This disease, caused by 25 types of bacteria, is also called radiant fungus. The disease is one of the chronic inflammatory processes observed in humans and animals. Many people, having noticed pustules on themselves, do not even suspect that they have become victims of deadly bacteria.
COST OF SOME GYNECOLOGIST SERVICES IN OUR CLINIC IN ST. PETERSBURG
| Price for a dermatologist appointment | 1000 rub. |
| Extended colposcopy | 1300 rub. |
| Ultrasound of the pelvis (all organs) | 1300 rub. |
| Call free: 8-800-707-1560 *The clinic is licensed to provide these services | |
Epidemiology of the disease
Actinomycosis is widespread. It affects both people and farm animals. Men get sick 2 times more often than women. Children rarely get sick. There have been no cases of transmission of infection from a sick person or animal.
Reservoir and source of infection
Actinomycetes are widespread. They are found in water, soil, straw, hay and dry grass and on cereals. Radiant fungi as saprophytes live in the human oral cavity, carious cavities, on the surface of the tonsils, bronchial mucosa and digestive system, including the rectum.
Mechanism of infection
- During exogenous infection, actinomycetes enter the human body through household contact, airborne droplets and airborne dust through mucous membranes, injured areas of the skin with dust, soil or plant parts. Allergic and paraallergic reactions, concomitant diseases, damage to the skin and mucous membranes of traumatic origin, acne, sycosis, hidradenitis suppurativa, etc. also contribute to the development of the disease.
- But most often actinomycosis develops as a result of self-infection or through metastasis, when a saprophytic infection of the oral cavity, gastrointestinal tract and respiratory tract acquires pathogenic properties when the immune system is weakened.
- The development of the disease is facilitated by frequent acute respiratory infections and concomitant diseases leading to the development of immunodeficiency, allergic and paraallergic reactions, pregnancy, surgical interventions, anatomical anomalies, injuries, bruises and wounds, acne, sycosis, hidradenitis suppurativa, etc.
Rice. 2. Accumulations of actinomycetes in tissues.
How do you get actinomycosis?
Radiant fungus is very common in nature: it is found in water, air and soil. The main breeding grounds for infection are rotting straw, hay and manure. Fungal spores penetrate into arable soil and from there into growing crops. The most common infection of humans and animals occurs through cereals.
The spores penetrate the skin or, when ingested, into the mucous membranes of the mouth, pharynx, esophagus or intestines. The respiratory tract is also easily affected. Transmitters of infection in addition to straw and hay, milk, flour, soil, etc.
It is also possible to become infected from a sick animal, but such cases are rare. Among domestic animals, actinomycosis most often affects cattle, horses, pigs, goats, and dogs and cats can also be infected.
What is important is that the infection can penetrate through intact skin.
In humans, actinomycosis is observed mainly in residents of rural areas, and in men more often than in women. The main age of patients is 20-40 years, although children are also affected. Dermatologists note that a common cause of actinomycosis infection is the habit of chewing ears of grain picked in the field. Elements of the ear have been repeatedly found in actinomycotic foci.
The incubation period varies, in some cases it lasts only a few weeks, in others it lasts several years.
Actinomycetes: morphology
Actinomycosis is caused by microorganisms of the genus Actinomyces. Previously, pathogens were regarded as fungi, now - as bacteria. The disease they cause is called pseudomycosis. There are several types of actinomycetes that are pathogenic for humans and animals: A. bovis (type species), A. israelii (the most common causative agent of pseudomycosis in humans), A. odontolyticus, A. naeslundii, A. viscosus, etc.
- Aerobic actinomycetes: live in soil, found in water, air and on cereals.
- Anaerobic actinomycetes: are saprophytes. They live on the mucous membranes of humans and animals. They are most pathogenic.
Rice. 3. Threads of mycelium of actinomycetes (photo on the left) and accumulations of Actinomyces Israelii in tissues (photo on the right).
Morphological characteristics of pathogenic actinomycetes
The growth of pathogens located in the tissues of granulomas and exudates is accompanied by the formation of intertwined threads of mycelium - drusen, which are located radially along the periphery (in the form of rays) and have club-shaped thickenings at the ends.
These formations in the pathological material have the appearance of small grains (lumps) of a yellowish or gray color ranging from 20 to 250 microns in size (depending on the age of the colonies).
- Microscopy reveals an accumulation of filaments of actinomycete mycelium in the center of the drusen, and flask-shaped swellings along the periphery.
- When histological material is stained with hematoxylin and eosin, the central part is colored blue, and the flask-shaped thickenings are colored pink. Sometimes there are drusen without flask-shaped thickenings along the periphery. In some cases, drusen do not form.
Actinomycetes occupy an intermediate position between bacteria and fungi. They have a cell wall, like gram-positive bacteria, but, unlike them, they contain sugars. They do not contain chitin or cellulose, are incapable of photosynthesis, do not have flagella, do not form spores, form primitive mycelium, and are not acid-resistant.
Rice. 4. Type of drusen of pathogenic actinomycetes.
Rice. 5. The photo shows densely packed filaments of mycelium of pathogenic actinomycetes.
Cultural characteristics of pathogens
For their growth, actinomycetes require anaerobic conditions (without oxygen). Grows well on protein media. When growing on solid nutrient media, by the end of the first day they form transparent microcolonies, after 7 - 14 days - lumpy colonies that have grown into the nutrient medium, resembling molars in appearance.
Rice. 6. Colonies of actinomycetes on chocolate agar.
Stability and sensitivity of pathogens
Actinomycetes exhibit resistance to desiccation and persist for 1–2 years at low temperatures.
Pathogens are sensitive to high temperatures of 70 - 800 C and die within 5 minutes. Within 5 - 7 minutes they die when exposed to a 3% formaldehyde solution. Sensitive to antibacterial drugs: benzylpenicillin, streptomycin, chloramphenicol, tetracycline, erythromycin, etc.
Rice. 7. Type of colonies of Actinomyces Israelii, the most common causative agent of pseudomycosis in humans.
How does infection occur and what are the symptoms of the disease?
If the fungus enters through a wound on the skin, an infiltrate with a board-like density develops in its tissue. The initial bluish tint gives way to bright red. The patient has a symptom of fluctuation: in the center of the affected area there is softened tissue, the process of necrosis is directed towards the edges. A granuloma is a collection of fungal colonies (drusen).
The infiltrate can grow in the form of fistulas, choosing the path through the subcutaneous fat. Blood vessels are subjected to enormous stress at the moment when granulomas melt. The disease can transform into a generalized form when the walls of the vessels are destroyed and the contents of the fistulas enter the blood.
A fungal infection can be joined by a bacterial one, which can lead to the formation of abscesses and/or phlegmon.
The patient exhibits symptoms:
- High body temperature.
- Excessive sweating at night.
- The surface of the skin turns pale. Gray color appears with abscesses and pleurisy.
- Dyspnea.
- Acrocyanosis caused by tissue hypoxia due to restriction of the respiratory surface of the lungs.
- The nail plate becomes convex (symptom of “clock hands”).
- The tips of the fingers thicken (“drumsticks”).
- The appearance of fistula tracts.
- Exhaustion of the body.
If excessive weakness is observed, foci of the disease come out in the form of fistulas, other organs are affected, these signs indicate the transition of the disease to a chronic form.
A severe form of actinomycosis is accompanied by metastases spreading to other organs. Sometimes the patient has only 1-2 years to live and faces death. Some patients live up to 5 years.
A complete cure is likely only with mild severity.
This type of disease in children most often manifests itself on the tonsils, and at an age when permanent teeth have already grown. It is dental plaque that contains radiant fungus.
Actinomycosis of bones also occurs, but it affects only adult patients.
How the disease develops
Actinomycetes are saprophytes. They are part of the normal microflora of the skin and mucous membranes of humans and animals. Some strains of pathogens, under certain conditions, acquire pathogenic properties and are capable of causing disease (endogenous pathway). In some cases, actinomycetes enter the body through damaged areas of the skin and mucous membranes (exogenous route).
When pathogens invade soft tissues, infectious granulomas are formed, in which accumulations of mycelium of radiant fungi - drusen - are found. Over time, as a result of infection with staphylococci (most often), abscesses develop in the granulations, and when they break through, fistulas are formed. Further, the pathogens, thanks to the production of aggressive enzymes, spread through the subcutaneous tissue, through the bloodstream and through the lymphatic vessels into tissues with a low oxygen content.
As a result of infection, specific sensitization and allergic changes develop in the patient’s body, which leads to the formation of antibodies.
Rice. 8. When actinomycetes invade soft tissues, an infectious granuloma is formed (photo on the left), where accumulations of mycelium of radiant fungi - drusen (photo on the right) are found.
Classification of the disease
Fungal pathology can take various forms of clinical picture depending on the location:
- Maxillofacial.
- Fungal infection of the tonsils.
- Lungs.
- Abdominal.
- Genitourinary system.
- Bones and joints.
- Pathological effects of actinomycetes on the skin.
