The signs of bronchitis and pneumonia are very similar; quite often acute bronchitis develops into pneumonia - a serious disease that threatens to develop severe consequences, including death, especially when it comes to the elderly. Despite some differences, both bronchitis and pneumonia often have common, mild symptoms. Therefore, in order to avoid a sad outcome, if you suspect pneumonia, you should never hesitate to consult a doctor, especially since bronchitis turning into pneumonia is a fairly common occurrence. One of the leading clinics involved in the diagnosis and treatment of the upper respiratory tract in Moscow is the Yusupov Hospital.
Respiratory damage to the bronchi: features
With bronchitis, the bronchioles of the airways leading to the lungs become swollen and excess mucus accumulates. The disease is provoked by a viral pathogen, followed by the addition of a bacterial infection. Young children are most susceptible to developing bronchitis. This fact is due to the narrowness of their respiratory tract and the lack of maturity of the immune system, which is unable to fight numerous respiratory infections. Therefore, both bronchitis and pneumonia in children are quite common.
Bronchitis is considered a highly contagious disease, as it is easily transmitted by airborne droplets. You can easily become infected with a dangerous virus by sneezing, coughing, or by contact with infected secretions on the surface of objects.
“Caution, the bronchi are closing,” or what is COPD
It is no secret that the bronchi and lungs come into direct contact with the air, every second “fighting off” thousands of toxic or abrasive air particles. Of course, some kind of cleaning system still exists, but its possibilities are not unlimited.
The “cleaning system” is not omnipotent
COPD, or chronic obstructive pulmonary disease, is better known as chronic bronchitis and emphysema.
According to WHO, about 250 million people worldwide suffer from the disease. At the same time, in developed countries the main cause is considered to be smoking, and in third world countries it is smoke from solid fuel (wood or coal) for cooking.
Toxic emissions from production, general dust levels in the air, and even the “atmosphere” in the room also play a role.
But it is not the air quality itself that is decisive, but the frequency and intensity of its influence.
Rare exposure to cigarette smoke, obviously, is not capable of provoking serious changes, because the inflammation of single cells quickly passes, and new ones replace the “dead” ones.
“Superficial” renewal of bronchial cells occurs approximately every 2-3 weeks, and complete “restoration” occurs within a year.
However, if aggression occurs on a regular basis, the inflammation becomes chronic.
When defense works against you
Any aggressive effect on bronchial cells is accompanied by a number of protective reactions: coughing, sputum production and attraction of immune cells to the site (inflammation).
In the case of chronic influence, excessive secretion of mucus leads to the accumulation of sputum, and damage to the epithelium leads to disruption of its movement “out”. The cough becomes unproductive, and sputum accumulates in the bronchi, mechanically narrowing their lumen.
The influence of inflammatory mediators provokes spasm of the bronchi and bronchioles. Which, normally, is also an element of protection that “blocks” the way for harmful substances into the respiratory tract. But with prolonged use, it leads to significant breathing problems.
And the destruction of the elastic tissue of the bronchi and lungs under the influence of their own, overly active enzymes, leads to a limitation of their normal expansion and contraction during breathing, “overstretching” of the lungs, and is subjectively felt as shortness of breath.
COPD is a threat to life
According to statistics, COPD occupies a leading position in the overall structure of causes of mortality.
The fact is that the disease develops surprisingly slowly, and more often makes itself felt after decades of influence of negative factors. Like, for example, COPD of smokers, which receives life-threatening status only after 30-40 years of smoking. That is, on average, by the age of 50 or more years of age, when the disease is most often detected.
Increasing shortness of breath, first appearing during movement and then at rest, provokes complications in the heart and general oxygen starvation, which is especially significant for the brain. Accumulation of sputum - infection. And chronic inflammation in such rapidly renewing cells as the bronchial epithelium significantly increases the risk of cancer.
Thus, the cause of death in COPD can be not only pulmonary failure itself, but also heart failure, as well as cancer.
And among the milder “side effects” of the disease are exhaustion, chronic fatigue, decreased thinking abilities, headaches and other pathologies.
Diagnostics
The diagnosis of COPD can be established only on the basis of an X-ray of the lungs (or CT scan), as well as their functional study (determination of capacity and volume).
An alpha-1 antitrypsin blood test can be used as an additional diagnostic method.
Genetically determined deficiency of this enzyme provokes the destruction of the elastic tissue of the lungs even in non-smokers and, unlike COPD, at any age. And therefore, the test is more often prescribed if a patient under 40 years of age complains of wheezing, chronic cough, severe shortness of breath after exercise, but does not smoke or is not chronically exposed to dust.
Antitrypsin deficiency also indicates a high risk of developing COPD in the future, even if no symptoms are currently observed. Therefore, the analysis can be used as a reliable prognostic marker.
Clinical picture of acute bronchitis
The onset of bronchitis is similar to acute respiratory disease (acute respiratory disease). It manifests itself in the following conditions:
- runny nose and nasal congestion;
- dry cough without mucus at the beginning of the disease;
- the appearance after a few days of clear, yellowish or green sputum;
- the occurrence of headache, chills (in the absence of fever or the presence of slight hyperthermia);
- absence of pathologies in the lungs, confirmed by x-ray studies;
- recovery occurs in two to three weeks.
The symptoms of bronchitis and pneumonia are different, but both of these pathologies are accompanied by rapid breathing, wheezing and the appearance of a bluish tint on the skin associated with a lack of oxygen.
