis
- Treatment of lymphogranulomatosis
- Prognosis for lymphogranulomatosis
The disease is characterized by damage to the lymph nodes, which occurs unicentrically in one group of lymph nodes (usually the supraclavicular, cervical and mediastinal lymph nodes), and spreads from one group to another. Gradually, internal organs and bone marrow are involved in the process.
Epidemiologists identify two peaks of incidence. One is for ages 15-35, and the other is for people over 50 years of age. The disease progresses more favorably in young people due to the absence of concomitant severe pathologies and greater opportunities in the treatment methods used.
Causes of lymphogranulomatosis
The causes of the development of lymphogranulomatosis continue to be investigated. Three main reasons are considered:
- Viral diseases, in particular the Epstein-Barr virus, which causes mononucleosis. This theory is supported by the fact that in approximately 20% of cases, the genetic material of this pathogen is isolated in the tumor biopsy. There is also some correlation with HIV, which leads to disruption of the immune system.
- Immunodeficiency states. There are a number of studies that indicate that lymphogranulomatosis develops against the background of T-cell immunodeficiency. This factor is supported by a violation of the ratio of T-helpers and T-suppressors.
- Hereditary predisposition. This theory is supported by family cases of lymphogranulomatosis and the discovery of characteristic genetic markers of this pathology. It is assumed that maternal lymphocytes can penetrate the placental barrier, causing immunopathological reactions in the fetus. The disease can also develop as a result of specific mutations, which can be provoked by drugs, ionizing radiation and other factors.
Classification of lymphogranulomatosis
There are 2 types of lymphogranulomatosis:
- Classic Hodgkin's lymphoma.
- Nodular Hodgkin's lymphoma with lymphoid predominance.
Classic Hodgkin lymphoma includes several histological variants of the tumor, but they are all characterized by a single immunophenotype. Tumor cells express CD 30, CD 15, PAX 5. In some cases, CD 20 expression may be noted (this is necessarily noted when describing the molecular genetic profile of the tumor, since these data affect treatment). Expression of CD 45 and CD 3 is not typical.
Nodular lymphoma differs from classic lymphogranulomatosis both clinically and immunomorphologically. Tumor cells intensely express CD 20 and CD 45. CD 30 and CD 15 are not detected.
Depending on the extent of tumor spread, there are 4 stages of lymphogranulomatosis:
- 1 local stage - either one group of lymph nodes or one internal organ is affected.
- Regional stage 2 - more than one group of lymph nodes is affected, but on one side of the diaphragm. Or there is damage to one internal organ, with regional lymph nodes involved in the process.
- Generalized stage 3 - groups of lymph nodes on both sides of the diaphragm are affected; the spleen or other internal organs may be involved in the process.
- Stage 4 disseminated - internal organs (lungs, kidneys, etc.) are involved in the process
What types of lymphomas are there?
Primary lymphomas are usually divided into two large groups:
- Hodgkin's lymphomas/lymphogranulomatosis (Hodgkin's disease, Hodgkin's lymphomas),
- Non-Hodgkin's lymphomas (lymphosarcoma, NHL).
According to the National Medical Research Center of Oncology named after. N.N. Blokhin, in Russia the incidence of non-Hodgkin's lymphomas is 1.5-3 times higher than the incidence of lymphogranulomatosis.
The difference between these lymphomas becomes clear after morphological examination of a tissue sample (biopsy). In Hodgkin's disease, large mutated Berezovsky-Sternberg-Reed cells are found in the affected lymph nodes. Hodgkin's lymphomas have a more aggressive course with pronounced symptoms, but they are easily treatable.
Lymph nodes affected by Hodgkin's disease are most often located above the collarbones, in the neck, armpits, and mediastinum.
In addition to B-lymphocytes, non-Hodgkin's lymphomas also affect T-lymphocytes. The disease usually occurs without significant symptoms and is difficult to treat. But first you need to correctly determine the type of non-Hodgkin lymphoma - the current classification consists of 30 names, including:
- chronic lymphocytic leukemia;
- T-cell leukemia;
- follicular lymphoma;
- diffuse large B-cell lymphoma;
- mycosis fungoides Sézari et al.