If there are injuries on the oral mucosa, this serves as an active migration of saprophytic radiant fungi - a maxillofacial lesion develops. The development of infection follows the same principle as in other places: a red-bluish granuloma in the form of a flat disk degenerates into a fistula. Typically, the granuloma is located in the angle of the lower jaw. The inflammatory process gains activity gradually. The patient experiences discomfort, he feels pain and the presence of something foreign in his mouth. Body temperature remains almost unchanged, sometimes rising slightly. Actinomycetes can infect the jaw periosteum, the space between the muscles. The lesion process can penetrate the skin of the neck and face. Often a spasm of the masticatory muscles occurs if they are affected by a lesion.
The photo shows maxillofacial actinomycosis:
Maxillofacial actinomycosis
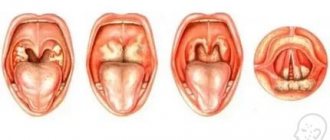
When infection activates in the tonsils, tonsillitis occurs, which takes a chronic form.
With a thoracic illness, the patient develops a wet cough. If blood is observed in the sputum, it means that the melting of the lung tissue has reached the stage of vascular damage. This condition of the patient is accompanied by moist single wheezing. When the type of breathing is amphoric, this indicates the appearance of a cavity in the lungs.
Breathing sounds at the very beginning of the lesion are somewhat dull. A sympathetic hue signals the formation of cavities. When the doctor palpates the chest, and an increase in voice tremors is observed, it means that infiltrates have arisen in the lungs.
The consequence of the growth of the granuloma, which is directed from the middle of the lung to the edges, is the formation of adhesions between the layers of the pleura.
Pain syndrome appears when inflammation affects the layers of the pleura. If the patient lies down, turning to the painful side, he thereby fixes the body, the pain subsides a little.
If lung treatment is not started in time, death cannot be ruled out.
Abdominal form - damage to the appendix area. Often, not only the appendage, but also the ileocecal region is affected by pathology. The person is given a preliminary diagnosis: appendicitis or intestinal obstruction. Actinomycetes enter the large intestine, stomach or through an overgrown granuloma through the blood. Sometimes the peritoneal wall is also involved. Metastases grow into the spine, liver, kidneys. Paraproctitis occurs if the fistulous tracts reach the perianal area and open into the intestinal lumen. This form of the disease is also deadly in the absence of medical care.
Actinomycosis of the genitourinary system acts as a secondary infection, provoked by the activity of the primary focus.
Bones and joints are exposed to the activity of radiant fungus when granuloma from neighboring organs grows or is carried with the blood into the bone tissue. The patient is diagnosed with osteomyelitis, accompanied by the occurrence of bone sequestration. The patient does not lose joint mobility for a fairly long period of time. A distinctive feature is the bluish tint of the edging of the fistula.
Skin damage by actinomycetes occurs as a result of generalization of the inflammatory process. Symptoms become obvious when the granuloma penetrates the subcutaneous fat.
Madura foot is a type of skin pathology, most often found in the tropics. Pea-sized nodules appear on the foot, and the skin becomes purple-purple. New nodules are joined to the primary ones, the foot swells, and its shape is distorted. The next stage is characterized by the formation of fistula tracts filled with ichor and pus. Fistulas open on all sides of the foot, which leads to deformation of the toes, which are directed upward. At the most severe stage, even the muscles of the lower leg and tendons are involved in the inflammatory process.
In the photo there is a Madura foot:
Madura foot
Symptoms of actinomycosis
The disease affects various organs and tissues, but the most common is actinomycosis of the maxillofacial region and abdominal organs. Less common are thoracic actinomycosis, lesions of the oral and nasal cavity, tongue, tonsils, genitourinary organs, central nervous system, mycetoma or Madura foot, etc.
The disease is characterized by a varied clinical picture, which is associated with numerous localizations of lesions and a long progressive course. The incubation period ranges from 2 weeks to several months and even years.
- With each form, a mildly painful infiltrate develops, which softens over time.
- Despite anatomical barriers, inflammation steadily spreads to surrounding tissues.
- Abscess formation (suppuration) gradually occurs and fistulas form. The fistula tracts are tortuous, filled with granulations and pus. The mouths of the fistulas are retracted, forming roller-like folds. Their color turns purple-blue. Discharge from fistulas is odorless.
- In the discharged purulent masses a large number of drusen pathogens in the form of granules are found. Yellowish or white granules 2 - 3 mm in diameter.
- The infiltrate wall thickens over time, giving it a characteristic woody consistency. The fistulas gradually scar.
- The pain syndrome is not expressed.
Rice. 9. Many fistulas are a characteristic feature of actinomycosis.
Treatment of fungal disease
The treatment course involves taking etiotropic medications and surgical intervention.
When prescribing antibiotics, the doctor must take into account the spectrum of their effects in order to destroy not only actinomycetes, but also other bacteria that could penetrate and settle in the pathogenic flora. Often this moment is very difficult, especially when the microflora becomes antibiotic-resistant.
Depending on the location of the colonies, a special treatment program is developed.
Maxillofacial pathology is treated with antibiotics of the penicillin group with clavulanic acid (Flemoklav, Amoxiclav). The first cycle lasts one week, the dose contains 2.4 mg three times a day. The dosage is gradually reduced, and the second cycle extends treatment for another 1 week. The same method is used to treat neck disease.
Infection of the lungs with radiant fungus takes longer: from 3 weeks to 1 month. Parenteral administration of drugs is used. If the stage is advanced, combinations of different antibacterial agents are prescribed.
If there are concomitant anaerobic bacteria, carbapenem antibiotics will be needed. Antifungal drugs are indicated in combination with other medications: Diflucan, Lamisil, Orungal, Nizoral.
During treatment, when the patient takes such radical drugs as antibiotics, therapy that strengthens the immune system is necessary. Among the most effective is Actinolysate, which improves the quality of phagocytosis (cellular immunity). This drug is prescribed for any form and stage of the disease. 3 ml is administered intramuscularly three times a week at regular intervals.
Antihistamines: Suprastin, Tavegil and Diazolin provide desensitizing therapy.
Sometimes additional medications are prescribed, for example, potassium iodide, which enhances the etiotropic effect.
Autohepotherapy is used as an immune stimulant, and Aloe extract is used intramuscularly to relieve inflammation.
Ointments with antifungal and antibiotic components promote wound healing, especially after surgical operations to remove fistulas.
Electrophoresis consolidates the effect obtained from drug treatment. Ultrasound is also recommended: daily, from 12 to 25 sessions.
In the photo, actinomycosis accompanied by the formation of a fistula:
Actinomycosis accompanied by fistula formation
Surgical treatment is carried out in individual cases, which are considered individually for each patient. If the operation leaves noticeable consequences, dermoplasty is performed.
For actinomycosis of the lung, resection of the affected part of the respiratory organ is performed, and adhesions are also removed.
Actinomycosis of the maxillofacial region
Among all forms of the disease, actinomycosis of the face accounts for from 55 to 60%, among all inflammatory lesions of the face and lower jaw - from 6 to 10%. The disease lasts a long time and is often complicated by bacterial infections. The disease affects the skin of the cheeks, muscles, lips, tonsils, tongue, salivary glands, larynx, trachea, orbital area and lymph nodes.
Actinomycetes penetrate into the tissues of the maxillofacial region through the mucous membrane of the oral cavity. However, it is rarely initially affected - only in 2% of cases. The process often spreads from carious teeth, gums, through the nasal mucosa, from the sinuses and tonsils, as well as through the bloodstream and lymphogenous route.
The appearance of a lesion is recorded only when the inflammatory infiltrate of the subcutaneous tissue reaches and fistulas form. A tumor-like formation or dense infiltrate most often appears in the area of the angle of the lower jaw, less often localized on the cheek, the anterior surface of the neck and chin. The lesion has a lumpy appearance due to the presence of multiple very dense infiltrates, each of which has a fistulous tract, from which purulent masses with small inclusions in the form of grains of grayish or yellowish color are released, which are drusen of actinomycetes. The pain syndrome is not expressed. Sometimes the patient has a low fever. The disease lasts for many months, but is relatively milder than with other forms of the disease. Lymphogenous spread of infection is not observed.
Actinomycosis of the bones of the lower jaw, simulating a tumor and banal osteomyelitis, is very rarely recorded.
Rice. 10. Actinomycosis of the maxillofacial region.
Rice. 11. Actinomycosis of the face.
What is actinomycosis
The content of the article
Actinomycosis is a subacute chronic bacterial infection caused by filamentous, gram-positive, non-acidic, anaerobic and microaerophilic bacteria. The disease is characterized by purulent and granulomatous inflammation and the formation of multiple abscesses and sinus tracts that may secrete sulfur granules.
The most common clinical forms of actinomycosis are cervicofacial (jaw), thoracic and abdominal. In women, pelvic actinomycosis is possible.
Actinomycosis of the skin
The cutaneous form of actinomycosis is rare. The disease affects the skin on the face, neck, hands and feet. The appearance of a lesion is recorded only when the inflammatory infiltrate of the subcutaneous tissue reaches and fistulas form.
The pathological process has varying degrees of severity. The following forms of the disease are distinguished:
- Skin (gummous, abscessive and mixed).
- Subcutaneous.
- Deep (muscular).
