Lower back pain occurs quite often. Patients say “my lower back hurts”, “my lower back is pinched”, “shot in the lower back”. If the pain is not acute, they may say “lower back hurts,” “lower back pulls,” “lower back ache.” Sometimes the pain is described as a burning sensation in the lower back.
Lower back
called the lower back - from the place where the ribs end to the tailbone. Perhaps a separate word for the lower back was needed just to indicate the place where it hurts. After all, if your back hurts, then in most cases it is your lower back that hurts.
What can low back pain look like?
Lower back pain
Most often, lower back pain occurs suddenly, sharply and is acute. In this case they talk about lumbago
(outdated popular name -
lumbago
). The pain is described as sharp, “shooting.” Movements are constrained, sometimes it is even impossible to straighten your back. With any movement the pain intensifies.
An attack of pain can last a couple of minutes, or it can last for a longer period of time (up to several days). It may be that the attack will pass and the pain will no longer remind itself, but often the pain returns and the person gets used to the fact that his lower back can hurt.
Lower back pain can not only be acute (sharp), it can be nagging and chronic. Mild but constant pain in the lower back, sometimes worsening, for example, during physical activity, an infectious disease, hypothermia, etc., is called lumbodynia
. Sometimes there is no direct pain, but stiffness remains in the lower back, and the patient experiences discomfort.
Diagnosis of the causes of lower back pain in women
If you experience lower back pain in combination with urination problems, the menstrual cycle, discomfort in the lower abdomen and other similar signs, you should consult a urologist or gynecologist. If there are signs of spinal diseases described above, you should immediately make an appointment with a chiropractor, neurologist or vertebrologist.
If it is difficult for a woman to independently figure out what caused the pain in the lower back, she is recommended to consult a therapist who will conduct an examination and prescribe laboratory tests and ultrasound, based on the results of which she will refer the patient to a specialist.
At the appointment, the chiropractor will conduct a thorough interview and examination of the woman, and will also use certain neurological tests. This will allow him to assess the degree of damage to the spine and make a preliminary diagnosis, which requires clarification using modern instrumental methods:
- X-ray;
- CT;
- MRI;
- electroneuromyography, etc.
The most informative and safe method for diagnosing pathological changes in the spine is MRI. This type of diagnosis allows you to detect the slightest deviations from the norm and thoroughly study the condition of the intervertebral discs, spinal cord and detect an area of compression of the spinal root. All this helps to create the most correct treatment tactics, which will give maximum results in the shortest possible time.
In our clinic, you can also learn in more detail about the composition of your body and the state of the vascular system, which is involved in the blood supply to internal organs, skeletal muscles, and the brain. Our experienced doctors will explain the data obtained to you in detail. Bioimpendansometry calculates the ratio of fat, muscle, bone and skeletal mass, total fluid in the body, and basal metabolic rate. The intensity of recommended physical activity depends on the state of muscle mass. Metabolic processes, in turn, affect the body's ability to recover. Based on the indicators of active cell mass, one can judge the level of physical activity and nutritional balance. This simple and quick test helps us identify disturbances in the endocrine system and take the necessary measures. In addition, it is also very important for us to know the condition of blood vessels for the prevention of diseases such as heart attacks, hypertension, heart failure, diabetes and much more. Angioscan allows you to determine such important indicators as the biological age of blood vessels, their stiffness, stress index (which indicates heart rate), and blood oxygen saturation. Such screening will be useful for men and women over 30, athletes, those undergoing long-term and severe treatment, as well as everyone who monitors their health.
In this case, body composition analysis gives us information that adipose tissue predominates in the body, and the bone-muscle component is in relative deficiency. These data will help the rehabilitation doctor competently draw up a physical activity plan, taking into account the individual characteristics of the patient.
Causes of lower back pain
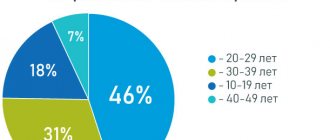
Lower back pain can be caused by various reasons, but the statistics are as follows:
- in 90% of cases the pain is caused by problems with the spine and back muscles;
- in 6% the cause of pain is kidney disease;
- 4% - diseases of other internal organs (genitourinary system, intestines).
The spine accounts for the majority of all cases of low back pain, and this is no coincidence. In humans, the center of gravity of the body is located exactly at the level of the lower back, and when walking, the entire load falls almost entirely on the lumbar spine (animals that move on four legs do not have this problem). And when a person sits down, the vertebrae of the lower back and sacrum experience the same force of pressure with which a 170-meter layer of water presses on a diver. Naturally, this area is particularly vulnerable.