Symptoms of lymphogranulomatosis
In the initial stages, lymphogranulomatosis can manifest itself as enlarged lymph nodes. They usually do not hurt, are mobile during palpation, are not fused with the surrounding tissues, and can stretch in the form of a chain. Patients can detect external lymph nodes themselves. And an increase in internal ones is manifested by disruption of the functioning of nearby organs. For example, with enlargement of the mediastinal lymph nodes, shortness of breath, dry cough, difficulty swallowing, and swelling of the upper half of the body may occur. If enlarged lymph nodes are located in the abdominal cavity, abdominal pain and swelling of the legs may occur.
When internal organs and bones are involved in the process, the following problems may arise:
- Pneumonia and pleurisy.
- Pain in bones with pathological fractures.
- Intestinal bleeding, perforation of the wall of the gastrointestinal tract with the development of peritonitis.
- When the bone marrow is involved in the process, anemia, bleeding and decreased immunity are noted.
Systemic manifestations include fever, night sweats and weight loss. Temperature increases are periodic and can produce peaks of up to 39 degrees. These signs are called B-symptoms and their presence is taken into account when determining the stage of the disease and choosing a treatment method.
Diagnosis of lymphogranulomatosis
Lymphogranulomatosis can be suspected based on clinical symptoms - swollen lymph nodes, night sweats, weight loss and fever. To confirm the diagnosis, a biopsy or removal of enlarged lymph nodes is performed, followed by morphological, immunophenotypic and molecular genetic studies. The data obtained is used to determine the type of lymphoma.
To detect enlarged internal lymph nodes and determine the stage of the disease, various medical imaging methods are used:
- Ultrasound.
- X-ray of the chest organs. Damage to the mediastinal lymph nodes is indicated by the expansion of the mediastinal shadow.
- CT.
- MRI.
An additional examination is also carried out to assess the patient’s general condition:
- General blood analysis. There are no specific changes. An increase in ESR may be observed (this is an unfavorable sign), and if the bone marrow is damaged, anemia, as well as a decrease in the level of platelets and leukocytes.
- Blood chemistry. It also does not have specific manifestations, but disturbances may occur when internal organs are involved in the process, for example, with liver damage, an increase in the level of transaminases may be observed.
- Bone marrow puncture is performed if the appearance of bone marrow lesions is suspected.
- When planning the use of certain drugs that have cardiotoxicity, an examination of the cardiovascular and respiratory systems is carried out with an assessment of cardiac ejection fraction and pulmonary function.
After a comprehensive examination, a patient with lymphogranulomatosis is assigned to one of three prognostic groups:
- Early stage with a favorable prognosis.
- Early stage with poor prognosis.
- Common stage.
Depending on the group, treatment tactics will be determined. The group is determined according to the GHSG or EORTC/GELA criteria. Poor prognosis factors are:
- Massive mediastinum is a condition in which, on a direct radiograph, the maximum diameter of the tumor is more than a third of the diameter of the chest cavity.
- Involvement of non-lymphatic organs in the process.
- Age over 50 years.
- ESR more than 30 mm/h.
- Damage to 3 or more lymphatic collectors.
Stages
According to one of the popular and widespread classifications, there are four stages of Hodgkin lymphoma (and zero). We will not describe their symptoms, but how the patient feels at each stage:
- 0th. A person feels and behaves as if he is absolutely healthy.
- I. The patient can lead a completely adequate lifestyle, but he is slightly weakened, so physical labor is limited.
- II. Severe fatigue is already noticeable, the person cannot take care of himself, it is difficult for him to move. The patient may spend about half the day in bed.
- III. At this stage, the patient lies a lot (more than half a day) and needs constant care. It is difficult for him to be active and perform even usual actions.
- IV. At this stage, patients are the sickest. They constantly lie or sit, get tired extremely quickly and can even communicate with difficulty and for a short time.
The doctor will explain to the patient what processes occur in the body at each stage of Hodgkin lymphoma - there are many manifestations and their details. It all starts with damage to the lymph nodes or some organs (for example, the spleen) - and then the tumor begins to spread, gradually taking over the body.
Treatment of lymphogranulomatosis
Chemotherapy and radiation therapy are used to treat lymphogranulomatosis.
Treatment of the early stage of lymphogranulomatosis (favorable prognosis)
To treat this form of granulomatosis, 2-4 cycles of chemotherapy followed by radiation therapy (RT) are used. For chemotherapy, a four-component ABVD regimen is used, including adriamycin, bleomycin, vinblastine, and dacarbazine. RT is administered to the primary lesion areas with a total focal dose of 30 Gy. Dose fractionation is used, in which daily sessions (5 days a week) of irradiation are carried out in a single focal dose of 2 Gy until a total focal dose of 30 Gy is achieved.