The gummous form is the most common. The disease is characterized by the appearance of a woody density of infiltrates (nodes) under the skin, which is why they have a lumpy appearance. The skin in the affected area acquires a purple tint. In some places, the lesions soften and fistulas form, which open and close on their own. From them, scanty purulent masses of a crumbly consistency with small (up to 1 mm) inclusions in the form of grains of grayish or yellowish color, representing drusen of actinomycetes, are released. The pain syndrome is not expressed.
The abscess form of actinomycosis is characterized by rapid suppuration and ulceration of infiltrated tubercles. A large amount of purulent discharge is released from the fistula tracts. The lesion occurs as a cold abscess. Patients have moderately severe intoxication.
In some cases, the infectious process spreads to deep-lying tissues. When they are destroyed, ulcers with undermined edges and granulations form, covering the bottom. The granulations contain many drusen of actinomycetes. When such lesions heal, uneven bridge-shaped scars are formed, tightly fused to the underlying tissues. The course of the disease is long and sluggish. If the outcome is favorable, a keloid is formed at the site of the node.
The muscular form of actinomycosis is characterized by the appearance of lesions in the muscle tissue (usually the masticatory muscles in the area of the angle of the lower jaw) under the fascia covering them. The pathological process develops over 1 to 3 months. Infiltrates are dense, cartilaginous consistency. The face becomes asymmetrical. Trismus develops. When suppuration occurs, fistula tracts are formed, from which purulent-bloody fluid mixed with drusen of actinomycetes is released. The skin around the fistulas retains a bluish color for a long time. When the lesions are localized on the neck, the changes take the form of transversely located ridges. The cavities formed after the rejection of purulent masses are filled with granulation tissue over time.
The pathological process can spread to the periosteum and bone. The lesion occurs as cortical osteomyelitis.
The mixed form of actinomycosis is characterized by the appearance of gummous formations and abscesses.
Rice. 12. Damage to the submandibular region and cheek area due to actinomycosis.
Rice. 13. When the lesions are localized on the neck, the changes take the form of transversely located ridges.
Rice. 14. Actinomycosis of the trunk and limbs.
How to diagnose the disease?
To determine the type of disease in question, diagnostics are carried out using various methods. It is very important to differentiate changes similar to tuberculosis detected by x-ray.
A blood test provides valuable information about the presence of an inflammatory process and sensitization of the body. Against the background of weakened immunity, leukopenia may develop, which is expressed by toxic granularity in red blood cells.
The disease in question is characterized by microabscesses, as a result of which the skin becomes cellular in structure. Condensed subcutaneous metastases, fistula tracts through which pus is released, paint a clear clinical picture characteristic of the disease being sought.
Carrying out puncturing allows us to study the composition of the contents of fistulas. Sputum cultures are performed to determine the type of fungus. For a better visual examination, the laboratory assistant takes a transparent medium. After an incubation period of 2-4 days, arachnid colonies form. On days 10-14, typical colonies appear (striated, smooth, rough, curved), thread-like mycelium is visible on them. Radiant fungus can create pigmentation, so colonies can be greenish, gray and crimson.
When clusters of colonies are detected, a presumptive diagnosis is made. Next, the type of fungus is determined. By the way, for a more accurate diagnosis, smears are taken from the fistula tracts, because in places such as carious teeth, gums, tonsils, a healthy person can also have fungus.
An actinolizer sample taken from subcutaneous tissue will also help establish the correct diagnosis. A negative result means that the patient has an advanced stage of the disease.
For diagnostic purposes, the following procedure is performed: 0.3 ml of antigen (lysed actinomycete) is injected subcutaneously into the forearm. If exactly 24 hours later erythema appears in that place, then it is possible to ascertain the presence of actinomycosis.
This diagnosis is also confirmed if, upon microscopic examination, radiant fungi, similar to grains, are visible in the sputum secreted by a fistula open into the bronchial lumen.
Computed tomography is not necessary to establish a diagnosis; this type of examination is necessary to monitor changes in the affected areas during therapy.
Also, with the help of ultrasound, only signs of an inhomogeneous structure can be detected, which may raise suspicion of actinomycosis.
Abdominal actinomycosis
Abdominal actinomycosis is the second most common among all forms of the disease and accounts for 25 - 30%. The primary focus is most often localized in the cecum and appendix. The disease develops with perforation of the stomach or intestines, ulcerative lesions, diverticulitis, trauma (bone damage, knife or gunshot wounds) and surgical interventions. The small intestine and rectum are affected, and very rarely the esophagus and stomach. The abdominal wall is affected secondarily.
The disease begins gradually with fever and malaise, abdominal discomfort, constipation or diarrhea. The diagnosis is difficult to establish. This takes months and even years.
On palpation, a mass formation can be detected. When an abscess is opened, drusen of actinomycetes are found in large quantities in the purulent discharge.
Abdominal actinomycosis must be distinguished from Crohn's disease, malignant tumors, abscesses, amebiasis, tuberculosis, etc. The diagnosis is established on the basis of biopsy data.
When the abdominal wall is damaged, specific skin changes occur. Fistulas are most often located in the groin area.
As the disease progresses, the rectum, diaphragm, liver, kidneys, genitourinary organs and spine are involved in the pathological process:
- When the rectum is damaged, paraproctitis develops. Fistulas appear in the perianal area. In the absence of adequate treatment, mortality reaches 50%.
- Damage to the genitourinary organs is rarely recorded. The infectious process spreads from the primary foci of actinomycosis located in the abdominal cavity.
- Actinomycosis of the genital organs is extremely rare.
- In 5% of cases the liver is affected. Actinomycetes most often penetrate the organ directly.
- The kidneys are rarely affected. The infection spreads from abscesses located in the abdominal cavity or lesser groove.
Fistulas arising from actinomycosis, despite excision and drainage, reappear.
Rice. 15. Actinomycosis of the abdominal cavity.
Pathological anatomy
Pathological changes in actinomycosis are different in humans and animals. In the bull, hyperplasia of the affected tissues predominates, and a voluminous tumor of a whitish-grayish color is formed, containing in places small pockets of softening; characteristic yellow grains are sometimes found in these nests; the lesion gradually spreads to muscles, bones, fiber and even blood vessels, like cancerous tumors. Under a microscope, the picture resembles embryonal sarcoma.
In humans, the process of suppuration mainly predominates, reminiscent of the development of abscesses and phlegmon and, due to the multiplicity of nests, giving a picture of chronic pyaemia. In humans, the body's reaction is also detected by the accumulation of small embryonic cells and the formation of granulation tissue, which acquires a special appearance due to the early fatty degeneration of cellular elements and secondary purulent softening of the nests. In fungous growths on the walls of the abscess, some wandering elements take the form of epithelial cells, while others take the form of giant cells. The latter may contain parasites. The fungus is also found in leukocytes. If these cells have sufficient viability, they destroy the parasites; otherwise, when the parasite takes over, the latter multiplies, goes beyond the boundaries of the collapsing cell and begins to fight with new cells. Parasites that have undergone degeneration appear to form hyaline bodies, similar to rhinoscleroma bodies.
Pathological changes in actinomycosis occur in all tissues and in all parts of the body. However, the disease usually retains the character of a local disease, but the tendency to spread and the method of this spread are different in different cases.
Lymphatic glands are rarely affected, and where this happens, their damage is caused by additional secondary infections. Blood poisoning, on the contrary, possibly leads to general forms of the disease with the formation of metastases in many organs. The mechanism of occurrence of such forms of the disease is easy to understand in cases where actinomitotic masses appear in the cavities of the heart or in large vessels of the neck.
The most common way the disease spreads is through gradual tissue damage and non-stop and unimpeded progression of the process. Thus, a painful focus that initially appears in the pharynx or lower jaw can successively capture the neck area, go down along the spine, spread to the mediastinum, pleura and lungs, descend into the abdominal cavity and even lower, appear on the upper thigh and in the inguinal triangle; in this case, secondary foci are formed along the way, which can open on the skin or in the internal organs with many fistulous openings. In other cases, the process spreads upward and suppuration passes through the vessels into the cranial cavity, affecting the brain and meninges.
Actinomycosis inflammation affects all tissues, aponeuroses, muscles, bones, nerves or blood vessels; fistulous tracts are formed in them, containing serous, liquid, often bloody and foul-smelling pus, in which there are characteristic grains. The walls of abscesses or fistulous tracts resemble the walls of cold tuberculous abscesses; here fungoous masses of a gray-yellowish or reddish color develop, very brittle, but still less bleeding than with tuberculosis. These changes differ from tuberculosis mainly in the woody hardness of the surrounding zone of chronic inflammation, which consists of layers of infiltrated and very dense connective tissue. More or less extensive scars also form in places; fungous or callose masses are absorbed, leaving behind a thin strand of fibrous tissue.
However, the changes have a different appearance, depending on the affected tissue. The bones become spongy, brittle and furrowed cavities, which are filled with convolutions of pus and contain mobile sequestra or gelatinous masses resembling raspberries; these cavities lead to the formation of fistula tracts, which fester severely. In the joints, the articular surfaces and ligaments are corroded and destroyed. If the spinal column is affected, then the vertebral bodies are exposed, their surface is corroded, becomes as if chewed out, the intervertebral circles disappear in places, and everything is covered with thick pus, which raises thickened fibrous tissue in front of the spine.