Treatment of the disease is aimed at preventing infection from entering the alveoli. To alleviate the condition, antihistamines, bronchodilators, steroids, and oxygen therapy are prescribed. With the help of properly selected medications, pulmonologists at the Yusupov Hospital Therapy Clinic are able to prevent the development of pneumonia and the chronic course of the disease, which may require longer treatment.
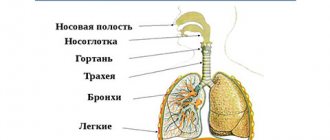
Lungs
Lung structure
The lungs are paired organs located in the chest cavity. They consist of lobes: the right lung contains three lobes, the left - two. Lung tissue consists of bubbles - alveoli, in which a vital process occurs - gas exchange between blood and atmospheric air.
The lung is covered with a membrane - the pleura, which passes from the surface of the lungs to the inner walls of the chest. A pleural cavity is formed between the two layers of the pleura, the pressure in which is lower than atmospheric (it is called negative pressure), which is of fundamental importance for the act of inhalation and exhalation.
Gas exchange in the lungs and tissues
The air moves along the airways and finally reaches the smallest structure of the lung - the pulmonary vesicle, or alveoli. The wall of the alveoli is intertwined with a dense network of capillaries - vessels with a thin wall through which gases diffuse: carbon dioxide leaves the blood into the alveoli, and oxygen enters the blood from the alveoli.
Oxygen dissolved in the blood reaches the internal organs and tissues of the body through the blood vessels. I note that moving through the blood, gases form compounds with hemoglobin in red blood cells:
- Oxygen (O2) - oxyhemoglobin
- Carbon dioxide (CO2) - carbhemoglobin
- Carbon monoxide (CO) - carboxyhemoglobin
The combination of hemoglobin with carbon monoxide is much more stable than the others: carbon monoxide easily wins the competition with oxygen and takes its place. This explains the severe consequences of carbon monoxide poisoning, which quickly accumulates during a fire in a confined space.
As the blood gives up carbon dioxide and takes in oxygen, it turns from venous blood (poor in oxygen) into arterial blood. In tissues, the reverse process occurs: cells need oxygen necessary for tissue respiration, and carbon dioxide, a byproduct of metabolism, requires removal from the cell into the blood.
I often ask students, “What moves the gas, what causes, for example, oxygen to move first from the alveoli to the blood, and in the tissues from the blood to the cells?” Remember that this driving force is the difference in partial pressure of gases.
The partial pressure of a gas is that part of the total volume of gas that falls on the share of this gas. I do not recommend that you memorize the table above, but it is quite good for understanding.
Note that the partial pressure of oxygen in the alveoli is 100-110, and in the venous blood of the capillary that encircles the wall of the alveoli, the oxygen pressure is 40. Thus, oxygen rushes from an area of higher pressure to an area of lower pressure - from the alveoli into the blood.
The ongoing movements of gases can be easily recorded by measuring the concentration of gases in the air inhaled and exhaled by a person. You probably won't need much of this information, but I encourage you to remember that the ambient air contains 21% oxygen and 0.03% carbon dioxide - this is important information.
The liquid covering the walls of the alveoli - surfactant - is important in the transport of gases. Initially, oxygen dissolves in the surfactant and only then diffuses through the capillary wall, entering the blood. Surfactant also prevents the walls of the alveoli from sticking together (collapsing) during exhalation.
Vital capacity of the lungs
One of the physiologically important indicators is vital capacity (VC). Vital capacity is the maximum amount of air that a person can exhale after the deepest breath.
This indicator is very variable; the average vital capacity of an adult is about 3500 cm3. In athletes, vital capacity is 1000-1500 cm3 more, and in swimmers it can reach 6500 cm3. The greater the vital capacity, the more air enters the lungs and oxygen enters the circulatory system, which is very important for tissue cells during sports.
Vital vital capacity is easily measured using a special device - a spirometer (from the Latin spirare - to breathe).
Mechanism of pulmonary respiration
Between the outer surface of the lung and the walls of the chest there is a pleural cavity, which plays a vital role in the process of inhalation and exhalation, and also reduces friction of the lungs during breathing movements.
The pressure in the pleural cavity is always 5-7 mm lower. rt. Art. atmospheric pressure, so the lungs are constantly in an expanded state, fastened through the pleura to the walls of the chest cavity.
Imagine: the lung is pulled up to the pleura, which is attached to the chest. And the chest constantly makes breathing movements, expanding and contracting, thus the lung follows the respiratory movements of the chest.
It remains to figure out how these respiratory movements occur? The reason for this is the contraction and relaxation of the intercostal muscles, as a result of which the chest rises and falls, respectively. Now we will discuss in detail the mechanism of inhalation and exhalation.
When inhaling, the external intercostal muscles contract, while the ribs rise, and the sternum moves forward - the chest expands in the anteroposterior and frontal (to the sides) directions. The diaphragm is a respiratory muscle; during inhalation it contracts and moves down: the chest expands in the vertical direction.
When you exhale, the internal intercostal muscles contract, the ribs lower, the sternum moves back - the chest narrows in the anteroposterior and frontal (to the sides) directions. During exhalation, the diaphragm relaxes and rises: the chest narrows in the vertical direction. Thanks to these movements, inhalation and exhalation are carried out.