Diagnosis and treatment of back pain in postmenopausal women
In recent years, there has been a steady increase in the number of patients with pathology of the musculoskeletal system (Waddell G., 1994). Chronic back pain affects up to 30% of the population in developed countries (Aronoff G. M., 1992, Bonica JJ, 1990).
In our country, the prevalence of vertebrogenic pain syndromes among the adult population reaches 62% in some regions.
Among the most common diseases, in the clinical picture of which pain syndrome predominates, are dorsopathies.
Dorsopathies are a group of diseases of the musculoskeletal system and connective tissue, the leading symptom complex of which is pain in the trunk and limbs of non-visceral etiology.
Degenerative changes in dorsopathy
Various structures of spinal motion segments may be involved in the degenerative process: intervertebral disc; facet joints; ligaments; muscles.
Dystrophic changes in the spine can vary in location.
Dystrophic changes in the disc: spondylosis (formation of spondylous marginal bone growths); Osteochondrosis is a pathology of the disc core.
A disc herniation should be considered as a manifestation of spinal osteochondrosis. The formation of pain syndrome during disc herniation is influenced by:
- violation of the biomechanics of the motor act;
- violation of posture and balance of the muscular-ligamentous-fascial apparatus;
- imbalance between the anterior and posterior muscle girdle;
- imbalance in the sacroiliac joints and other pelvic structures.
The following main diagnostic criteria for lumbar intervertebral disc herniation are distinguished:
- the presence of vertebrogenic syndrome, manifested by pain, limited mobility and deformities (antalgic scoliosis) in the affected part of the spine; tonic tension of paravertebral, as well as other muscles, the degree of involvement of which is determined by the intensity of nociceptive impulses from the affected SMS and compressed root;
- sensory disorders in the area of the neurometamere of the affected root;
- motor disturbances in the muscles innervated by the affected root;
- decreased or lost reflexes;
- CT, MRI or X-ray data verifying the pathology of the intervertebral disc, spinal canal and intervertebral foramina;
- data from electroneurophysiological studies (F-wave, H-reflex, somatosensory evoked potentials, transcranial magnetic stimulation), recording conduction disturbances along the root, as well as the results of needle electromyography with analysis of action potentials of motor units, allowing to establish the presence of denervation changes in the muscles of the affected myotome;
- the presence of relatively deep biomechanical disturbances in motor compensation.
Dystrophic changes in the joint - spondyloarthrosis.
Dystrophic changes in the vertebral bodies - aseptic necrosis (Kümel's disease); vertebral dystrophy - the strength of the vertebrae decreases, the disc straightens and gradually penetrates into the bodies of neighboring vertebrae - the shape of the disc is formed in the form of a biconcave lens.
In recent years, due to an increase in the proportion of elderly people in the population, among whom postmenopausal women predominate, the problem of dorsopathies is also considered from the point of view of the role that osteoporetic disorders play in the development of this process.
Osteoporosis is defined as “a systemic skeletal disease characterized by decreased bone mass and deterioration of bone microarchitecture, leading to increased bone fragility and risk of fracture.” According to some estimates, osteoporosis is found in more than 30% of women over 50 years of age.
The development of postmenopausal osteoporosis is primarily associated with insufficient estrogen production, which leads to disruption of the synthesis of local mediators of bone tissue remodeling.
With age, other important mechanisms play an increasingly important role in the progression of osteoporosis, the main of which is vitamin D deficiency and the development of resistance of a number of tissues, including skeletal bones, to the effects of this vitamin.
The following risk factors for the development of osteoporosis can be identified:
- genetic and anthropometric: old age, low bone mass, ethnic predisposition (Caucasian and Mongoloid races);
- hormonal: female gender, early menopause, late onset of menstruation, amenorrhea, infertility;
- lifestyle: dietary habits, smoking, low physical activity, caffeine abuse;
- the presence of concomitant diseases: endocrine, rheumatic, hematological, tumor, etc.;
- long-term use of medications, surgical operations: glucocorticosteroids, chemotherapy, oophorectomy, removal of the thyroid gland.
The most common causes of secondary low back pain in postmenopausal women are:
- congenital anomalies: Spina bifida, spondylolisthesis;
- trauma: vertebral fractures, protrusion of intervertebral discs;
- arthritis, including reactive arthritis, ankylosing spondylitis, etc.;
- other diseases: metabolic (osteoporosis), tumors, infections (tuberculosis, osteomyelitis), mental illness;
- projection pain in diseases of the internal organs: ulcer or tumor of the posterior wall of the stomach, inflammation, cyst or tumor of the pancreas, dissecting aneurysm of the abdominal aorta, colon tumors;
- diseases of the genitourinary organs: urolithiasis, endometritis, uterine prolapse, uterine cancer.