The lungs can be affected either by continuation, due to the spread of the process from the mediastinum or costal walls, or primarily, or, finally, due to embolism. Bronchopneumonic foci are then found in them in the form of miliary nodules around the bronchi or in the form of more voluminous nodes the size of a cherry or an apple.
These changes consist in the accumulation of small cells, which quickly undergo fatty degeneration and purulent melting and lead to the formation of purulent cavities, sometimes becoming very large. Scar tissue forms around the circumference, turning large areas of the lung into a dense, compact mass. This chronic inflammatory process extends to the pleura and mediastinum and can cause severe disfigurement of the chest. Sometimes an effusion forms in the pleura, which is sometimes serous, sometimes purulent and fetid. Abscesses descend into the mediastinum, along the spine and under the costal pleura; all these purulent cavities, interconnected by fistulous tracts, are in communication with the bronchi and open on the outer integument with numerous holes, or pierce the thoraco-abdominal barrier and pour into the abdominal cavity.
In the digestive apparatus, changes predominate in the first pathways. The esophagus is sometimes an entry point for infection: when opened, fistula tracts were found in it, which served as a connection between its cavity and between the abscess lying in front of the spine.
In the intestines, only the mucous membrane can be affected. At autopsy, they may find the inner surface of the small intestines dotted with round or oblong whitish plaques, 4 to 5 millimeters thick and 1 centimeter wide: such plaques mostly consist of colonies of a radiant fungus, the threads of which fill the cavity of the Lieberkühn glands. In other cases, lenticular abscesses are observed that can heal spontaneously. Sometimes the changes are more profound: a diffuse infiltration of some part of the intestine with multiple purulent small foci is formed. The affected loop, thanks to adhesions, is attached to neighboring loops, to the abdominal wall and to the internal organs; in the intervals, abscesses of various volumes, foci of encysted peritonitis are formed, which can open into the intestinal cavity or on the skin, descend into the iliac cavities, into the pelvis, etc. Such changes are especially often observed around the cecum and represent a type of actinomycotic peritiphlitis; they are also found around the rectum.
Sometimes a purulent focus receives communication with the bladder, and yellow grains are found in the urine, or purulent foci form around the uterus, ovaries, or prostate gland.
In the liver, either more or less limited foci of metastatic origin or extensive nests of softened, grayish or dirty-gray tissue with black dots are formed; Thick and bloody pus flows from these nests.
In cases where blood poisoning occurs, embolic foci can be found in all organs, in the lungs, in the liver, in the spleen, in the adrenal capsules, in the testicles, in the muscles, etc. Such foci resemble pyeemic abscesses.
Nerve centers may also be subject to specific emboli; There may be cases of abscesses appearing at the site of the gyri and in the depths of the white matter. Sometimes changes in the neck, pharynx or lower jaws subsequently spread to the meninges, temporal and parietal gyri after perforation of the base of the skull.
As rarer pathological forms, it remains to be noted those cases when in humans changes are found in the form of a tumor or neoplasm (limited neoplasm) and, therefore, more closely resemble actinomycosis, characteristic of cattle.
In addition to these changes, directly caused by the influence of parasites on tissues, amyloid degeneration of internal organs is often observed if the disease, with a longer course, is detected by suppuration of bones or multiple and prolonged suppuration of internal organs.
Thoracic actinomycosis
Thoracic actinomycosis is the third most common among all forms of the disease and ranges from 10 to 20%. Most often the lungs and pleura are affected, less often - soft tissues. Actinomycosis of the mediastinum develops rarely.
The routes of damage are both primary and secondary. With a primary lesion, the infection spreads with secretions from the nasopharynx, with a secondary lesion - from foci located in the face, neck and abdominal organs. With hematogenous dissemination, mortality from the disease reaches 50%.
Thoracic actinomycosis develops gradually. Initially, low-grade body temperature and weakness appear. Next is a dry cough, then with sputum, often tasting of honey and smelling of earth. The disease lasts for a long time under the mask of bronchitis, pneumonia and pleurisy. The infiltrate spreads towards the periphery, affecting the pleura, chest wall and skin, which acquires a purple-bluish color. When palpating the swelling, severe burning pain appears. When the infiltrate suppurates, fistulas are formed. The purulent contents contain large quantities of drusen pathogens. Fistulas often communicate with the bronchi. The disease is difficult. Without adequate treatment, patients die.
Thoracic actinomycosis should be distinguished from nocardiosis, tuberculosis, pneumoconiosis and lung cancer.
Rice. 16. Thoracic form of actinomycosis.
Symptoms and clinical forms
Varied localization, the tendency of the process to spread and move from one area to another and, consequently, the participation of a large number of organs make it impossible to general describe the symptoms of actinomycosis and make it difficult to separate into separate clinical forms. However, since in the vast majority of cases actinomycosis occurs in the form of a local lesion, and the localization depends on the entrance gate, it is easiest and more consistent to describe these various localizations in turn, each of them constituting a separate form.
Actinomycosis of the face and neck
Quite often, the onset of actinomycosis is detected at the site of a damaged tooth or after it is pulled out. An abscess develops on the gum, which at first is nothing special; after opening it, a fistula is formed, and the abscess takes on the character of a cold abscess. In other cases, the development of the disease from the very beginning is slow and torpid; A hard, flat, painless nodule appears, which often sits on the inner surface of the lower jaw or at its posterior corner, and in the center of which, after a more or less long time, a false ripple appears, depending more on the presence of fungal tissues than on the accumulation of pus. The skin turns red, acquires a bluish-pale color, merges with the tumor, which opens with one or more fistulous openings; from the latter flows serous or viscous, liquid pus with convolutions, in which the presence of yellow granules can be discovered either directly or subsequently. These abscesses are characterized by the extreme density of the inflammatory zone surrounding them; it seems as if the abscess is actually sitting in the tumor. Such a lesion may then remain in a stationary state, with periods of improvement alternating with frequent relapses; Spontaneous healing may even occur, although this is rare; most often, neighboring parts are gradually affected. Thus, many very complex cavities are formed, communicating with each other and with the main focus through tortuous passages and simultaneously opening on the skin (in the submandibular region and on the neck) and in the oral cavity. The fistula openings are bordered by yellowish-bluish unstable fungal granulations. In depth, the tumor fuses with bones, which can become disfigured and also become damaged. The process moves further to the muscles, so that when the masticatory muscle is damaged, signs of trismus occur. The tumor protrudes into the mouth, causes tooth loss, pushes back the tongue and interferes with chewing and swallowing. At the same time, severe pain rarely occurs; Most often, pain is observed only with pressure. For a long time, sometimes for months at a time, there is no fever or any general symptoms.
In this situation, actinomycosis drags on for months and years with a persistence that leads to despair. However, the matter may not be limited to the primarily affected area; gradually the process progresses, like an abscess, descends along the neck along the pharynx, exfoliating the prevertebral fibrous tissue, exposing and necrotizing the vertebrae. It thus passes into the chest cavity and can also penetrate into the cavity of the abdomen and pelvis. At the same time, lateral continuations of the process develop in the pleura, lungs, mediastinum and heart. Along the way, more or less extensive bags are formed, opening here and there with many fistulous tracts. Sometimes scarring occurs in one place, but in other places the process continues to move forward continuously.
The spread of the process can also occur along the large vessels of the neck, which, due to contact with the inflammatory focus, are also gradually affected. Growths form in their lumen, which serve as a source of specific embolisms and many metastases in the internal organs. In other cases, as happens with actinomycosis of the upper jaw, the base of the skull is affected after perforation, and death occurs from inflammation of the meninges and brain.
If actinomycosis becomes so widespread and has such an endless duration, then eventually it comes to cachexia, which is sometimes complicated by amyloid degeneration of internal organs and leads patients to death if they do not die earlier from damage to some important organ or from general pathological phenomena.
Sometimes actinomycosis exhibits not a chronic, but an acute or subacute course: fever appears, a strong reaction occurs, and signs of phlegmon are detected. If the lesion is localized or spreads along the bottom of the mouth, then rapid inflammation of the pharynx, tongue and adjacent tissue occurs, which leads to severe attacks of asphyxia.
Of the special localizations, we can mention actinomycosis of the tongue, most often the tip; it is found either in the form of an abscess the size of a nut or a pea, or in the form of multiple cracks. Actinomycosis can also be observed in the parotid glands, which can become infected through the Stenon's duct; in such cases, either abscesses or solid tumors develop, resembling actinomitotic neoplasms in cattle.
As for the primary lesion of the pharynx or esophagus, in addition to the phenomena of dysphagia and pain, which are not always observed or are temporary, it is detected by abscesses that spread to neighboring areas.
Actinomycosis of the thoracic organs
Actinomycosis of the thoracic organs most often develops secondaryly, as a continuation, especially with lesions of the mouth and pharynx. However, the lungs can sometimes become primarily infected; in such cases, therefore, one must keep in mind the existence of subtle and unrecognized lesions of the first pathways, especially lesions of the teeth.
Typically, changes of varying degrees occur in the lungs, pleura and mediastinum, as well as in the walls of the chest, and they are always associated with similar changes in neighboring organs. However, in some cases, there are exceptional or at least predominant lung lesions.