Can we take control of our breathing? Easily. But we don’t always control it even during the day, let alone at night. The breathing process is controlled by the respiratory center located in the medulla oblongata of the brain. The respiratory center is automatic - periodically impulses themselves flow to the respiratory muscles, for example, during sleep.
The composition of the blood greatly affects the intensity of breathing. Numerous experiments have shown that an increase in CO2 concentration stimulates the respiratory center. This can explain the increase in breathing during physical activity, for example, running, when CO2 is actively formed in the muscle cells of the legs and enters the blood, breathing becomes more frequent reflexively.
The reflex regulation of breathing is most clearly demonstrated by the experiment with cross circulation, in which the circulatory systems of two dogs are connected. When the trachea is compressed, the first dog stops breathing, and carbon dioxide stops being removed from the blood - its concentration in the blood increases, which leads to shortness of breath (rapid breathing) in the second dog.
Pneumothorax
Normally, the pressure in the pleural cavity is negative, which stretches the lungs. However, with injuries to the chest, the integrity of the pleural cavity may be disrupted: in this case, the pressure in the cavity becomes equal to atmospheric pressure.
Violation of the integrity of the pleural cavity is called pneumothorax (from the ancient Greek πνεῦμα - blow, air and θώραξ - chest). When pneumothorax occurs, the lungs collapse and cease to participate in breathing.
Mountain and decompression sickness
Climbers and mountain hikers (especially beginners) often experience altitude sickness. This condition occurs due to the fact that when rising to a height, the partial pressure of oxygen drops, and its concentration in the blood does not meet the body's needs - it is lower than it should be.
At first, mountain sickness manifests itself as euphoria (unreasonable joy) and increased heart rate. If the conquest of mountain peaks continues, then these symptoms are gradually joined by apathy (a state of indifference), muscle weakness, cramps and headache.
What to do, you ask? It is necessary to immediately stop further ascent, and if symptoms worsen, begin descent. It is best to prevent altitude sickness by following the rule - do not increase the altitude of your overnight stay by more than 300-600 meters.
Caisson disease occurs in divers and is associated with an increase in the partial pressure of a gas - nitrogen, which occurs when diving under water. There is a pattern: the deeper the diver descends, the more nitrogen becomes dissolved in the blood. What is the danger of nitrogen dissolving in the blood?
With a sharp, rapid rise, the solubility of nitrogen in the blood decreases, and the blood literally boils. Just imagine, real gas bubbles appear in the vessels! They can clog the vessels of the lungs, heart, and other internal organs, as a result of which blood circulation stops, and the consequences can be very sad, even fatal.
How to prevent decompression sickness? You can use helium gas in the breathing mixture instead of nitrogen, which does not lead to such consequences. It is also necessary to adhere to the rule of gradual ascent, with stops, and avoid sudden ascent.
© Bellevich Yuri Sergeevich 2018-2021
This article was written by Yuri Sergeevich Bellevich and is his intellectual property. Copying, distribution (including by copying to other sites and resources on the Internet) or any other use of information and objects without the prior consent of the copyright holder is punishable by law. To obtain article materials and permission to use them, please contact Yuri Bellevich
.
Pneumonia: features
The development of pneumonia is caused by a complication after an infectious process in the upper respiratory tract, bronchitis or a primary infection. Pneumonia affects the alveoli and terminal airways. Due to the fact that the disease manifests itself with symptoms identical to the common cold, its first signs are often neglected.
The cause of pneumonia often lies in an infection or an allergic reaction of the body. You can determine the difference between bronchitis and pneumonia with the help of an experienced diagnostician, since the inflammatory process in the alveoli of the lungs is accompanied by slightly different symptoms.
The presence of pneumonia can be assumed in the following conditions:
- high temperature (exceeding 38.5 degrees);
- active secretion of sputum;
- hemoptysis;
- pain in the chest area;
- difficulty breathing;
- increased heart rate (more than 100 beats per minute);
- increased breathing (more than 24 per minute);
- duration of the disease exceeding two to three weeks.
Complications of pneumonia can include:
- lung abscess;
- respiratory failure;
- exudative pleurisy;
- septic fever.
Damage to the alveoli of the lungs is detected using the same diagnostic tests that are carried out for bronchitis. The correct selection of antibacterial drugs and their timely administration guarantee effective treatment and elimination of infection in the lungs.
Visualization of bronchial diseases (part 2)
Transcript of the second part of the video lecture by Professor Igor Evgenievich Tyurin on the visualization of bronchial diseases, images from the second program of the radiology diagnostics series for therapists.
Igor Evgenievich Tyurin, professor, doctor of medical sciences:
— Since obstructive diseases themselves are considered a risk factor for the development of many socially significant, important, latent diseases, X-ray examination for such patients is of certain importance for identifying a malignant tumor, tuberculosis. It may be detected somewhat more often in this category of patients than in the general group of patients.
What changes can we detect with X-rays and CT scans? I tried to divide these pathological conditions into several component parts in order to make it more systematic, understandable, methodical, from the point of view of the perception of sometimes quite complex X-ray and tomographic symptoms.
X-ray changes. Signs of bronchitis, bronchial obstruction and emphysema.
Unfortunately, when it comes to a conventional X-ray examination or even a computed tomography examination, radiologists and attending physicians relatively rarely differentiate these symptoms and clinical radiological manifestations from each other. Although the manifestations, even with conventional x-ray examination, are completely different. We must be able to find these signs even on a regular x-ray in order to accurately characterize the pathological process.