The diagnostic algorithm for a doctor’s actions when a postmenopausal patient comes to complain of lower back pain is presented in Fig. 1.
| Figure 1. Diagnostic algorithm for a doctor’s actions when a postmenopausal patient visits with a complaint of lower back pain |
First of all, the doctor takes a medical history and performs a physical examination of the patient.
Then, in the absence of neurological deficit, it is necessary to conduct an x-ray examination of the lumbar and sacral spine. In this case, the following pathological changes can be diagnosed: metabolic bone diseases (osteoporosis, osteomalacia, hyperparathyroidism), osteoarthritis, compression fracture, ankylosing spondylitis (Bechterew's disease), spondylolisthesis, tumors (hemangioma, osteosarcoma, metastases, osteoma, myeloma), spinal osteochondrosis, urolithiasis disease.
If no pathological changes are detected during X-ray examination, it is necessary to conduct a manual examination of the pelvic organs (rectal, vaginal). Endometriosis, tumors in the pelvic area, infections of the pelvic organs (abscess, cervicitis) can be diagnosed.
If there are no pathological changes in the pelvic organs, it is necessary to conduct a computer or magnetic resonance examination. In this case, the following pathological changes can be detected: infectious process (osteomyelitis, tuberculosis, syphilis), retroperitoneal tumors, intervertebral disc herniation, spinal canal stenosis.
In the absence of the above diseases, it is necessary to do a clinical blood test and determine the erythrocyte sedimentation rate (ESR). If ESR increases, it is necessary to exclude rheumatism and spinal tuberculosis. If the ESR is normal, it should be taken into account that back pain can be caused by sprained muscles and ligaments, varicose veins of the pelvis, and psychosomatic disorders.
If a physical examination reveals neurological deficits or other abnormalities, a computer or magnetic resonance imaging study should be performed. In this case, the following pathological changes can be detected: abdominal aortic aneurysm, intervertebral disc herniation, spinal compression fracture, spinal tumors, epidural abscess of the lumbar spine (Fig. 2).
| Figure 2. No radiographic changes |
The main factors in the etiopathogenesis of back pain in elderly women are:
- metastatic lesion of the skeleton;
- osteoporosis, manifested by bone deformities;
- spinal osteochondrosis, complicated by disc herniation, spinal canal stenosis.
Differential diagnosis of lumbar dorsopathy
Visceral pathology:
- pancreatitis, pancreatic tumor;
- peptic ulcer;
- nephrolithiasis, pyelonephritis;
- renal vein thrombosis;
- abdominal aortic aneurysm;
- ovarian tumors, cysts;
- inflammatory processes of the abdominal and pelvic organs.
Spinal lesions:
- primary bone lesions (osteoporosis, osteomalacia);
- vertebral lesions (metastases, myeloma, fractures, spondylitis, primary tumors);
- degenerative diseases of the spine leading to gross changes, including intervertebral hernias, spinal stenosis.
Treatment of back pain in postmenopausal women
To treat dorsopathies, a number of methods are used, which include medications, including enzyme therapy, orthopedic, physiotherapy, massage, electroacupuncture, manual therapy, etc. (Khabirov F.A.). However, none of the listed methods fully meets modern requirements in terms of effectiveness and tolerability. In particular, this applies to the use of non-steroidal anti-inflammatory drugs (NSAIDs), which have a pronounced analgesic effect. However, along with reducing inflammation and pain, drugs in this group often cause adverse side effects, such as damage to the mucous membrane of the stomach and intestines (“ulcerogenic effect”), impaired renal function, platelet function, etc.
In recent years, the group of NSAIDs has been supplemented with new drugs - so-called selective cyclooxygenase-2 inhibitors. A distinctive feature of these drugs is a more selective inhibition of the activity of one of the 2 isoforms of the key enzyme in the biosynthesis of prostaglandins - cyclooxygenase-2 (COX-2), which, according to modern concepts, is responsible for the biosynthesis of these anti-inflammatory and algogenic substances in the lesion. inflammation. At the same time, new NSAIDs have a slight effect on another isoform of this enzyme - cyclooxygenase-1 (COX-1), which carries out the biosynthesis of prostaglandins outside the focus of inflammation. The prostaglandins formed with its participation are important physiological regulators of microcirculation in the mucous membrane of the gastrointestinal tract and kidneys, gastric secretion, blood cell functions, etc. It is the non-selectivity of the action of “old” NSAIDs in relation to COX-1 and COX-2 that is considered as the cause of the development most of the side effects they cause. At the same time, selective COX-2 inhibitors have demonstrated a high level of safety in controlled clinical trials.