With actinomycosis of the lungs, it comes to ulceration and the formation of cavities of various sizes, which are usually surrounded by extensive sclerosis of the lungs and pleura. This strongly resembles pulmonary tuberculosis, and the error is especially possible in cases where the lesion is concentrated in the apices. The disease is manifested by cough, night sweats, fever, which can be irregular and has a hectic type, and sometimes repeated hemoptysis, chest pain and signs of compaction or emptying of the lung; finally, the patient develops purulent sputum, in which the characteristic elements of the parasite can be found. The duration of the disease is usually quite significant, and improvements alternate with deterioration. The general condition remains normal for much longer than with tuberculosis. Finally, most often there is a tendency to the formation of superficial lesions, abscesses on the walls of the chest or in the subcutaneous tissue and numerous fistulous tracts that open on the outer integument and lead to communication between the lung caverns and the external atmosphere. A scanty amount of fluid usually flows from the fistula openings, which is often very smelly and contains yellow grains of the parasite. These features are of great importance for recognition, but we must remember that tuberculosis can be associated with actinomycosis.
In other cases, the symptoms of pleurisy come to the fore, which appear either primarily, during acute symptoms, or secondarily, during another lesion; in this latter case, pleurisy occurs in an insidious manner and is manifested by chest pain, shortness of breath, and physical signs of effusion. The latter can be purulent if an actinomycotic focus has formed in the pleura itself, and the liquid turns out to be extremely fetid. However, the effusion may be purely serous or serous-fibrinous in nature, and in this case, pleurisy is caused by inflammation of neighboring organs, which proceeds from a purulent focus nesting either in the lungs, or in the mediastinum, or descending along the bone wall.
Actinomycosis of the thoracic organs also includes those extensive suppurations in the mediastinum that spread along the spine, exposing and corroding the bones, compressing the esophagus; the latter is often in communication with these purulent nests through a fistulous tract through which the infection has penetrated; from here purulent streaks form either in the adjacent serous membranes or in the walls of the chest. These suppurations lead to the development of abscesses in the intercostal spaces or on both sides of the spine. The probe enters these fistulous abscesses deeply, without reaching the bottom, so most often one can only guess that the abscess, inaccessible for examination, probably has a significant extent.
Actinomycosis of the abdominal cavity
Abscesses arising from the chest cavity easily penetrate the diaphragm, descend in front of the spinal column, following the sheath of the psoas muscle, into the iliac fossa and then appear below the femoral arch in the inguinal triangle. This path resembles the spread of a tuberculous abscess.
The anterior abdominal wall can also serve as a site of injury; Thus, extensive infiltration can be observed, extending from the pubis to the navel and sometimes presenting such significant hardness that it makes possible the assumption of the existence of a dense tumor.
The abdominal viscera may also be affected primarily. As for the intestines, here the lesion may remain hidden. If it is superficial and extensive, then symptoms of subacute or chronic enteritis, profuse diarrhea and vague pain occur. Much more often, a separate segment of the intestine is affected, and inflammation develops around the circumference and fusion with the peritoneum; When examining the abdomen, a more or less limited painful tumor is found, which after some time fuses with the wall and opens. In many cases, a picture of peritiphlitis or appendicitis is observed. Sometimes the disease takes the form of acute phlegmon; pain in the ileum, constipation, fever, redness and swelling of the abdominal wall and abscess formation with the emptying of foul-smelling pus mixed with fecal matter. In some cases, the course is chronic, and peritiphlitis recurs, abscesses empty into the intestines and recur again after a certain period of time.
A favorite place for the development of abscesses is also the circumference of the rectum; Before opening, they can, due to pressure, lead to symptoms of intestinal blockage.
Finally, purulent foci can appear in all places of the abdominal cavity, forming large bags where the insides float in bloody pus; these bags are opened on the outer integument through numerous fistulous tracts. Similar purulent foci surround the uterus, tubes and ovaries and communicate with the bladder, so that characteristic yellow grains can be found in the urine. All these localizations are observed in various forms, depending on the occasion.
Liver damage deserves special mention. In this case, the onset of actinomycosis is slow, insidious and is detected by progressive health problems and pain, which are localized in the right hypochondrium. Then, the liver increases in volume, and on the surface you can see reddish raised nodules, reminiscent of gummous neoplasms. Reactive changes occur around the circumference, namely, pleuritic effusion at the base of the chest on the right side and the phenomenon of limited peritonitis. The abscess then approaches the surface, the outer wall is deeply infiltrated, turns red and opens, and thick, greenish-brownish pus flows out of the hole, which subsequently turns into a fistulous tract. Death is a common outcome of this form of the disease.
Actinomycosis of the brain
Nerve centers are sometimes affected as a continuation of the neck abscess, when suppuration, spreading through the vessels, leads to perforation of the base of the skull; this complication leads to death. In other cases, infection occurs through the bloodstream: metastatic abscesses develop somewhere in the brain, manifested by symptoms of a brain tumor, pressure phenomena, headaches, limited soreness, partial paralysis and attacks of epilepsy, the cause of which can only be recognized when it is known that other characteristic lesions existed before this.
Rare forms of the disease
Damage to the genitourinary organs
Much less often, actinomycosis affects the organs of the genitourinary system. The development of diseases of the female genital organs is associated with the use of intrauterine contraceptives. Often the disease develops several months after removal of the intrauterine device. Women experience fever, weight loss, pain in the lower abdomen, and bleeding from the genital tract. An extensive infiltrate forms in the tubo-ovarian area. Actinomycetes are found in vaginal smears.
Damage to bones and joints
Actinomycetes penetrate bones and joints from affected neighboring organs or hematogenously. Cases of diseases of the pelvic bones, spine, legs, knee and other joints are described. Mycosis is often associated with injury. The disease occurs as osteomyelitis. It should be noted that despite severe lesions, patients are able to move, since the function of the joints is not seriously impaired. In the case of fistulas, a specific skin lesion is noted. The disease develops slowly.
Lymph node involvement
Most often, the disease affects the cervical, mandibular and mental lymph nodes. They increase in size, and periadenitis and adenophlegmon often develop. The disease has a protracted course. Complications include actinomycotic osteomyelitis.
Damage to the salivary glands
Actinomycetes enter the salivary gland through its duct. The disease develops with salivary stones, wounds, and the infection spreads through the bloodstream and through the lymphatic tract. In the area of the gland, a dense node is palpated, fused with the surrounding tissues. Over time, the infiltrate softens and suppurates. A purulent mass containing drusen of fungi is released from the fistula tracts. The disease progresses over a long period of time in waves.
Middle ear lesion
The disease occurs as recurrent otitis media. Without treatment, mycosis is complicated by mastoiditis. Thick purulent masses are often mistaken for cholesteatoma. Short courses of antibacterial drugs give a short-term effect. Dissection of the eardrum does not give the desired result.
Other rare lesions
- When the central nervous system is affected, the disease proceeds as meningitis and meningoencephalitis.
- Cases of damage to the maxillary sinuses and ethmoidal labyrinth have been described.
- Actinomycetes can infect the lacrimal sac, conjunctiva of the eye, lower and upper eyelid.
- The disease may affect the tonsils, tongue and oral mucosa.
Rice. 17. In the photo on the left there is secondary actinomycosis of the armpit area. In the photo on the right there is a skin lesion in the stage of abscess formation and fistula formation.
Rice. 18. Actinomycosis of the gluteal region.
What happens if actinomycosis is not treated?
Inside the tumor, ulcers form, covered with purple, increasingly thinning skin. They gradually approach the surface and then open up. A purulent fluid is released containing fat cells, fibrin and, above all, grains with fungal drusen. If a secondary infection occurs, phlegmon and large abscesses may develop.
Actinomycosis does not spread through the lymphatic tract, but the ulcers can open into the vessels, due to which the fungus penetrates the blood and is carried into all tissues and organs. This picture ends in death. Death occurs from exhaustion or amyloid degeneration, due to the absorption of decay products, and not from the action of a specific poison.
Mycetoma
Mycetoma (maduromatosis or Madura foot) has been known since ancient times. The disease most often occurs in people living in tropical countries. Pathological lesions appear on the foot in the form of several dense nodes, ranging in size from a pea or more. The skin over the nodes is initially unchanged, but then acquires a red-violet or brownish color. Over time, new nodes appear on the foot. The foot swells and increases in size. Over time, its shape changes, and the fingers turn upward. When abscess formation occurs, fistulas appear, from which a purulent mass with an unpleasant odor and a mass of yellowish inclusions is released. The pain syndrome is slightly expressed. As the disease progresses, fistulas begin to appear on the dorsum of the foot. The foot takes on a peculiar appearance - it is deformed and completely riddled with fistulas. Atrophy of the leg muscles is often observed. Without treatment, tendons and bones become involved in the pathological process. Usually one foot is affected. The disease lasts a long time - 10 - 20 years.
Rice. 19. Madura foot.
The causative agent of actinomycosis
Actinomycosis is characterized by the presence in pathological products of colonies of the parasite in the form of bodies, visible to the naked eye and either free in pus or contained in inflamed tissues.