What are x-ray changes in the form of signs of chronic bronchitis? Precisely chronic bronchitis, because acute inflammation of the bronchial mucosa, as a rule, does not find any reflection in X-ray and tomographic examination. In fact, neither one nor the other is intended for the diagnosis of acute respiratory viral infections with damage to the paraximal or middle caliber bronchi.
Common signs, such as enhancement and deformation of the pulmonary pattern, are added by radiologists to their protocols through the interstitial component. Thickening of the walls of the bronchi, which we can see on x-rays and tomograms, is defined as peribronchial couplings. At the same time, perivascular couplings.
Bronchial dilatation is possible. But with conventional X-ray studies, in contrast to tomographic studies, we see dilated bronchi much less often and not as confidently as with CT.
If we return to conventional X-ray examination, then in patients with obstructive diseases we see these changes in the large bronchi in the hilar region. This is due to thickening of the walls of the bronchi.
(Slide show).
The arrows here indicate peribronchial couplings, that is, thickening of the walls of the bronchi, which we can see in longitudinal or cross section. It quite accurately and adequately reflects the severity of the chronic inflammatory process in the bronchi themselves. Plus, there is a change in the pulmonary pattern due to the pulmonary interstitium, which we can observe in such patients.
03:22
But what I would like to draw your attention to. We will return to this more than once today. These changes immediately on the basis of one x-ray cannot be interpreted as irreversible changes, as manifestations of pneumosclerosis, or any specific morphological type of changes in the lung tissue.
Most often, we see such patients during an exacerbation of the disease, when it is not so much and not only about sclerotic changes in the walls of the bronchi or in the peribronchial lung tissue, but rather about swelling of the walls of the bronchi, incoming changes. In fact, this picture resembles interstitial edema with peribronchial changes.
As soon as these acute symptoms go away and the patients return to their stable state, the X-ray picture very often also indicates the disappearance of a significant part of these signs, which are sometimes not entirely correctly characterized as irreversible changes.
With a conventional X-ray examination, we rarely see signs of bronchi dilatation, bronchiectasis, or cystic cavities with relatively thick walls. Sometimes we even see fluid levels in them (during an exacerbation).
These are pronounced changes that can be observed in advanced stages. They need to be differentiated from other diseases that can lead to the formation of bronchiectasis in addition to obstructive pulmonary disease.
It is fundamentally important that on x-rays we see quite clearly signs of bronchial obstruction. This:
- flattening of the diaphragm;
- limitation of her mobility;
- vertical position of the heart;
- increase in retrosternal space;
- signs of pulmonary arterial hypertension that may occur in this type of patient.
05:14
It is no coincidence that the flattening of the diaphragm and the limitation of its mobility are written in the first two lines. It has long been known and well proven that these are the two most important, reliable, accurate signs that characterize a violation of the passage of air through the small bronchi and an increase in the residual volume in the lungs.
When we interpret or review x-rays of the chest cavity, then, first of all, we pay attention not to the degree of transparency of the lung tissue, which depends extremely variable on age, on the constitution, on the physical conditions of the x-ray, but on the position of the mediastinum, diaphragm, retrosternal space.
Flattening of the diaphragm and changes in the configuration of the chest are the two most important radiological signs that allow us to talk about the formation, the presence of obstructive changes in the lung tissue. Previously, fluoroscopic examination was much more often used for this purpose. Radiologists could evaluate the mobility of the diaphragm and the limitation of this mobility in patients with obstructive diseases.
Nowadays this is done much less frequently. But we see it well. An increase in the retrosternal space and a flattening of the dome of the diaphragm, which should have a dome shape as the main respiratory muscle. These are two of the most important signs of the presence of bronchial obstruction in this type of patient.
Where these changes reach a significant degree of severity, we see not only changes in the configuration of the chest, which takes on a typical beam-like shape. Not only a flat or even concave diaphragm towards the abdominal cavity, but also those signs that radiologists mention in their reports.
This is an increase in the airiness of the lung tissue, a depletion of the pulmonary pattern, which is practically indistinguishable against the background of the exceptionally high air content in the lung tissue. A classic example of such obstructive disease is on x-ray.
07:40
These changes can be traced over time if we observe such patients for quite a long time. This can lead to typical changes in the configuration of the chest cavity and changes in the position of the diaphragm and mediastinal organs.
Doubtful signs (that's how I would label them). I specifically draw your attention to this, because in the protocols these signs are often designated as characteristic manifestations of an obstructive state or manifestations of emphysema.
This is not entirely true, because the increase in airiness of the lung tissue, and the low location of the diaphragm, which we see on photographs in direct projection, and the expansion of the intercostal spaces are signs that to a very significant extent depend on the constitution, on many other technological factors. They do not always correctly reflect the condition of the lung tissue.
What signs characterize these same changes on CT. Everything that we just said for a regular X-ray examination can also be observed with a CT scan. But in addition to this, we observe several more very important and interesting signs, which we will talk about in more detail today.
These are expiratory air traps, deformation of the trachea, which is visible on X-ray examination, but is also accurately and clearly detected on CT. This is expiratory bronchial collapse. In some cases, this is a symptom of mosaic density, which characterizes the density and uneven airiness of the lung tissue.
Air traps are a classic sign of bronchial obstruction, which is detected on CT.
(Slide show).
In this patient, when examined during exhalation, the lower lobes of the lungs appear to be as airy as during inspiration. The upper ones naturally increase their density, or their airiness decreases due to the fact that the volume of air in the alveoli during exhalation becomes smaller.
