When someone in the family becomes seriously ill, goes to the hospital, undergoes surgery and is bedridden for a long time after it, all the actions of loved ones are aimed at taking measures to arrange the sick home and organize the recovery process.
At the same time, they may not remember the danger of bedsores, since they have never encountered this phenomenon. Meanwhile, this complication can arise in just 2 hours of bed rest, and a significant number of people are discharged home from the hospital with bedsores.
So, relatives are caring for a patient and notice with horror that bedsores have appeared, what can they do to prevent them from happening? First of all, don't panic. At the initial stage, they are treated well, and there are many official and folk remedies. It is possible that the patient is not turned over in bed often enough.
Treatment of bedsores: a single algorithm of actions
The most reasonable solution is to invite a professional nurse who knows how to avoid bedsores in bedridden patients and how to treat them if they already exist. If the choice of a nurse is successful and she comes “to the yard”, the life of the family and the daily routine, the process of rehabilitation of the patient will soon improve. Organizing the day-to-day activities of caregiving with the help of an experienced professional will allow people to be away with peace of mind, knowing that their loved one is under control.
If relatives are in the process of searching and choosing a caregiver and have not yet made their decision, they should know how to wipe bedsores at home. You can use traditional medicine or modern pharmaceutical drugs, but the best thing is the remedy that the doctor called to the patient will prescribe.
Here's how to properly treat bedsores; the algorithm of actions involves several directions:
- maintaining skin hygiene - wiping with wet wipes, removing traces of discharge;
- preventive treatment of diseased areas - light massage of the area around the redness or wound to stimulate blood circulation;
- treatment with medicinal agents - ointments, powders, special dressings.
The main objectives of the treatment of pressure ulcers
Specialists at the Yusupov Hospital rehabilitation clinic select medications against bedsores on an individual basis, after conducting a thorough examination and determining the stage of the disease. If conservative therapy is ineffective, surgical intervention may be prescribed.
Drug treatment of bedsores has the following objectives:
- stimulate blood circulation in affected tissues;
- eliminate necrotic masses from the surface of the affected skin area;
- activate regenerative processes in wounds.
In parallel with treatment, the rehabilitation clinic of the Yusupov Hospital carries out mandatory measures to prevent bedsores.
The best way to treat bedsores: several recommendations
More specifically: how can bedsores be treated? Saline solution, camphor alcohol for hygienic treatment. To dry the skin and stimulate local blood circulation, ointments and gels Iruksol, Actovegin, Solcoseryl, and ointments containing silver are used. You can dry the skin with Xeroform powder. Film bandages that are applied to bedsores and protect the skin from bacteria are very helpful. These are breathable films that, due to their transparency, allow one to observe the condition of bedsores.
However, there are as many treatment options as there are patients. Each person's body is individual. The professional knowledge of the doctor and nurse will provide complete information on how best to treat bedsores, but it happens that it will be necessary to use different means before the desired result is achieved. You can try cold water treatment - this will simultaneously keep the skin clean and cause contraction and then dilation of blood vessels, which improves local blood flow.
Treatment of bedsores at the Yusupov Hospital
The most favorable prognosis is for treatment of bedsores diagnosed in the early stages. In each case, the doctors at the Yusupov Hospital use an individual approach.
To treat bedsores of the first stage, camphor alcohol is used (every 2-3 hours it is necessary to wipe the areas of skin redness with alcohol) and alcohol tincture of Sophora japonica (treat the affected areas with tincture several times a day).
The use of wet wipes that have an antiseptic effect is not recommended, since newly formed bedsores must remain dry to prevent tissue death and the formation of necrotic masses.
At the second stage of bedsores, it is advisable to use medications:
- antiseptics (chlorhexidine);
- ointments (wound healing, anti-inflammatory, etc.);
- hydrogel dressings with a special gel that prevents the penetration of pathogenic bacteria into wounds;
- wound healing applications.
Despite the rather high cost of hydrogel wipes and applications, these products are in great demand in the treatment of bedsores, as they promote faster wound healing and significantly reduce the risk of complications.
The danger of the last stages of development of bedsores lies in the high probability of their transfer to healthy areas of the skin. To prevent this process at the third and fourth stages of the disease, it is advisable to perform surgical intervention to cleanse the wound of necrotic masses. After such an operation, procedures are begun to promote the healing of wounds and ulcers.
Nowadays, there are four groups of medications that need to be used in the later stages of development of pressure ulcers:
- necrolytic action: trypsin, collagenosin, etc.;
- regenerating action (promoting tissue restoration): ointment with Kalanchoe extract, vinylin, bepanthen, etc.;
- anti-inflammatory action: algofin, dexamethasone, etc.;
- means for stimulating blood circulation in affected areas: pyricarbate, etc.
The surgeon must select the most appropriate remedy for bedsores in each case. He develops an effective treatment regimen taking into account the patient’s health status, the individual characteristics of his body, as well as the degree of likelihood of developing severe complications.
Bedsores on the back: how to treat, an experienced nurse knows
The back is a vulnerable spot in bedridden patients. If bedsores appear on the back, how to treat them and how to prevent their development? Practice has shown that first of all it is necessary to reduce the pressure that this part of the body experiences. An anti-decubitus mattress will greatly ease the suffering of the patient. It is also necessary to change the position of the body of a lying person every two hours, turning him over on one side or the other, if possible on his stomach. Recommendations for treating wounds are the same as given above.