These bodies are usually compared in size to grains of lycopodium, mustard or millet. Their sizes actually range for the smallest from 0.01-0.15 mm, and for the largest - up to 2 mm; on average their size is 0.45 mm. They have a roundish shape, a smooth or papillary surface, reminiscent of a mulberry, have an oily consistency and are easily crushed. Their color varies and depends on age: the youngest are gray and transparent like gelatin; then they become white, opaque and yellow like sulphur; the oldest ones acquire a brown, greenish and even black tint. They may be subject to limescale infiltration.
When examined under a microscope, a neutral mass is found in them, from which processes diverge in the form of rays, ending in yellowish, light-refracting swellings in the form of a club or knob. In sections or preparations prepared by splitting, it can be seen that the central mass consists of a dense fibrous network in which thin threads intersect; some of them go straight, while others are tortuous or spirally twisted. These threads are divided dichotomously; the branches have the same diameter as the original thread, and are connected to it continuously, without any articulation. The filaments consist of a thin shell and protoplasmic contents, sometimes monotonous, sometimes dotted with small grains. At the periphery, the threads receive a regular radiant arrangement and end in a slight swelling in the form of a button.
These club-shaped or knob-shaped swellings are yellowish in color, refract light and give the colony a very characteristic appearance. Each thread ranges from 4 to 12 microns in length and from 1.5 to 4 microns in width; they can be single or finger-like branched and consist of a thick membrane in the form of several layers, in which the thread of the fungus ends.
In addition to these elements, that is, fungal filaments and peripheral swellings, when splitting one can see short, rigid rods resembling bacilli, as well as roundish grains similar to micrococci.
Coloring reactions to radiant fungus are very characteristic. The threads are well stained using the Gram method, and with double staining with violet and eosin, very demonstrative preparations are obtained, where the swellings are pink and the threads are dark purple.
Radiant fungus is cultivated on various media.
Animal actinomycosis
Most often, actinomycosis affects cattle, a little less often - sheep, goats, pigs and horses. The disease is recorded throughout the year, but especially often during the stall period, when animals are fed dry food, as well as when grazing on stubble (the remains of cereal stems after harvesting). During this period, there is a high probability of damage to the oral cavity.
Actinomycetes enter the animal's body through damaged mucous membranes, as well as aerogenously (through the air). Granulomas develop in the organs and tissues of the animal, which affects the health of the animal and the possibility of its use for food purposes.
Rice. 20. Actinomycosis in animals.
Characteristics of the pathogen and causes of the disease
Actinomycetes have the properties of bacteria due to the presence of a nucleoid. Their thread-like structure, forming mycelium, resembles fungi; they reproduce by spores.
Radiant mushrooms are characterized by special resistance; they are widely distributed in soil, dust, walls covered with dampness, and on ears of grain crops. In the human body they are considered to be part of the opportunistic intestinal flora. They also live in tonsils, carious cavities, and plaque on teeth.
The causes of fungal activity are divided into endogenous and exogenous types.
Endogenous (internal) - characteristic of immunity deficiency, vitamin deficiencies, after serious illnesses and surgical operations.
The exogenous (external) type is possible when a pathogenic fungus is introduced into the body from the external environment: with dust, during agricultural work, harvesting grain crops.
As soon as an actinomycete enters the body, for example, with dust, granulomas (compactions) appear in the lungs, followed by a process of tissue necrosis. The pathological agent actively develops in the center of the granuloma, which is accompanied by severe inflammation. The process of skin dying causes the appearance of fistulas. It is possible that when a granuloma is opened, suppuration enters the bronchi. Sputum can come out when coughing, and it is in them that the fungus is found.
When actinomycetes are introduced into a wound through a scratch or puncture by sharp parts of a spikelet, an inflammatory process on the skin may occur.
Diagnosis of the disease
Diagnosis of actinomycosis is based on data from clinical and laboratory research methods. For the purpose of conducting microbiological research, the following are used:
- Discharge from fistulous tracts.
- Tissue biopsies.
- Points from lesions.
- Scrapings from granulation tissues.
- Exudate.
- Bronchial lavage water.
- Urine.
Discharge from the nose and throat, as well as sputum, have no diagnostic value, as they contain actinomycetes that usually live in the cavities of the upper respiratory tract, including pathogenic species. The only reliable study is the diagnosis of material obtained from transthoracic and abdominal percutaneous puncture biopsy.
Microscopic research method
This technique is focused on searching for specific granules in the material under study. These formations are accumulations of actinomycetes with a dense hyaline center surrounded at the periphery by filamentous cells of radiant fungi with flask-shaped thickenings at the ends. When stained with Gram stain, the mycelium becomes purple in color, and the periphery becomes pink.
Actinomycotic drusen should be distinguished from granules formed by other aerobic actinomycetes - Actinomadura, Nocardia, Streptomyces. A distinctive feature is that drusen of actinomycetes are always accompanied by accompanying microflora, while other pathogens are not.
Rice. 21. Actinomycetes under a microscope.
Rice. 22. The photo shows drusen of actinomycetes.
Microbiological method
Actinomycetes grow well on sugar agar and Sabouraud's medium. The first colonies (microcolonies) appear within 2 - 3 days. After - 10 - 14 days, lumpy or flat wrinkled macrocolonies grow. Based on the totality of biological properties, a pure culture is identified. To identify the pathogen in fixed tissues or directly in drusen, the method of direct immunofluorescence is used. Determining the sensitivity of pathogens to antibacterial drugs helps doctors select adequate antibiotic therapy.
Rice. 23. The photo shows a colony of actinomycetes.
Serodiagnosis
This diagnostic method is low specific and not sensitive enough.
Allergy diagnostics
An allergy test with actinolysate is of secondary importance. Only positive or strongly positive results are taken into account.
- Weakly positive tests are often recorded in persons with dental diseases, and primarily in alveolar pyorrhea.
- Negative tests are often recorded in individuals with severely reduced immunity, which is often observed in HIV-infected patients.
Express diagnostic methods
Direct and indirect fluorescence techniques are used to detect specific antibodies to actinomycetes and determine the type of pathogens located in drusen.
Use of PCR
Genetic studies are currently under development.
Differential diagnostic
Actinomycosis should be distinguished from a number of diseases:
- The pulmonary form of actinomycosis should be distinguished from abscess, neoplasms, deep mycoses of other nature and tuberculosis.
- The abdominal form of actinomycosis should be distinguished from appendicitis, peritonitis and other purulent diseases of the abdominal cavity.
- Bone lesions should be distinguished from purulent diseases of the musculoskeletal system.
- Actinomycosis of the skin should be distinguished from tuberculous lupus, scrofuloderma, gummous syphilides, malignant tumors and other deep mycoses.
Rice. 24. The photo shows a histological specimen of an organ affected by actinomycetes. The inflammatory infiltrate consists mainly of neutrophils. Granules (drusen) consist of many threads of branched gram-positive bacteria.
Publications in the media
A variety of microorganisms, populating almost any natural environment, invisibly accompany a person throughout his life. Living in soil, water, air, on plants, on the walls of residential and industrial premises, microorganisms are constantly in contact with humans. And, as a result, some of them have adapted to life on the skin, mucous membranes and internal cavities of humans (gastrointestinal tract, upper respiratory tract, urogenital tract, etc.), forming complex associations with specific relationships in their habitats. The human body normally contains hundreds of types of microorganisms: bacteria, protozoa, viruses, fungi. Opportunistic microorganisms constitute the normal microflora of a person, without causing harm to him. The term “normal microflora” unites microorganisms that are more or less often isolated from the body of a healthy person. It is often impossible to draw a clear boundary between saprophytes and pathogenic microbes that are part of the normal microflora. All microbes living in the human body simultaneously exist in these two states. Any of them can be the cause of infectious processes. Harmless “helpers” (lactobacteria, bifidobacteria) with a high degree of colonization can cause diseases. Conversely, pathogenic bacteria (pneumococci, meningococci, clostridia) colonizing the surfaces of human organs do not cause infection, which is facilitated by the competition of previously formed microflora and the protective properties of the macroorganism.
One of these “double” agents of human normobiota are actinomycetes.
They are widespread in the environment: in soil, water, including tap water and spring water, in hot mineral springs, on plants, on rocks and even in deserts. In the human body, actinomycetes saprophyte on the skin, in the oral cavity, dental plaque, tonsil lacunae, upper respiratory tract, bronchi, on the mucous membrane of the gastrointestinal tract, vagina, anal folds, etc.
The term actinomycetes (an outdated name for radiant fungi) currently extends to a wide range of gram-positive aerobic and microaerophilic bacteria that have the ability to form branching mycelium with characteristic sporulation, as well as irregularly shaped rods and coccoid elements that are formed as a result of fragmentation of the mycelium.
Actinomycetes include bacteria of the genera Actinomyces, Actinomadura, Bifidobacterium, Nocardia, Micromonospora, Rhodococcus, Streptomyces, Tsukamurella, etc.
The transition of actinomycetes from a saprophytic to a parasitic state is facilitated by a decrease in the immune defenses of the body, the presence of severe infectious or somatic diseases (chronic pneumonia, hidradenitis suppurativa, diabetes, etc.), inflammatory diseases of the mucous membranes of the oral cavity, respiratory and gastrointestinal tract, surgical interventions , long-term use of intrauterine contraceptives, hypothermia, injuries, etc.