Such large air traps, which occupy lobes of the lung or several segments or a segment of the lung, are indeed of great diagnostic value and allow us to judge the nature of the pathological process.
10:03
They are detected with high-resolution CT, at the height of deep delayed exhalation and occur when the passage of air through the small bronchi is delayed. They vary in volume. Only relatively large changes (segmental, lobar air traps) are of clinical significance.
Small areas of increased airiness during expiratory examination can also be observed in completely healthy people without any diseases in this area.
A saber-shaped trachea or trachea like a saber sheath is a radiological syndrome of bronchial obstruction, when the trachea is compressed by enlarged lungs on both sides of the sagittal plane and takes on a peculiar shape. In direct or frontal projection, it is small and narrow. In the lateral projection of the sagittal plane, the dimensions are quite wide.
Expiratory bronchial collapse can also be a manifestation of bronchial obstruction and create a very interesting clinical picture, which is not entirely typical for the usual clinical picture of obstructive pulmonary disease.
We can clearly see this with expiratory CT scans. The bronchi, segmental and subsegmental, clearly visible during inhalation examination, turn out to be collapsed and practically indistinguishable against the background of the lung tissue during exhalation examination. This slows down the release of air from the lung tissue and creates corresponding clinical symptoms.
11:36
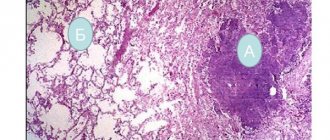
Emphysema as one of the most important manifestations of obstructive pulmonary disease and chronic obstructive pulmonary disease. Standard, traditional definition that has existed for many years. Pathological irreversible increase in the air-containing spaces of the lung as a result of destruction of lung tissue in the absence of inflammatory changes.
What is fundamentally important in this definition is what is important for radiology diagnostics, for tomographic studies, for evaluating X-ray data. Emphysema is an irreversible pathological condition that is accompanied by pronounced morphological changes in the lung tissue. This is an increase in the amount of air in the lung tissue associated with the destruction of lung tissue.
This fundamentally distinguishes emphysema from many other functional disorders that can occur in the lung tissue. Functional changes as a result of hyperventilation, an increase in the volume of lung tissue, in which no disturbances in the structure of the lung tissue occur.
The task of X-ray examination and CT is precisely to try to identify these morphological signs, determine their localization, and degree of severity. On this basis, determine or propose some kind of possible treatment measures.
The types of emphysema are familiar to everyone. It differs in the nature of changes in the lung tissue. It can be localized in the upper and lower lobes and have a diffuse distribution.
From the point of view of morphological changes, well-known diagrams of the pathology of small airways and lung tissue clearly show why normal airways and the adjacent air-containing spaces, expanding, form panacinar, centriacinar and distal acinar emphysema.
13:39
These changes, if we are talking about radiographic studies, are not so easy to identify. With X-ray examination, we must determine morphological changes in the lung tissue. Not functional, associated with an increase in the amount of air remaining in the lung tissue, but morphological.
Conventional radiography is not very accurate in distinguishing between these two pathological conditions. We can detect direct radiological signs of emphysema. This is a local depletion of the pulmonary pattern (vascular zones). This is a violation of the architectonics of the pulmonary pattern (pushing, pushing apart, displacement of blood vessels, some individual areas due to the formation of individual cavities).
Direct visualization of the walls of the bullae, which we can detect on x-rays. This will be a direct indication for establishing the presence of emphysema as a pathological condition.
(Slide show).
This is one example of the fact that it is not always easy to navigate the nature of changes in lung tissue and reliably and accurately state that there really is emphysema. Signs of emphysema and increased lung volume in this patient are expressed completely differently than in previous patients.
However, if you look at the image in a lateral projection on the upper part of the lung field, you will notice an unusual pulmonary pattern - something similar to the cavities that form in this part of the lung.
If we return to the CT scan, in the left lung almost the entire upper lobe is replaced by a large number of air cavities with thin walls. Between them there is compressed lung tissue. This picture is the cause of the pathological changes that appear on the x-ray.
Identifying such vascular zones or areas lacking a pulmonary pattern, or the walls of the air cavities themselves, which we can sometimes see in such patients, helps us to correctly assess the nature of the pathological changes.
But when we see such a picture, when almost the entire right lung is replaced by huge air cavities, the remaining lung tissue is shifted towards the mediastinum, and most of the right lung and the entire upper lobe of the left lung are occupied by huge air cavities, in this case the radiologist’s conclusion about the presence of emphysema is correct, strict and completely objective.
16:27
Something to look at critically. When we do not see this kind of direct signs of emphysema, then talking about the presence of emphysema only on the basis of deformation of the pulmonary pattern or some asceological features of the pulmonary pattern (especially during fluorographic studies) is an element of overdiagnosis or an x-ray stamp. It is hardly reasonable to use it in protocols or in descriptions of radiological studies.
The types of emphysema that we can see on CT are centriacinar, panacinar, and distal acinar emphysema.
(Slide show).
This is what they look like on a CT scan. What is the advantage of this technology. The fact is that we can find direct morphological signs of this condition in situations where this is practically impossible with conventional x-ray examination.
This is especially true for small centrilobular or centriacinar changes, when small air-containing cavities are formed in the lung tissue, bordering the lung tissue. They can only be seen on CT when it comes to intravital examination of the lungs. Compared to morphological studies (inaudible, 17:42) this is very large.