In addition, lighter treatment options are being considered. For example, if there are no more than 2 affected areas, there are no conglomerates of lymph nodes and a normal ESR, it is possible to limit yourself to two cycles of chemistry. In some cases, it is possible to raise the question of canceling radiation therapy for certain categories of patients based on PET-CT data, but it still remains open.
Treatment of early stages of lymphogranulomatosis with poor prognosis
Treatment of lymphogranulomatosis in this case involves 4-6 cycles of chemotherapy according to the ABVD regimen with radiation therapy of the primary tumor localization zones in a total focal dose of 30 Gy.
For patients under 50 years of age in good general health, treatment can be intensified with two cycles of chemotherapy according to the BEACOPP protocol, followed by 2 cycles of ABVD with standard dose radiation. This program increases the likelihood of 3-year event-free survival, but the question of late toxicity remains open.
Treatment of common stages of lymphogranulomatosis
When treating common stages of lymphogranulomatosis, chemotherapy and irradiation of areas with the largest tumor masses that remain after chemotherapy (residual lesions) are used. The main task at this stage is to achieve complete, stable remission already in the first line of therapy. The choice of treatment tactics depends on the patient’s age and general condition.
For patients under 50 years of age, the BEACOPP-14 regimen is recommended with irradiation of residual lesions larger than 2.5 cm. But this chemotherapy regimen is highly toxic, including to the bone marrow, so planned administration of granulocyte colony-stimulating factors is required.
In order to avoid tumor lysis syndrome, which is also highly toxic, a preparatory phase (prephase) is carried out with vincoalkaloids 10-14 days before the start of planned chemotherapy.
In patients aged 50-60 years, the BEACOPP-14 regimen can provoke the development of severe life-threatening complications, so the standard treatment is the ABVD regimen. A course of 6-8 cycles is used, depending on the tumor response. After completion of chemotherapy, irradiation is carried out according to the standard regimen. It is allowed to use the BEACOPP-14 protocol in healthy patients aged 50-60 years in the amount of 6-8 cycles. Supportive therapy for patients with lymphogranulomatosis is not required.
Treatment of relapses and refractory forms of lymphogranulomatosis
Patients with relapses of lymphogranulomatosis or persistent forms of the disease that are not amenable to first-line therapy are recommended to undergo high-dose polychemotherapy followed by hematopoietic stem cell transplantation. This treatment is carried out in healthy patients under 50 years of age. In other cases, various gentle chemotherapy regimens or radiation are used, which, although they do not allow for a complete cure, do allow for a fairly long-term remission. The choice of treatment regimen is determined individually, taking into account the chemosensitivity of lymphogranulomatosis and the general condition of the patient.
Radiotherapy for lymphogranulomatosis
Radiotherapy for lymphogranulomatosis has played an important role in treatment for many years. But issues of reducing the volume of irradiated tissue and the total focal dose are currently being considered. In general, radiation is given 2-4 weeks after the end of chemotherapy. The maximum interval should not exceed 6 weeks.
When planning irradiation fields, a detailed description of the lesions is made - their location, size, topographical landmarks. After completion of radiation therapy, patients should undergo regular examination in order to promptly identify diseases potentially caused by ionizing radiation. For example, when irradiating the lymph nodes of the neck, it is necessary to regularly examine the thyroid gland (ultrasound + TSH). When irradiating mediastinal lymph nodes, screening for breast cancer, etc. is necessary.
The concept of “lymphoma” unites many diseases that differ in their clinical manifestations, course and prognosis. All lymphomas are divided into two large groups: Hodgkin lymphoma (HL) and non-Hodgkin lymphomas. The first is named after the scientist Thomas Hodgkin, who first described it in 1832 (and the name itself was introduced by WHO in 2001). Synonyms: lymphogranulomatosis, Hodgkin's disease. HL became the first clinically and morphologically recognizable malignant tumor and the first malignant disease in which patients had a chance of complete cure if only radiation therapy was available to the oncologist. Today, successes in the treatment of HL are among the bright victories of oncology.
Alesya Markovets, researcher at the clinical research laboratory of the Republican Scientific and Practical Center for Pediatric Oncology, Hematology and Immunology. Statistics
According to the Republican Cancer Registry, the incidence of Hodgkin's lymphoma in children in Belarus is 1.34:100,000. The disease occurs at all ages except for children under one year of age, extremely rarely - up to 5 years, most often among adolescents from 15 to 19 years. Every year in our country there are about 30 cases of HL among children and adolescents.