In such cases, actinomycosis develops - a chronic purulent non-contagious disease caused by the formation of characteristic bluish-red and then purple infiltrates of dense consistency with multiple foci of fluctuation and fistulas with purulent discharge in soft and bone tissues of almost any localization. The duration of the incubation period can vary from 2–3 weeks to several years (from the time of infection to the development of manifest forms of actinomycosis).
The leading way in the development of actinomycosis is the endogenous method, in which the pathogen penetrates into tissues from places of its saprophytic habitat, most often through the digestive tract and oral cavity (carious teeth, gum pockets, tonsil crypts). The most favorable conditions for the introduction of actinomycetes are created in the large intestine, due to stagnation of food masses and a greater likelihood of injury to the wall. With the exogenous method, pathogens enter the body from the environment aerogenously or through traumatic injuries to the skin and mucous membranes.
The spread of actinomycetes from the primary lesion occurs by contact through the subcutaneous tissue and connective tissue layers of organs and tissues. The hematogenous route is also possible when an actinomycotic granuloma breaks through into a blood vessel.
The main causative agents of actinomycosis are Actinomyces israelii, A. bovis, Streptomyces albus, Micromonospora monospora; nocardiosis (“atypical actinomycosis”) and mycetoma - Nocardia asteroides, N. brasiliensis. The list of detected pathogenic actinomycetes is expanding. Modern literature increasingly describes cases of actinomycosis caused by rare species: Actinomyces viscosus, A. graevenitzii, A. turicensis, A. radingae, A. meyeri, A. gerencseriae, Propionibacterium propionicum, etc.
In the emergence and formation of the actinomycotic process, accompanying aerobic and anaerobic bacteria also play a significant role. Most cases of actinomycosis are caused by polymicrobial flora. Usually, along with actinomycetes, Staphylococcus spp., Streptococcus spp., Fusobacterium spp., Capnocytophaga spp., Bacteroides spp., representatives of the Enterobacteriaceae family, etc. are isolated. The addition of pyogenic microorganisms aggravates the course of actinomycosis, changes its clinical picture, and contributes to the spread of the process.
The clinical picture of actinomycosis is varied and is found in all countries in the practice of doctors of various specialties (dentists, surgeons, dermatologists, gynecologists, etc.). The main localizations are maxillofacial (up to 80%), thoracic, abdominal, pararectal, mycetoma (Madura foot). In addition, actinomycotic lesions appear not only in the classical form with characteristic tissue infiltration, abscesses and fistulas, but also in the form of the dominant pathogenic flora of a nonspecific inflammatory process, complicating the course of the underlying disease.
Actinomycetes may play an active role in the etiology of chronic tonsillitis. The palatine tonsils are colonized by actinomycetes in chronic tonsillitis and, in association with other bacteria, often provoke inflammatory reactions. Actinomycotic bacteremia of the oral cavity may occur as a result of dental procedures. In 30% of cases out of 80% of identified bacterimia, the actinomycotic nature of stomatitis is determined, the etiological agents of which are saprophytes of the oral cavity - A. viscosus, A. odontolyticus and A. naeslundi. By joining the local pathogenic flora, actinomycetes contribute to the development of a long-term non-healing inflammatory process with acne, trophic ulcers, hyperemia, maceration and weeping on the skin. Possessing a high degree of intestinal colonization, they are one of the main agents of dysbiosis. Summarizing all of the above, it should be noted that bacteria from a large group of actinomycetes can appear as participants in any infectious and inflammatory manifestations of the human body from dermatitis to endocarditis.
Thus, actinomycosis, characterized by a variety of localizations and clinical manifestations, needs to be diagnosed in a timely manner and possibly effectively treated, knowing the patterns of pathogenetic development, predisposing factors of infection, characteristics of pathogens and treatment methods.
However, the diagnosis and treatment of diseases associated with actinomycetes are the subject of a few specialized laboratories and clinics in the world. Difficulties in their differential diagnosis hinder the widespread recognition of these microorganisms in clinical practice.
Diagnosis of actinomycosis
A reliable sign of actinomycosis is the detection of characteristic actinomycotic drusen in the form of small yellowish grains, resembling grains of sand, in pus from fistulas, in biopsies of affected tissues. In native (not stained) and histological preparations, drusen are clearly visible against the background of purulent detritus in the form of radiant formations with a denser homogeneous granular center of thin, densely intertwined mycelium (photo 1). For their ability to form radially arranged filaments of mycelium, often with “cones” at the ends, actinomycetes were once called “radiant mushrooms”. The leading role in the formation of drusen - tissue colonies of actinomycetes - is the response of the macroorganism to antigens secreted by actinomycetes into the environment. Drus formation helps slow down the dissemination of the pathogen in the affected organism, as well as the localization of the pathological process. Actinomycosis is characterized by specific tissue reactions: granulomatous productive inflammation, leukocyte infiltration, microabscesses, “cellular” tissue structure, specific granuloma surrounded by polynuclear cells, giant and plasma cells, lymphocytes and histiocytes.
In the body of patients, drusen do not develop at all stages of the disease and are not characteristic of every variety of “radiant fungus”, so they are not always found, and the absence of drusen at the initial stages of diagnosis does not deny actinomycosis. In addition, these formations are capable of spontaneous lysis, calcification, deformation, calcification and other degenerative changes.
Drusen do not form in nocardiosis. In tissues, Nocardia is found in the form of thin mycelial filaments 0.5–0.8 μm and rod-shaped forms of the same thickness. Due to its acid resistance, Nocardia stains well according to Gram-Weigert in blue and according to Ziehl-Neelsen - in red: all this allows for differential diagnosis between actinomycosis and nocardiosis, since this is dictated by the difference in treatment methods for these diseases.
Microbiological examination, which includes microscopy and inoculation of pathological material on nutrient media, is important for the verification of actinomycosis of any localization. The optimal temperature for growth is 35–37°C.
When microscopy of clinical material and grown cultures stained with Gram or methylene blue, actinomycetes look like branched filaments 10–50 µm long or are represented by polymorphic short rods 0.2–1.0×2–5 µm, often with club-shaped ends, solitary, in pairs of V- and Y-shape configurations and in stacks. Gram-positive, but often the coloring is not typical, in the form of a rosary.
Many aerobic actinomycetes grow well on common bacteriological media - meat-peptone, trypticase-soy, blood and brain heart agars. To identify microaerophilic species, thioglycollate medium is used. The cultural characteristics of actinomycetes are very diverse. On dense agar media, colonies resemble bacterial ones in size - 0.3–0.5 mm in diameter. The surface of the colonies may be flat, smooth, bumpy, folded, granular or mealy. The consistency is doughy, crumbly or leathery. Many actinomycetes form pigments that give the colonies a variety of shades: grayish, bluish, orange, crimson, greenish, brown, blackish-violet, etc.
Clinical aerobic isolates, for example Nocardia asteroids and Streptomyces somaliensis, on a rich nutrient medium produce so-called atypical growth - dense leathery colonies, usually not pubescent with the aerial mycelium so typical of strains and without sporulation. To demonstrate differentiation and the formation of characteristic spores and pigments, special media are required: with colloidal chitin, soil extract or decoctions of plant materials.
In a liquid nutrient medium, pure cultures of microaerophilic actinomycetes form whitish “lumps” suspended in the substrate. The environment remains transparent. If there are bacterial impurities, the medium is cloudy and homogeneous.
Description of clinical cases of “atypical” actinomycosis
During the period of 2007, 25 patients with various clinical forms of actinomycosis were under our supervision. Among the examined patients there were 12 women and 13 men (aged 15-25 years - 4 people, 26-35 years - 4 people, 36-45 - 2, 46-55 - 5 people and 56-66 years - 10 people).
In addition to the “classical” actinomycosis of the maxillofacial, axillary and inguinal areas in the fistulous stage, we diagnosed actinomycotic complications of various pathological processes. For example, actinomycetes were found in the vaginal discharge of a patient with nonspecific colpitis and vulvovaginitis, which seriously aggravated the course of the underlying disease and required multiple courses of anti-inflammatory therapy. Actinomycetes in diagnostically significant quantities were identified during inflammatory processes in the oral cavity (in scrapings from the pharynx, tonsils, tongue), during otomycosis, during long-term non-healing macerations and hyperemia of the skin in the perianal area, from the mucous membranes of the rectal ampulla. The addition of actinomycetes to the pyogenic microbiota of trophic ulcers significantly aggravated the course of the disease, complicated the process of treating such patients, slowing down the regression of lesions. In patients with acne, when opening foci of inflammation in the sebum, actinomycetes were often found, the presence of which contributed to the development of a protracted course of the disease.
Under our observation was patient K., 43 years old, with a rare case of primary actinomycosis of the skin of the soft tissues of the groin areas, fistulous form.