Celebrex and Movalis are new specially developed drugs in this group that have minor side effects on the gastrointestinal tract.
Celebrex (celecoxib) is a new specially developed drug in this group that has minor side effects on the gastrointestinal tract and is highly effective, comparable to the “gold standard” NSAID - diclofenac.
Celebrex is recommended for use in a dose of 200 mg 2 times a day in the complex treatment of patients with severe pain syndrome due to dorsopathy.
Celebrex does not cause platelet aggregation, does not have a negative effect on cartilage tissue and combines well with antihypertensive drugs (ACE inhibitors) and oral hypoglycemic drugs (glibenclamide and tolbutamide)
From the point of view of the speed of achieving the effect, parenteral and rectal routes of administration of non-steroidal anti-inflammatory drugs have an advantage.
Local use of analgesic ointments, gels, creams, characterized by a high content of non-steroidal anti-inflammatory drugs, is indicated.
Finalgel is a gel consisting of piroxicam. Penetrates well into subcutaneous fatty tissue, muscles and ligaments. Has an analgesic, anti-edematous, cooling effect. Directions for use: squeeze out the gel in a volume of 3 cm, rub well. Use 3-4 times a day.
Finalgon is an ointment containing two drugs: nonivamide, a synthetic derivative of xapsaicin, a locally irritating substance isolated from pepper, and nicoboxil, a derivative of nicotinic acid, which has a pronounced vasodilator effect. The main thing in the mechanism of action of finalgon is the stimulation of skin-visceral receptors. As a result of increased blood flow in the affected area, pronounced analgesic, antispasmodic and warming effects are observed, and local blood circulation improves. Method of use of the drug: approximately 0.5 cm of ointment is squeezed out of the tube; The drug is applied to a palm-sized area of skin; to enhance the therapeutic effect, you can cover the sore spot with a woolen cloth.
To relieve tonic muscle tension during back pain in postmenopausal women, centrally acting muscle relaxants are used. Drugs in this group do not affect neuromuscular transmission and at the same time reduce the tone of skeletal muscles as a result of inhibition of mono- and polysynaptic reflexes by reducing the release of excitatory amino acids (glutumate and aspartate). It should also be noted that these drugs have a moderate analgesic effect.
The use of medications that have a positive effect on bone tissue also becomes of great importance in the treatment of dorsopathies (including those developing against the background of osteoporosis). Such drugs include preparations based on vitamin D, its active metabolites and derivatives.
Vitamin D plays an important role in the functioning of the body as a whole. It can be considered as a leading factor in maintaining calcium homeostasis; in addition, this vitamin is involved in key processes of skeletal formation and bone tissue remodeling. The main mechanisms of action of vitamin D are: increased absorption of calcium in the intestine, activation of bone remodeling processes, suppression of excessive secretion of parathyroid hormone, improvement of neuromuscular conduction and contractility of motor muscles.
Alfacalcidol, 1α-hydroxyvitamin D3, is a synthetic analogue of the active metabolite of vitamin D3, calcitriol. This drug is a prodrug, that is, a substance that turns into an active form after entering the body. As a rule, prodrugs are better tolerated, last longer, and are more effective. Alfacalcidol is characterized by a longer period of existence in the body than calcitriol, which allows it to be prescribed 1 or 2 times a day; in addition, unlike preparations of native vitamin D, alfacalcidol does not require re-hydroxylation in the kidneys, and in one stage it turns into active metabolite of vitamin D. Taking into account the reduced activity of the kidneys in elderly people, who have a reduced ability to form calcitriol, the use of alfacalcidol for a lack of vitamin D in the body can be considered justified.
When choosing therapy for postmenopausal women with back pain, an individual approach is required - the clinical manifestations of the disease, structural features of the spine, the stage of the pathological process, and the presence of concomitant pathologies should be taken into account.
Thus, osteoporetic and biomechanical disorders play an important role in the pathogenesis of dorsopathies in postmenopausal women.
The diagnostic algorithm for dorsopathy should include an assessment of the condition of bone tissue (densitometry, CT).
Complex treatment of dorsopathies in postmenopausal women involves the combined use of non-steroidal anti-inflammatory drugs and preparations of the active metabolite of vitamin D.