Causes and risk factors
The specific cause of HL remains unknown in most cases. The role of viruses in the etiology of malignant lymphomas (Epstein-Barr, cytomegalovirus, herpes virus type 6) is currently being studied, but indisputable evidence of the viral theory has not been obtained. In addition, factors predisposing to the development of HL include various immunodeficiency conditions (taking drugs that suppress the immune system, HIV infection, congenital immunodeficiencies), exposure to ionizing radiation and genetic factors.
Clinical picture
In HL, the tumor is represented by malignant Reed-Sternberg cells and Hodgkin cells. Various internal organs may be affected, causing disruption of their normal functioning.
Tumor conglomerate of cervical lymph nodes in Hodgkin lymphoma. As a rule, the first sign of the disease is a painless enlargement of one or more lymph nodes, often in the neck, less often in the axillary, groin area. Sometimes the tumor process begins in places inaccessible to inspection - the chest (mediastinum) or abdominal cavity. Then the enlarging lymph nodes can put pressure on neighboring organs, causing a dry cough, shortness of breath, and abdominal pain. The tumor can spread to internal organs (lungs, liver, kidneys, etc.).
In addition to enlarged lymph nodes, symptoms such as fever, weakness, night sweats, itchy skin, and weight loss may be observed. These symptoms are taken into account when determining the stage of the disease.
Diagnostics
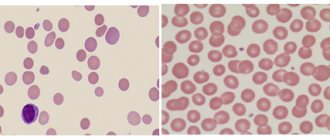
To diagnose HL, it is necessary to perform a biopsy of the affected lymph node or its conglomerate, followed by histological and immunohistochemical studies. The tumor substrate of HL is Reed-Sternberg cells (large binucleate cells) and Hodgkin cells, displacing normal cells of the lymph node of any area of the body. Malignant cells are surrounded by a cellular infiltrate consisting of histiocytes, lymphocytes, monocytes, plasma cells and eosinophils. The histological variant of HL depends on the structure of the reactive microenvironment of tumor cells (cellular composition).
To determine the extent of the tumor process, adequate staging of the disease is necessary before starting treatment. Until recently, ultrasound data of peripheral lymph nodes, abdominal and pelvic organs, CT or MRI were considered standard methods. If necessary, bone marrow biopsy and skeletal scintigraphy were performed.
Currently, the standard examination for HL is positron emission tomography with 18F-fluorodeoxy-glucose combined with CT (PET-CT).
PET-CT allows you to more accurately determine the lymph nodes and areas of the body involved in the tumor process, determine the stage and extent of treatment. In our country, this method has become available to all patients with HL since 2021. The stage of the disease is determined according to the Ann Arbor system (Cotswold staging revision, adopted at a conference in Ann Arbor, USA). This staging system takes into account the number of lymphatic zones and areas involved in the tumor process, the location of the affected lymph nodes on one or both sides of the diaphragm, the presence or absence of extralymphatic spread of the tumor (E), localized or disseminated process, as well as the presence or absence of systemic symptoms (A or in).
According to the International Clinical Classification, there are 4 stages of HL.
Hodgkin's lymphoma diagnostic cells
Reed-Sternberg cell.
Hodgkin cell.
Forecast
In children and adolescents, HL is one of the most curable tumors. About 85–90% of patients with classical HL are cured in the early stages of the disease (compared to 75–80% of patients with advanced stage). Unfortunately, every year from 15% to 20% of primary cases of HL in children and adolescents in Belarus are detected in an advanced form (stage 4).
Treatment
Treatment of patients with HL is a long process, takes from 3 to 12 months and is carried out according to special protocols. Depending on the stage of the disease, patients are divided into 3 groups (with their own intensity and duration of therapy).
Therapy for Hodgkin's disease consists of two stages: polychemotherapy, aimed at maximizing the destruction of malignant cells and achieving remission with the help of chemotherapy, and radiation therapy, aimed at consolidating and long-term maintenance of remission by destroying residual tumor cells, which may subsequently cause a relapse.