Centrilobular emphysema is a common pathological condition that occurs in a significant proportion of people who abuse smoking, in most patients suffering from chronic obstructive pulmonary disease, which we see in almost all patients in the 3rd and 4th stages of this disease.
It is characterized by the predominance of changes in the upper lobes of the lungs, sometimes in the 6 bronchopulmonary segments, and the formation of relatively small air cavities in the lung tissue, the walls of which can be either the lung tissue itself or the interlobular septa.
This predominant localization in the upper lobes of the lung without pronounced subpleural localization is a typical picture for this type of patient. It is reliably detected by CT. Although it is completely unobvious with conventional x-ray studies.
18:43
Panlobular emphysema is a much rarer condition. It is characterized by diffuse expansion of the acini and fusion of intralobular structures into a single air space. This condition can often be observed in diffuse forms of emphysema and in cases of β-antitrypsin deficiency.
Congenital pathology, especially when it comes to young people. Especially in cases where these young people do not have obvious clinical symptoms for obstructive pulmonary disease, and there is no reason for its development.
In this case, performing a tomographic study and detecting a similar computed tomographic picture, when we see the predominance of these changes (increased airiness, destruction of lung tissue, formation of intrapulmonary cavities mainly in the lower parts of the lungs), suggests the possible nature of emphysema in these patients and forces carry out the necessary amount of additional research.
The most familiar pathological condition is paraseptal or bullous emphysema. Air cavities are localized along the visceral pleura, especially along the mediastinal pleura and costal pleura. This type of emphysema is and often serves as the cause for the formation of spontaneous pneumothorax. This is the clinical significance of this type of emphysema.
For patients with spontaneous pneumothorax, performing a CT scan after straightening the lung tissue is fundamentally important so that further tactics and the course of treatment of the patient can be determined.
Bullous emphysema is a condition that can almost always be seen with a routine x-ray. It is characterized by obvious changes on CT scan. Here, CT scans are performed not so much to diagnose this condition, but in most cases to those patients who are scheduled to undergo lung volume reduction surgery, to assess the exact location of the bullae and the possible type of surgery for the patient.
21:00
Such bullae can lead to compression of the lung tissue. This is clearly seen in the condition of the lower lobe of the right lung in this patient. As a consequence, surgical resection of these bullae results in straightening of the lung tissue. In many cases, it improves the quality of life of such a patient.
CT, in contrast to conventional x-ray examination, which is aimed more at identifying functional changes and signs of bronchial obstruction, is a very accurate, reliable tool for determining the phenotypes of chronic obstructive pulmonary disease and, in general, changes in lung tissue that occur in patients with any obstructive disease lungs.
The clinical presentation of these patients may vary significantly. The morphological changes in their lung tissue can also be completely different. Depending on whether in this patient changes predominate in the bronchial tree (in the middle, in the small bronchi) or in the lung tissue in the form of the development of emphysema and various types of air cavities of this localization.
Solving anatomical issues, distinguishing between types of obstructive pulmonary disease, and CT scans are of fundamental importance in differential diagnosis.
As a conclusion, a brief overview of what we see on X-rays and CT scans in patients with bronchial obstruction, I will repeat once again. In most patients, the presence of emphysema and bronchial obstruction can be confidently assumed based on conventional plain radiography.
To date, this is the original technique, research intended for such patients.
Why do you need high-resolution CT? Do you mean a conventional step-by-step study or a multi-slice CT scan? It allows you to identify emphysema, clarify the nature of changes in the lung tissue, the type of emphysema, and give it a quantitative description.
To this we add that multilayer CT today is a very accurate and powerful tool for assessing the bronchial tree in general. Not only in this category of patients, but also in patients with other pathological processes in the lung tissue (bronchiectasis, bronchiolitis).
Irina Alexandrovna will talk about this in detail. I'll end here.
What is the difference between bronchitis and pneumonia?
Regardless of which disease is suspected in the patient - bronchitis or pneumonia, there are no differences in diagnostic tests to identify it. In order to differentiate both pathologies, you need to know the following signs of distinguishing bronchitis from pneumonia:
- inflammation of the bronchi is caused predominantly by a viral agent, while pneumonia is of bacterial origin;
- Patients with pneumonia have a high temperature and chills, while with bronchitis there is only a slight fever;
- diseases are characterized by different types of wheezing: with bronchitis, wheezing with a whistle, with inflammation, wheezing is wet and dry;
- damage to the bronchi is accompanied by the formation of scars and the development of edema in the respiratory tract, in contrast to pneumonia, in which edema and accumulation of fluid occurs in the pulmonary alveoli.
Acute bronchitis - symptoms and treatment
Uncomplicated forms of acute bronchitis
Treatment of uncomplicated forms of acute bronchitis is carried out on an outpatient basis.
Patients need to know the “red flags,” i.e., symptoms that require immediate medical attention. "Red flags" for bronchitis:
- High fever, chest pain or headaches increase after 2-3 days of treatment.
- Breathing problems such as wheezing or shortness of breath occur.
- Cough with blood discharge. The blood may be bright red, but the sputum may be dark or rusty in color.
- Severe weakness, lethargy.
- The cough lasts longer than 3-4 weeks.
These symptoms may indicate a complicated course or development of chronic bronchitis.
It is not recommended to use in therapy:
- Antihistamines (use is justified only when allergies occur in acute bronchitis) and physiotherapeutic treatment due to the lack of evidence of their effectiveness.