T. T. Batysheva, Candidate of Medical Sciences G. Ya. Shvarts Polyclinic for Rehabilitation No. 7, Moscow
Diseases of the musculoskeletal system that cause lower back pain:
Why does your lower back hurt?
- pinched sciatic nerve. The nerve roots extending from the spinal cord are compressed by neighboring vertebrae. In this case, a sharp, shooting pain occurs. As a rule, pinched roots become possible due to degenerative changes in the spine (osteochondrosis): the intervertebral discs separating the vertebrae from each other are destroyed, the gap between the vertebrae narrows and sudden movement (tilting, turning) can lead to pinching of the nerve branch;
- sciatica (lumbosacral radiculitis). Pinched nerve roots can become inflamed. Inflammation of the nerve roots is called radiculitis (from the Latin radicula - “root”); To indicate inflammation of the sciatic nerve, a special name is sometimes used - sciatica. If the sciatic nerve is damaged, lumbar ischialgia may be observed - pain in the lower back, also spreading to the buttock and leg along the sciatic nerve;
- intervertebral disc herniation – protrusion of a fragment of the intervertebral disc into the spinal canal. Occurs as a result of injury or degenerative changes in the spine (osteochondrosis);
- myositis of the lumbar muscles. Myositis is an inflammation of skeletal muscles. The cause of myositis of the lumbar muscles can be hypothermia or sudden tension.
Also, lower back pain can be caused by diseases such as multiple sclerosis, degenerative sacroiliitis, osteoporosis.
Diagnostic methods
After an appointment with a specialist, the following diagnostic control methods are usually used:
- ultrasound examination of the kidneys, pelvic organs and abdominal area;
- X-ray of the spine to check for changes in the intervertebral discs;
- MRI image, reflecting a broad picture of the processes occurring in the spine;
- biochemical analysis of blood, urine, cerebrospinal fluid, etc.
When determining the source of a painful symptom, a highly specialized specialist may prescribe additional types of studies based on the patient’s medical history.
Prevention of low back pain
The occurrence of lower back pain is often provoked by a careless attitude towards one’s own health. Pain may be caused by:
- staying in the same position for a long time (for example, during sedentary work);
- incorrect posture;
- low mobility;
- excessive physical activity.
All these factors contribute to the development of diseases manifested by lower back pain. The risk of pain can be reduced by following the following advice from doctors:
- watch your posture;
- Avoid uncomfortable postures when working while sitting. It is advisable that the knees are slightly higher than the hip joints. To do this, use a low chair or footrest. Place a small pillow between your lower back and the back of the seat;
- When working sedentarily, you need to get up from time to time to move around. Take five-minute breaks every hour; how to lift weights correctly
- It is advisable to sleep on an orthopedic mattress (elastic and quite hard);
- You need to lift weights by bending your knee joints, not your back. That is, you need to squat down, bending your knees, and then straighten them, while maintaining a straight line of your back;
- When carrying a load, it must be evenly distributed between both hands; you cannot carry the entire load in one hand (one heavy bag);
- Every day you should do a set of exercises aimed at strengthening the abdominal and back muscles.
How to lift weights
Diagnostic features
If there are no additional symptoms, you should consult a neurologist or orthopedist. In other cases, the help of other doctors is necessary. To begin with, you can visit a therapist, and if necessary, he will refer you to additional consultations with specialized specialists. Diagnosis of this ailment must be comprehensive. Typically it includes:
- radiography, MRI, CT of different parts of the spine;
- examination by a gynecologist;
- taking a smear;
- Ultrasound of internal organs and blood vessels;
- urine and blood tests.
X-ray and other images can reveal abnormalities in the spinal column: inflammatory processes, formation of osteophytes, thinning of intervertebral discs, displacement of the vertebrae. Tests and ultrasound provide information about the condition of internal organs, help detect the presence of inflammation and establish the nature of its origin.
Lower back pain due to kidney disease
For lower back pain, it is important to determine what is causing it - pathologies of the musculoskeletal system or kidney disease (as well as other internal organs). Diagnosis must be carried out by a doctor. However, there are signs to suggest that the pain may be due to problems with the kidneys and/or other organs of the genitourinary system. If these symptoms occur, it is advisable to immediately contact a urologist. Kidney disease (or more broadly, the genitourinary system) can be suspected if lower back pain is accompanied by:
- general deterioration in health (lethargy, drowsiness, weakness, increased fatigue);
- swelling of the eyelids and face. Swelling is especially pronounced in the morning, after waking up, and subsides in the evening;
- increased body temperature, chills, sweating;
- loss of appetite, nausea, vomiting;
- frequent or painful urination;
- changes in the characteristics of urine (it may become more concentrated in color or, conversely, colorless, contain mucus or blood);
- increased blood pressure.