Results of treatment for HL at the Republican Scientific and Practical Center DOGI
Over the past decade, the Republican Scientific and Practical Center for Pediatric Oncology, Hematology and Immunology has used a treatment protocol for HL developed by German pediatric oncohematologists, which has shown to be highly effective. Five-year overall survival is 98%, event-free survival is 90%, but in patients with advanced disease (stage 4 disease) it is significantly lower (89% and 74%, respectively). The most significant factor influencing the effectiveness of treatment is the volume of the original tumor, estimated by the size of the lymph node conglomerates (especially the mediastinal lymph nodes) and the number of affected areas. In recent decades, the proportion of patients with no complete effect or relapse of the disease has remained virtually unchanged and is 25% for adults. Among children and adolescents with HL in Belarus, such patients account for 10%.
In Europe and the USA, attempts have been made to treat this category of patients with more intensive chemotherapy regimens (PCT). Since 2021, the Republican Scientific and Practical Center DOGI has also introduced a new protocol for the treatment of patients with high-risk HL. Intensification of therapy in such patients has shown high efficacy and acceptable toxicity.
The first treatment protocols for HL necessarily included high-dose radiation therapy (RT) (35–40 Gy). Over time, it became apparent that the radiation dose could be lower with combination treatments. In addition, it is the delayed effects of RT that are decisive in the development of adverse long-term effects after treatment for HL (secondary tumors, cardiovascular diseases, pulmonary dysfunction).
With the active introduction of PET-CT in the diagnosis of lymphomas, a new era in the treatment of children with HL began. PET-CT has become actively used not only for staging, but also for assessing remission status and early response to therapy. Rapid achievement of PET negativity is a marker of tumor sensitivity to chemotherapy. A way has emerged to identify patients for whom it is possible to refuse RT. Since 2017, RT has been discontinued in patients with early stages who have achieved complete remission according to PET-CT data after completion of the PCT stage.
Despite significant successes in the treatment of HL in children, a certain number of therapeutic failures remain; 5% of patients with HL are refractory to first-line therapy and 5% of patients have a relapse of the disease, with 90% of cases occurring within the first two years. The return of the disease is much more common in patients with advanced stages. If the child relapses late (more than a year has passed since the end of treatment), then the second course of chemotherapy and radiation gives very good results (10-year survival in more than 90% of patients). If the child has an early relapse (3 to 12 months have passed since the end of treatment), very intensive therapy (high-dose chemotherapy with autologous hematopoietic stem cell transplantation (autoHSCT)) is required to have a good chance of recovery. The use of standard second-line chemotherapy in these patients allows achieve an answer in 50% of cases.
As knowledge in the fields of biology, pathology and immunology has developed, it has become possible to find therapeutic targets and develop new drugs that should not only be effective, but also less toxic. This is especially true for pediatric and young patients. The CD30 receptor on HL tumor cells became such a target. Since 2011, it has become possible to use regimens that include a targeted drug (monoclonal antibody brentuximab vedotin for the treatment of patients with refractory and recurrent HL), which leads to a pronounced and sustained response to therapy. Since 2015, the Republican Scientific and Practical Center DOGI has included this drug in anti-relapse treatment regimens, which made it possible to achieve complete remission in 85% of patients with refractory HL.
Currently, the development of treatment methods that reduce the likelihood of complications and long-term consequences in survivors of the disease continues.
Clinical case
Patient M., 17 years old. Considers himself sick since June 2016, when he experienced a weight loss of about 5 kg in 2 months, itching of the skin of the legs and feet, in the evenings a rise in temperature to subfebrile values (max. 37.9 ° C), pain in the knee joints and lumbar region . He was examined by a rheumatologist at his place of residence. Clinical examination revealed an increase in cervical-supraclavicular and axillary lymph nodes; a general blood test revealed an increase in ESR to 62 mm/h, leukocytosis to 12.4-109/l. Antibacterial therapy was carried out (amoxiclav for 7 days), without effect. According to ultrasound data, OBP is focal changes in the structure of the spleen. Consulted with a hematologist at the diagnostic center, with suspicion of a lymphoproliferative disease he was sent to the Republican Scientific and Practical Center DOGI.
At the time of admission to the center (08/30/16): the condition was of moderate severity. Temperature 37.6 °C. The skin and mucous membranes are of normal color and clean. Peripheral lymph nodes: multiple cervical lymph nodes are palpated on both sides up to 2.5 cm, dense, in the supraclavicular region multiple dense ones up to 1.5 cm on both sides, axillary lymph nodes on both sides up to 2.5 cm, dense, mobile, in conglomerates. Other groups of peripheral lymph nodes are not enlarged. Heart sounds are clear, rhythmic, heart rate - 80 per minute. Breathing is vesicular, wheezing is not heard, respiratory rate is 18 per minute. The abdomen is soft and painless. The liver and spleen are not enlarged.