- Mustard plasters, pepper plasters, jars. The harm from their use significantly outweighs the possible benefits (there is a possibility of allergic reactions and thermal burns).
- Antibiotics for viral, uncomplicated acute bronchitis [9].
- Medicinal herbs, as there is insufficient evidence of their effectiveness and safety [10].
There is no “quick fix” for a cough due to a viral infection. The main goal of treating bronchitis is to relieve symptoms while the patient's immune system fights off the infection. The most effective methods of treating acute viral bronchitis:
- Prescription of antiviral drugs (only for flu symptoms) [11].
- Taking paracetamol, ibuprofen in age-appropriate dosages to reduce high fever and relieve any pain.
- Drink plenty of fluids to prevent dehydration [12].
- Frequent ventilation of the room, creating optimal humidity levels (40-50%) and temperature 19-22 °C.
- To give up smoking. Cough and serious lung diseases are more common in smokers.
Patients, as a rule, buy a wide variety of cold and cough remedies at the pharmacy. There is little evidence of any effect on infection, but some may be useful in treating certain symptoms. For example, vasoconstrictor drops help relieve symptoms of nasal congestion.
In March 2009, the Medicines and Healthcare Products Regulatory Agency (MHRA, UK) released an important statement stating:
Parents and guardians should no longer use over-the-counter cough and cold medications on children under 6 years of age. There is no evidence that they work, and they may cause side effects such as allergic reactions, sleep disturbances, etc. For adults looking for a cough suppressant (for short-term use only), over-the-counter medications with some evidence of effectiveness include dextromethorphan, guaifenesin, dexbrompheniramine/pseudoephedrine and bromhexine. Codeine is not an effective cough suppressant and should be avoided. Products containing pelargonium (Pelargonium sidoides) extract, such as Umcka ColdCare, may reduce symptoms and speed resolution of acute bronchitis in adults. Significant improvements in cough relief have been observed with Vicks Medinite syrup [13]
Recommendations of the Russian Federation
For dry, painful, painful cough, absence of wheezing in the lungs and other signs of bronchial obstruction, butamirate can be used. For viscous, poorly discharged sputum, it is possible to prescribe ambroxol, and from the age of two - acetylcysteine and carbocysteine.
Acute obstructive bronchitis
Therapy of acute obstructive bronchitis has its own characteristics. Treatment is indicated using a device that sprays drugs directly into the respiratory tract - a compressor inhaler (nebulizer). Children under 5 years old - use a mask, over 5 years old - a mouthpiece.
The following drugs are used:
- Inhaled β2-agonists (salbutamol/Ventolin nebula) or combination drugs (fenoterol + ipratropium bromide - Berodual) are mixed with a solvent (0.9% sodium chloride solution) and are used to dilate the bronchi and relieve their edema [14].
- Inhaled corticosteroids (ICS) - a suspension of budesonide in nebulas. This is an effective anti-inflammatory drug with a high level of safety.
The second method, less preferable, is the administration of the same groups of drugs through a metered dose aerosol inhaler (MDI) with a spacer (special adapter) and an appropriate face mask or mouthpiece. The duration of the course, doses of drugs and the frequency of their use are determined by the doctor.
Syrup forms of bronchospasmolytics, including aminophylline, are not recommended due to possible side effects [15]:
- From the nervous system: headache, dizziness, increased nervous excitability, sleep disturbances, drowsiness, tremor, convulsions.
- From the digestive system: nausea, vomiting, diarrhea, exacerbation of gastric and duodenal ulcers, increased activity of hepatic transaminases (enzymes that reflect the functionality of the liver). It happens extremely rarely.
- From the cardiovascular system: tachycardia, decreased blood pressure, collapse (a life-threatening condition caused by a drop in blood pressure and deterioration of blood supply to vital organs).
- From the urinary system: pink coloration of urine.
- Allergic reactions: skin rash, urticaria, paradoxical bronchospasm.
Treatment of acute bronchiolitis
- Use of general principles for the treatment of acute bronchitis.
- Humidified oxygen therapy is recommended if the amount of oxygen in the blood (SpO2) is less than 92-94% (normal is 95-98%). Most often, oxygen therapy is carried out by insufflating oxygen through nasal catheters (cannulas) or a mask.
- Nebulizer therapy is selected individually and may include bronchodilators (drugs that relax the muscle elements in the wall of the bronchi and thereby increase their lumen), 3% sodium chloride solution, etc. The effect of glucocorticosteroid therapy has no evidence [16].
Bacterial bronchitis
For bronchitis caused by mycoplasma, chlamydia or whooping cough, it is recommended to prescribe antibacterial therapy with drugs from the macrolide group (josamycin, azithromycin, clarithromycin) [17]. If necessary, nebulizer therapy is carried out.
Antibacterial therapy is prescribed more actively if we are talking about risk groups:
- patients over 75 years of age with high fever;
- patients with concomitant severe chronic pathology (diabetes mellitus, heart failure, COPD);
- patients receiving immunosuppressive therapy;
- patients with alcohol dependence.
These people have an immunosuppressed state to begin with, so the risk of developing complications is higher than in the general population. If a decision is made about the need for antibiotic therapy, the starting antibiotic is usually amoxicillin [18].
Stenosis of the trachea and bronchi
2902 19 July
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Stenosis of the trachea and bronchi: causes, symptoms, diagnosis and treatment methods.