Kidney disease is one of the possible causes of lower back pain
Also an important sign that lower back pain is caused by problems of the internal organs, and not the musculoskeletal system, is its independence from the position of the body: the pain does not increase or decrease from changes in the position of the body and limbs. However, with prolonged standing in a standing position due to check pathology, the pain may intensify. The location of the pain also matters. With kidney disease, pain is most often observed on one side (since usually only one kidney is affected). Kidney pain may not be limited to the lower back, but may spread along the ureter, to the groin, to the external genitalia, to the inner thighs.
Diagnosis
First of all, patients turn to a therapist, who conducts a full examination of the whole body and prescribes laboratory tests. If the patient exhibits symptoms characteristic of gynecological, degenerative or oncological pathologies, the doctor makes an appointment with a highly specialized doctor. This could be a vertebrologist, gynecologist, rheumatologist or oncologist.
These specialists check the patient using instrumental analysis methods. A gynecologist can use ultrasound to study the condition of a pregnant woman and a patient with gynecological diseases. This is a safe diagnostic method that uses ultrasound waves to obtain an informative clinical picture. Polyps, cysts and endometriosis are clearly visible on the monitor, so a specialist can easily determine their location and prescribe surgical treatment.
In the case of cancerous tumors or injuries of the lower back, the doctor prescribes a CT or MRI of the spine. Computed tomography is well suited for older people, when the effect of radioactive substances on the body is much less. Magnetic resonance imaging allows you to examine the body of a young woman or teenager using electromagnetic waves.
MRI is performed in open-type machines, which allows patients with fear of claustrophobia to be diagnosed. During the scan, the patient must lie still for about 15–20 minutes.
Lower back pain: what to do?
Low back pain is a symptom of a disease that requires treatment. Therefore, it is necessary to consult a doctor. But in the event of a sudden attack of acute pain (“lumbago”, typical of radiculitis), first of all, it is necessary to relieve the pain syndrome. Doctors advise:
- use gentle heat. Tie a woolen scarf or woolen belt around your lower back;
- take painkillers;
- It is necessary to take a position that allows you to relax your back muscles. It is recommended to lie on your back, on a hard, flat surface (board); The legs should be raised and bent at the knees, for which a rolled blanket or pillow should be placed under them. (It is not advisable to lie on the floor; there may be a draft).
What to do for acute lower back pain
The proposed pose is not a dogma. The patient should feel relief, so other positions are possible; for example, lying on a board, place your legs bent at the knees on it, holding a pillow between them. You can try lying on your stomach and stretching your legs, placing a bolster under your ankle joints. If the severity of the pain has been relieved, this does not mean that a doctor is no longer needed. Without proper treatment, attacks will recur, and the situation as a whole will worsen.
Causes of back pain
Finding out why your back hurts is not easy. The fact is that the spine is at the same time a support, protection, and shock absorption of the body. If chronic back pain appears, the problem is a violation of any of these functions.
If you feel back pain between the shoulder blades, it may be associated with bronchitis and cough. If your back muscles hurt, the discomfort may be due to overexertion due to heavy lifting the day before. Back pain on the right or left can be caused by a sudden rotation of the body.
There are more serious causes of periodic sharp pain. For example, inflammation of internal organs, kidney stones, spinal bruise. If diagnostics of the back do not show degenerative changes, it is worth examining the internal organs. Thus, discomfort in the lumbar region may be a symptom of nephrosis.
In one case or another, the treatment is different, so first of all you need to establish the cause.
Types of diseases based on the nature of back pain
Possible causes of aching pain :
- myositis;
- lumbago;
- intervertebral hernia.
It worsens when lifting weights, physical work, hypothermia, or staying in one position for a long time.
Causes of shooting pain in the limbs :
- intervertebral hernia;
- radiculitis;
- osteochondrosis.
Discomfort increases with walking, bending, coughing and sneezing. Feeling weak in the legs and arms.
Causes of throbbing pain :
- intervertebral hernia;
- osteochondrosis;
- lumbago;
- spondylosis.
The discomfort does not go away even after taking an analgesic.