KBC: Hb 119 g/l, erythrocytes 4.29-1012/l, platelets 329-109/l, leukocytes - 13.02-109/l, e - 1%, s - 87%, l - 7%, m - 3%, ESR - 62 mm/h.
BAC: ALP - 107 IU/l, LDH 248 IU/l, bilirubin -17.8 µmol/l, ALT - 30, AST - 23, CRP - 3.4 g/l (normal up to 0.5), urea - 6.5 mmol/l, creatinine - 72 mmol/l, protein - 86.2 g/l.
Ultrasound of the iliac lymph nodes: the iliac lymph nodes are not significantly enlarged; the structure of the spleen is heterogeneous, single lesions up to 10 mm in the structure of the spleen; lymph nodes at the gate of the liver up to 14 mm.
Ultrasound of peripheral lymph nodes: hyperplasia of the lower cervical, supraclavicular, subclavian and axillary lymph nodes on both sides with pathological changes in structure (ultrasound picture of lymphoproliferative disease).
An open biopsy of the axillary lymph node on the left was performed, morphologically - areas of lymph node tissue with the presence of an erased structure, the formation of fibrous septa and accumulations of lacunar, diagnostic and Hodgkin cells. IHC: CD3(+ background cells), CD30(+++), CD15(++), pax5(++), CD20(-), EBV(-).
Hodgkin's lymphoma, variant nodular sclerosis, mixed cellular composition, grade 1. NOS (9663/3).
PET-CT: in the anterior mediastinum of the upper floor, in the middle with an accent to the right, there is a tumor mass; 36-73-60 mm. Isolated enlarged lymph nodes: paratracheal and bifurcation, up to 15 mm; parasternally on the right, up to 18 mm. According to PET data: accumulation of radiopharmaceuticals in addition to the nodes described above - in the right root (bronchopulmonary l/nodes), in l/nodes - precordially on the right, in the cardiodiaphragmatic region on the left, paraesophageal (node on CT, 14 mm).
No foci of pathological density were identified in the pulmonary parenchyma. The pulmonary pattern is not changed. The lobar and segmental bronchi are patent. The roots of the lungs are not expanded, structural. The axillary nodes are not enlarged. The pleural cavities are free. Soft and bone tissues of the chest without structural changes. There is an increase in retroperitoneal lymph nodes, up to 23 mm; common iliac up to 15 mm. On PET, pathological accumulation of radiopharmaceuticals, in addition to the nodes described above, is in the porta hepatis, in the external iliac nodes, and in the spleen.
No pathological space-occupying formations were detected in the abdominal cavity and retroperitoneal space. The liver is not enlarged and has a homogeneous structure. The pancreas is homogeneous, of normal size and position. Kidneys without visible changes.
In the left ilium, a focus of hyperdense density with finely tuberous contours measuring 10.5-6.6 mm is determined. PET also shows increased accumulation of radiopharmaceuticals in the vertebral bodies C6, Tn4, L5, S1; ribs; pelvic bones.
Conclusion: lymphoproliferative disease with damage to the lymph nodes on both sides of the diaphragm, spleen, and bones.
MRI of the pelvic bones, lumbosacral spine, femurs: multiple different-sized foci of pathological signal are determined in the pelvic bones (pubic, iliac, ischial on both sides), femurs on both sides, sacrum (body with transition to the transverse process on the left of the L5 body vertebra, as well as small ones in the body of L4 (up to 9–10 mm) and L2 (up to 5 mm).
Conclusion: MRI picture of multifocal lesions of the pelvic bones, femoral bones on both sides, sacrum, L5, L4, L2 vertebrae.
Diagnosis: classic Hodgkin's lymphoma (nodular sclerosis variant) with damage to the cervical-supraclavicular lymph nodes on both sides, subclavian lymph nodes on both sides, mediastinal lymph nodes, root of the right lung, axillary lymph nodes on both sides, lymph nodes at the porta hepatis, para-aortic lymph nodes, spleen, iliac lymph nodes on both sides, multiple lesions of skeletal bones. Stage IVB.
The patient underwent 6 blocks of PCT according to BEACOPP-escalated schemes.
A complete metabolic response was obtained according to PET-CT data after the PCT stage. In order to consolidate remission, radiation therapy was performed on the areas of the initial lesion in SOD = 20 Gy.
Special treatment completed on 03/21/17. The patient is still in stable remission and is being monitored by an oncologist at his place of residence.