Definition
Stenosis of the trachea and bronchi is a narrowing of the lumen of the trachea and/or bronchi as a result of the replacement of normal wall structures with coarse scar tissue, leading to the destruction of cartilaginous rings and disruption of their frame function.
Causes of tracheal and bronchial stenosis
The trachea is a tube that connects the larynx to the bronchi. Its main function is to conduct air into the lungs. The trachea consists of 18-22 cartilaginous rings, thanks to which its lumen is maintained. The main bronchi (right and left) depart from it and go almost at right angles to the gate of the corresponding lung.
The number of patients with tracheal and bronchial stenosis in the world is constantly increasing. This is due to the increasing number of tracheal intubations for mechanical ventilation during complex surgical procedures or for the treatment of severe respiratory distress in intensive care units.
Mechanical damage to the mucous membrane of the trachea by an endotracheal tube and prolonged compression of the blood vessels supplying it lead to inflammatory processes in the wall with subsequent formation of connective tissue.
The cartilaginous basis of the tracheal wall frame loses its function, and a narrowing of the airway lumen develops. The topographic-anatomical relationship of nearby organs and tissues changes, which negatively affects the processes of blood circulation and respiration.
Some diseases can lead to narrowing of the trachea and bronchi. One of them is amyloidosis, a rare systemic disease in which intercellular deposition of homogeneous protein masses occurs in all organs and tissues of the body without exception. The accumulation of amyloid in the proximal (extrathoracic) part of the trachea causes clinical stenosis of the upper respiratory tract of varying severity, which often requires surgical expansion of the lumen or tracheostomy.
Wegener's granulomatosis is another rare systemic disease of unknown etiology, which is characterized by granulomatous-necrotizing systemic vasculitis, involving the upper and lower respiratory tract, lungs, and kidneys. Ulcerative-necrotic changes in the mucous membrane of the pharynx, larynx, and trachea develop. Surgical treatment for Wegener's granulomatosis is carried out for health reasons, since postoperative wounds during open surgical interventions can take a very long time to heal.
Osteochondroplastic tracheobronchopathy most often affects the middle and lower thirds of the trachea and bronchi. The cause of osteochondroplastic tracheobronchopathy remains unclear (congenital origin, chronic bronchitis, specific inflammatory process (tuberculosis, syphilis), etc.). In the submucosal layer of the trachea and bronchi, growths of spongy bone and/or cartilage appear between the tracheal rings. The trachea and large bronchi turn into hard, rigid tubes, approaching the density of bone tissue. Dense whitish tubercles along the cartilaginous rings can hang into the lumen of the trachea and bronchi like stalactites. The lumen of the trachea narrows and becomes deformed.
Tuberculosis of the trachea and bronchi is most often a complication of pulmonary tuberculosis and only in very rare cases - an independent disease. The process begins with the formation of an infiltrate in the mucous membrane. Scarring in the large bronchi leads to their narrowing and can cause atelectasis (collapse of lung tissue).
Congenital causes of tracheal and/or bronchial stenosis may be an abnormal development of the tracheal and/or bronchial wall; double arch of the aorta, compressing the lumen of the trachea.
The causes of tracheobronchial stenosis can be transplantation of one or two lungs, the “lung-heart” complex; closed and open damage; respiratory tract burns; chronic infectious inflammatory processes of the trachea and large bronchi; malignant tumors of the lungs, esophagus and mediastinum.
Rare causes include Crohn's disease, relapsing polychondritis, sarcoidosis, fibrosing mediastinitis, and gastroesophageal reflux.
Classification of the disease
Due to its occurrence:
- congenital stenoses;
- acquired stenoses:
- posttracheostomy,
- postintubation,
- post-traumatic,
- idiopathic.
According to the degree of narrowing of the airway lumen:
1st degree - narrowing by less than 1/3 of the tracheal diameter (“scar deformity” - physiologically insignificant, treatment is not required); 2nd degree – narrowing from 1/3 to 1/2 of the diameter of the trachea (manifests itself with significant physical activity, treatment, as a rule, is not required); 3rd degree – from 1/2 to 2/3 of the diameter (treatment required); 4th degree - narrowing by more than 2/3 of the lumen diameter (emergency assistance is required, as it poses a threat to life).
According to the length of the lesion:
1st degree - limited stenosis (less than 15% of the entire length of the trachea); 2nd degree - moderate stenosis (from 15% to 30%); 3rd degree - extensive stenosis (from 30% to 60%); 4th degree – widespread stenosis (more than 60%).
Symptoms of tracheal and bronchial stenosis
The main clinical manifestation of tracheobronchial stenosis is difficulty breathing - from shortness of breath during exercise to stridor (wheezing noisy breathing caused by turbulent air flow in the respiratory tract) at rest.
Patients may experience cough, hemoptysis, and difficulty swallowing. Dysphonia is manifested by nasality, hoarseness, and hoarseness of the voice. Patients indicate previous trauma, surgery on the neck organs, and prolonged stay on mechanical ventilation.
The patient's condition depends on the degree of stenosis of the trachea and/or bronchi.
Diagnosis of tracheal and bronchial stenosis
To assess the severity of airway obstructions and the dynamics of the development of the process, various research methods are used:
- spirography is a method for studying the function of external respiration, including measurement of volume and speed parameters of breathing;
- spirography with pharmaceutical samples - measurement of lung volume against the background of exposure to special pharmacological drugs for diagnosing respiratory pathologies;