Possible causes of bursting and pressing pain :
- in the chest area - pulmonary embolism and myocardial infarction;
- on any part of the spine - spondyloarthrosis;
- in the lumbar region - intestinal obstruction;
- in the neck area - atherosclerosis.
| Nature of pain | Diseases that cause it |
| Aching back pain (acute and chronic) | Lumbago (shooting in the lower back). The reason is hard physical labor. It usually goes away on its own within a few days. |
| Myositis, muscle strain, sudden heavy lifting, hypothermia, maintaining an uncomfortable position for a long time, for example during work. | |
| Displacement of intervertebral discs. The most common cause is osteochondrosis, but displacement can also occur with sudden heavy lifting and constant high physical activity. | |
| Sharp, radiating to the extremities | Osteochondrosis. Causes nagging pain in the back that radiates to the leg and becomes stronger when sneezing, coughing, or straining. |
| Radiculitis. Constant sharp (stabbing) or dull pain. It is usually localized on one side, can radiate to the thigh, buttock, leg, lower leg, and sometimes causes numbness and itching. The pain can also be burning and intensifies with movement. | |
| Intervertebral hernia. With this pathology, pain occurs when bending over, lifting heavy objects, intensifies when sneezing, coughing, moving, and is accompanied by weakness in the leg. | |
| Throbbing pain, severe, may not go away after taking an analgesic | Osteochondrosis, cracks in the vertebrae, lumbago, intervertebral hernia, spondylosis. |
| Bursting | In the upper back and in the middle of the sternum - may indicate angina pectoris, myocardial infarction, pulmonary embolism. In the lower back - intestinal obstruction, spondyloarthrosis. |
| Pressing | Angina pectoris, myocardial infarction, problems with the gallbladder (pain occurs after eating), atherosclerosis, hypertensive crisis. |
Why does my back hurt after sleep?
After waking up in the morning, you feel stiffness, discomfort and pain below the shoulder blades, in the right or left side, in the lumbar region. These sensations can be associated not only with an incorrect sleeping position or resting on an incorrectly selected mattress. After sleep, your back hurts for the following reasons:
- during the day physical work was performed with sudden lifting of weights;
- back muscles are weakened;
- intervertebral hernia or osteochondrosis is diagnosed;
- hypothermia occurred;
- the spine is curved, causing the muscles to contract unevenly;
- obesity, due to which the load on the spine is distributed unevenly;
- pregnancy;
- stress.
Diseases associated with joints and the spinal column
Back pain in the spinal area can occur due to the development of pathologies of the musculoskeletal system such as:
- Ankylosing spondylitis. The paravertebral muscles spasm, so to relieve discomfort the patient tilts the body forward. Over time, the vertebrae become woody, inflamed and fused, so the flexibility and mobility of the spine is impaired.
- Spondylolisthesis and spondylolysis. Due to these diseases, pain is mainly localized in the lumbar region. The vertebrae move forward or backward and compress the nerve endings;
- Osteochondrosis. The depreciation of the spine worsens. The discs between the vertebrae crack, the fibrous ring ruptures, and through the resulting cracks the core of the disc comes out and is pinched.
- Rheumatoid arthritis. Develops in the knees, shoulders, hip joint and moves to the cervical spine. In the morning, you feel stiffness and lumbago due to excess pressure on the nerves from the affected vertebrae.
- Osteomyelitis. Infection of the bone tissue of the spine causes inflammation and severe muscle pain.
- Reiter's disease results from inflammation of the small supporting muscles of the back.
- Intervertebral hernia due to the fact that during movement the protrusion between the vertebrae is compressed and pinched.
Muscle-related diseases
When determining the causes of back pain, tightness and spasms of the muscular corset that supports the spine are often discovered. Mobility is impaired as a result of:
- Fibromyalgia. My back hurts from my neck to my lower back. Neurological symptoms can be observed - sensitivity increases when pressing certain points on the back.
- Polymyositis. The back muscles become inflamed due to hypothermia and overexertion. It hurts to turn the body, muscle weakness is felt.
- Dermatomyositis. The skin near the striated and smooth muscles of the back becomes inflamed.
- Charcot's disease. The peripheral nerves that run along the spine become inflamed. Sensitivity worsens, muscle weakness increases, and gait changes.
- Polymyalgia rheumatica. It is difficult to raise your arms and stand on your feet without the help of someone else. The asymmetry of the back is noticeable.
Spinal cord pathologies
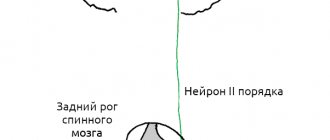
Back pain often occurs due to spinal cord compression. The spinal cord is the connecting link between the brain and the body. It runs from the head to the tailbone in the spinal canal between the vertebrae. There are 31 branches leaving the spinal cord. Each nerve is responsible for the innervation of one or another part of the body. The back may hurt due to pinching or inflammation of any part of the spinal cord as a result of:
- compression of the spinal membranes due to a spinal fracture, abscess or hematoma;
- cerebrovascular accidents;
- inflammation of nearby muscles;
- lack of vitamins and minerals;
- hemorrhages;
- complications of syphilis or HIV;
- multiple sclerosis;
- back tumors of various etiologies.