She has been ill for 1 year, when changes appeared in the groin area on the left due to constant rubbing of the skin with uncomfortable underwear. I didn’t go to the doctors. It worsened in December 2007, when 2 ulcers and fistulas with purulent discharge appeared. She was consulted by a dermatologist who suspected a neoplastic process. Examined by an oncologist and parasitologist. The diagnosis of cancer or parasitic disease could not be established. She was referred to a mycologist with suspicion of deep mycosis. On examination: the lesion is located in the left groin area, measuring about 1.7x5 cm, there are 2 functioning fistulas with scanty purulent and sanguineous discharge. The patient was examined in the mycological laboratory of the Institute. E. I. Martsinovsky MMA named after. I.M. Sechenov for actinomycosis and bacterial infection. In the pathological material studied, microscopy of the specimens revealed actinomycetes, rods, cocci, and leptotrichia. When purulent discharge from fistulas was inoculated onto nutrient media, the growth of actinomycetes and coccal flora was obtained.
The diagnosis of actinomycosis of skin and soft tissues was verified. The patient is being observed and treated by a mycologist.
Patient N., 24 years old, diagnosed with acne, actinomycosis (photo 2).
Complaints of rashes on the skin of the body since childhood. We can reliably say that the disease was 10 years old, when acne was diagnosed at the age of 14. The patient was treated with external agents and antibiotics of various groups with a temporary effect. The general condition is currently complicated by chronic gastritis. On examination: the skin of the torso, face, and back is affected by inflammatory elements (papulopustular rash, open and closed comedones), in some places confluent in nature, infiltration of the skin and soft tissues. A microscopic examination of sebum from acne elements in the patient revealed cocci and single rods. In culture from the test material under the conditions of a mycological laboratory (photo 3).
Diagnosis: acne, actinomycosis of the face, trunk, back of the skin and soft tissues of a secondary nature, infiltrative form in the stage of moderate exacerbation. Currently, the patient is being treated by a mycologist at the clinic of the Institute named after. E. I. Martsinovsky MMA named after. I. M. Sechenov.
Treatment
Treatment of patients with actinomycosis is carried out comprehensively in various combinations depending on the location and clinical manifestations - iodine preparations, antibiotics, immunocorrective and restorative agents, actinolysate, local treatment with ointments, physiotherapeutic procedures and surgical intervention.
Iodide preparations (up to 3 g of potassium iodide per day), previously dominant in the treatment of actinomycosis, can now be used in combination with antibiotics or radiotherapy as an additional means for softening and resorption of the infiltrate.
Antibiotics occupy a leading place in the treatment of actinomycosis . The most commonly used antibacterial drugs are from the group of tetracyclines, penicillins, carbopenems, lincosamines, aminoglycosides, cephalosporins, the active ingredients of which are gentamicin, amikacin, tobramycin, lincomycin, levofloxacin, cefaclor, cephalexin. The drugs “Panklav”, “Flemoxin Solutab”, “Unidox Solutab”, etc. have proven themselves well. A long course of antimicrobial therapy (from 6 months to 1 year) and high doses of drugs are required. Traditional therapy for actinomycosis involves intravenous penicillin at a dose of 18–24 million units daily for 2–6 weeks, followed by oral penicillin, amoxicillin, or ampicillin for 6–12 months. In milder cases, in particular with cervical-maxillofacial actinomycosis, less intensive treatment with short courses of antibiotic therapy is sufficient. There is experience with effective short-term treatment of actinomycosis with imipenem for 6–10 weeks and ceftriaxone daily for 3 weeks. Antimicrobial therapy is continued for some time after symptoms disappear to prevent relapse.
When treating actinomycosis, it is also necessary to take into account the adjoining pathogenic microflora, which may exhibit increased resistance to antibiotics, which is explained by the long-term previous use of various chemotherapy drugs. To influence the accompanying flora, metronidazole (Metrogyl, Trichopol, Efloran) and clindamycin (Dalacin, Klimitsin) are used. A good anti-inflammatory effect is shown by the use of sulfonamide drugs (co-trimoxazole, sulfadimethoxine, sulfacarbamide). When a mycotic infection occurs, antifungal drugs are prescribed: fluconazole, itraconazole, terbinafine, ketoconazole, etc.
Immunocorrective agents . To correct immunodeficiency, Diucifon is indicated orally - 0.1 g 3 times a day or intramuscularly in the form of a 5% solution of 5 ml every other day for 3-4 weeks. In our opinion, the immunocorrective drug “Cycloferon” has also proven itself well - 2 ml intramuscularly every other day, 10 days.
General strengthening therapy stimulates the body's reactivity and increases the effectiveness of immunotherapy. Detoxification therapy is carried out with intravenous solutions of Hemodez, 5% glucose solution, etc. In order to activate regeneration, autohemotherapy is used - weekly, for a total of 3-4 transfusions per course. Vitamins are prescribed in average therapeutic doses.
Immunotherapy with Actinolysate promotes the accumulation of specific immune bodies and improves treatment results, allowing to reduce the amount of antibacterial agents and avoid unwanted side effects. Actinolysate is administered intramuscularly 2 times a week, 3 ml, for a course of 25 injections, courses are repeated 2-3 times with an interval of 1 month.
As local therapy , ointment treatment with antibacterial drugs of these groups, washing of fistulas with antiseptic solutions, furan-type drugs, administration of 1%, 2%, 5% alcohol solution of iodine, which help cleanse actinomycosis foci and eliminate inflammatory phenomena, are indicated.
Physiotherapeutic procedures . At the stage of lesion formation, electrophoresis of calcium chloride and Diphenhydramine is performed. After opening the lesions with residual infiltrates, iodine electrophoresis, Lidase, and fluoridation are prescribed. Ultrasound is applied directly to the area of the lesion according to the generally accepted scheme for 12–25 days (depending on the condition of the patient and the lesion) at intervals of 3–4 months.
Surgical treatment is carried out against the background of conservative therapy and consists of radical excision of lesions within apparently healthy tissue. If it is impossible to carry out radical surgery (for example, with cervical-maxillofacial actinomycosis), opening and drainage of abscess foci is indicated.
Treatment of actinomycosis
Treatment of actinomycosis is complex and includes several complementary techniques:
- Etiotropic therapy.
- Surgery.
- Immunotherapy.
- Boosting immunity.
- Hyposensitizing therapy.
- Physiotherapy.
Sanitation of organs that are supposed to be entry points for infection is mandatory: the mouth, nose, ear, throat, etc.
Of the antibiotics, the drug of choice is benzylpenicillin. Tetracyclines, erythromycin, clindamycin, chloramphenicol, kanamycin, ristomycin, chloramphenicol, etc. are also prescribed. Antibacterial treatment is prescribed and carried out under medical supervision.
If conservative therapy is ineffective, surgical treatment is indicated, aimed at excision of the affected tissue with subsequent drainage. For extensive suppuration in the lung tissue, lobectomy is indicated.
In order to stimulate the immune system, the introduction of a specific drug actinolysate is practiced.
After recovery, the patient is subject to observation for 2 years. 1-2 courses of anti-relapse treatment are indicated.
Diagnostics
The numerous localizations of actinomycosis lead to the fact that for each of them, to make a diagnosis, one must be guided by special signs. In all cases where lesions are susceptible to inheritance, special attention should be paid to the course and development of abscesses, to the grayish color and slight bleeding of fungal granulations, and especially to the unusual hardness, almost woody density of the surrounding infiltrate. However, in the end, the diagnosis can only be definitively established through bacteriological examination, that is, the discovery of radiant fungus grains or mycelium threads in pus or in fungous growths.
Similarly, with lesions of internal organs, if the unusual course of chronic peritonitis, pleurisy or liver abscess, their tendency to adhere to the walls and open with numerous fistulous tracts, can inspire the idea of actinomycosis, then final confirmation of the diagnosis is still possible only when a fungus is found. It is therefore necessary to examine pus, as well as excreta.
Treatment
Treatment of actinomycosis is quite lengthy, it can take up to several months. As a rule, the most effective method of therapy is the use of antibiotics (penicillin, doxycycline, erythromycin), but in the case of persistent severe fibrous tumors, surgery is indicated.
The information presented in this article is intended for informational purposes only and cannot replace professional advice and qualified medical care. If you have the slightest suspicion that you have this disease, be sure to consult your doctor!
The mechanism of origin and progression of actinomycosis (pathogenesis of the disease)
In the location of its introduction (as already noted, this is often the mucous membrane of the digestive system), the fungus Actinomyces bovis provokes inflammation. This process is characterized by exudation and cell proliferation. As a result, a granuloma appears from the epithelioid cells accumulated around the pathogen. In its middle, necrobiosis actively develops - an irreversible process leading to tissue death. In it, the appearance of grayish or yellow foci is observed, in the purulent-mucosal environment of which drusen of A. bovis lie. Plasma cells are grouped along the periphery of the focus.
Further, fibrous tissue develops in the node, which as a result is “covered” with lime. As the disease progresses, the abscesses begin to open, and rfyfks turn into fistulas - which secrete purulent fluid for a long time and do not heal.
Spreading into nearby tissues, the fungus destroys them and forms a scar. A. bovis is also quite capable of penetrating blood vessels, thus traveling throughout the body and giving rise to metastases.
Penetrating into the bone, the fungus triggers the development of osteitis, osteomyelitis and tissue necrosis.