Back pain due to psychosomatics
Increasingly, back discomfort is not associated with physical illness. After the examination, no pathology is detected, which means that pain in the back and joints is caused by psychological factors. Unpleasant sensations can be triggered by depression, chronic stress, nervous tension, and sexual dissatisfaction. Due to nervousness, the gait changes, lumbago worsens, and sensory disturbances appear.
Which doctor should I contact with a complaint of lower back pain?
If you have lower back pain, it is best to consult a general practitioner, since first of all you need to determine which organ disease is causing the pain. Depending on the results of the examination, consultation with a particular medical specialist may be required. Can be assigned:
- consultation with a neurologist to assess the condition of the spine, back muscles and nervous system;
- consultation with a urologist – in case of suspected urinary system disease;
- consultation with a gynecologist – if chronic diseases of the female reproductive system are suspected or present;
- general blood test and general urinalysis - to confirm or exclude the inflammatory nature of the disease;
- radiography of the spine;
- Ultrasound of the hip joints;
- as well as other studies.
Diseases of the genitourinary system
Pain in the lumbar region is sometimes associated with diseases of the genital area or pathologies of the urinary system. This is indicated by fever, intoxication, weakness, appetite and sleep disturbances, and rapid weight loss. Pain on one side or throughout the lower back may, for example, be a sign of pyelonephritis (unilateral or bilateral, respectively) - an inflammatory pathology of the kidneys. Signs of genitourinary diseases:
- pain in the urethral area;
- yellow, greenish, brown discharge;
- change in urine color;
- frequent or infrequent urination;
- false urge to urinate;
- increase in the volume of the lower abdomen;
- menstrual irregularities;
- itching, pain, swelling in the perineum.
If such symptoms appear, you should urgently consult a doctor: many gynecological and kidney diseases are life-threatening and require hospital treatment, in some cases surgical treatment.
Diagnostics
To make a diagnosis of back pain, you need to make an appointment with a neurologist, take tests if necessary, and also undergo hardware testing as prescribed by a specialist.
- Blood tests.
They allow you to determine the presence of infection, ESR (increased erythrocyte sedimentation rate, which indicates inflammation, infection). If an increased level of leukocytes is detected, then this is also a sign of inflammation and infection. Also, blood tests can determine iron deficiency anemia, the cause of which may be oncology. - Hardware diagnostics.
- Duplex and triplex ultrasound scanning of the vessels of the neck and brain. Allows you to anticipate the structure and patency of blood vessels, the presence of narrowing or dilatation, plaques, blood clots, as well as compliance of blood flow with standards. It is used in diagnosing the causes of headaches, dizziness, high blood pressure, as well as in cases of suspected cerebrovascular accident, and in the early diagnosis of pre-stroke conditions.
- MRI (magnetic resonance imaging). The most accurate and effective examination method. Allows you to visualize tumors on the vertebrae, herniated intervertebral discs, compression (and its degree) of the spinal nerves and spinal cord, narrowing of the spinal canal, inflammatory changes, including post-traumatic ones. MRI is required before surgery and in the postoperative period.
- CT (computed tomography). Detects vertebral fractures and their nature, allows you to find even very small fragments if they were formed due to injury. Based on the data obtained, you can create a 3D image of the desired area. CT “sees” what went unnoticed during radiography.
- Radiography. Allows you to assess the condition of bone structures. It is carried out to diagnose fractures, arthritis, spondylolisthesis, and the degree of postural impairment. It can be performed with functional tests, that is, when the patient flexes and extends the spine during the examination. Visualizes inflammation of the joints in the spine, helps to identify the localization of compression of the nerve processes by indirect signs. The degree of color intensity of the vertebrae in the image allows you to evaluate their strength (with osteoporosis they are more “transparent”, and when healthy they are bright white).
- Electromyography (EMG). A study aimed at determining the condition of nervous tissue. It evaluates the electrical impulses produced by the nerves, as well as the reaction of the muscles to them. Electromyography helps identify nerve compression caused by stenosis (narrowing) of the spinal canal or intervertebral hernia.
- Bone scan. This test is necessary if the doctor suspects a bone tumor or compression fracture due to osteoporosis.