The problem of bedsores can be solved very effectively if a competent nurse is invited to care for the patient. The social support nursing service offers experienced medical personnel who know how to properly treat bedsores at home and will cure them in a short time.
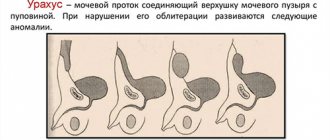
Risk category and place of formation
Bedsores occur in people who are permanently bedridden or use a wheelchair. Pathology occurs due to constant pressure on individual areas of soft tissue, which leads to disruption of local blood circulation and their gradual destruction.
The points of formation of bedsores are associated with the patient’s usual body position:
- When lying on your back, the area of the sacrum, heels, and elbows is affected. The occipital and scapular region is affected.
- Positioning on the side leads to injuries in the area of the femur, greater trochanter, and mastoid process. The area of the temporal bone is involved in the process.
- A sitting position causes compression of the tissues in the feet and shoulder blades. The ischial tuberosities are affected.
The risk of necrosis formation and the stage of pressure ulcers are determined using the Waterlow scale. The calculations take into account the general condition of the patient.
The appearance of redness, itching and pain with an unpleasant odor in places where soft tissues come into contact with hard surfaces indicates an infection. The patient's relatives should consult a doctor. Professional help is necessary if bleeding or foreign fluid appears from a bedsore.
Reasons for the development of bedsores
For a problem such as bedsores, the causes cannot be explained solely by the fact that a person is lying down. In fact, a lot depends on his condition and the characteristics of his care. The likelihood of developing pressure ulcers increases under the following conditions:
- large body weight. The stronger the pressure, the higher the risk of developing bedsores;
- too little body weight. When exhausted, the patient loses body fat as well as muscle. As a result, much less soft tissue remains between the bones and the skin - the bones put pressure on the skin, and bedsores form faster;
- friction against the skin of sheets and other materials and objects.
Reasons not related to pressure and friction
- Skin contact with urine and feces due to improper care.
- Anemia and diseases associated with impaired blood circulation in tissues.
- Low or high body temperature.
- Severe dryness or sensitivity of the skin. The more often irritation occurs, the more likely it is to develop bedsores.
- Reduced protein intake. Without protein, muscle mass decreases - as a result, the risk of developing bedsores increases.
All these reasons work both individually and in combination, but most often several factors act at once.
The most effective ways
Bee products
Since ancient times, the healing power of bee products has been used to treat skin diseases, wounds, trophic ulcers and bedsores.
Honey products
The bactericidal, antiviral and soothing properties of honey, which is a natural antibiotic, are very important for treatment:
- Honey releases hydrogen peroxide, which makes it an excellent antiseptic.
- In addition, taking honey and honey-containing preparations improves immunity and helps to recover.
Important! The antibiotic properties of honey increase as it is stored. It is better to take aged honey. It is believed that dark (buckwheat, heather, chestnut) and amber (sunflower, mountain, meadow) types of honey have the most pronounced antimicrobial properties.
To treat bedsores, an ointment is made from equal parts of finely grated raw potatoes and honey.
A gauze bandage is soaked in it and applied to the skin overnight. Honey dressing reduces dry skin, hyperemia (overflow of blood vessels and redness), pain, and promotes regeneration of the epidermis.
Reference! You can take a decoction of honey, fresh or dried plantain leaves internally.
How to treat bedsores with honey and potatoes is described in the video:
Stages and symptoms
Bedsores can develop quickly, but the formation of bedsores and ulcers occurs through four stages (each of which has its own symptoms):
- Stage 1
Redness of intact skin. It is slightly inflamed and may be painful, itchy and warm to the touch. You may also notice that the texture of your skin has changed slightly. At this stage, bedsores on the heels resemble a sunburn. This initial stage is difficult to detect in people with dark skin.
- Stage 2
In the second stage, the first signs of skin damage appear. They look like abrasions, blisters or small pits. The outer layer of skin is broken, red and painful. The surrounding tissue may be pale, red, and swollen. The upper layers of tissue, as the most damaged ones, begin to die and peel off. Bruising at this stage indicates suspicion of possible deeper tissue damage, involving fat or muscle tissue.
- Stage 3
Complete loss of tissue. The damage extends to the deeper layers of tissue in the heel. Crater ulcers are present and are susceptible to infection. Subcutaneous fat may be visible, but no bones, tendons or muscles are affected. The depth of a stage 3 ulcer depends on its anatomical location. Most often, bedsores on the heels progress to stage 3, until others notice them and begin to treat them.
- Stage 4
Loss of tissue, opening of bone and tendons. Ulcers with black edges spread to the heel bone and can lead to the development of osteomyelitis (a purulent-necrotic process in the bone). The exposed calcaneus is visible or directly palpable at the bottom of the trophic ulcer. These ulcers are extremely difficult to treat and may require many months and activities to heal. Therefore, preventing the development of ulcers should be taken more seriously.
Risk factors for pressure ulcer formation
Risk factors include the patient's high or very low weight, immobility, and poor care. But there are other additional points that are important to consider. There is also a risk of bedsores in people who have a low pain threshold or whose body reacts less well to pain due to painkillers. In such a situation, the prevention of bedsores consists of constantly inspecting the body, without waiting for the patient to complain of discomfort.
Another risk of bedsores is postoperative and other pain, which even forces a person with good mobility to constantly be in one position. Most often in such cases, the problem is detected at the first stage of bedsores, so it can still be corrected with less effort.
An additional problem may be taking medications that disrupt the water-salt balance in the body. If the instructions contain such data, the formation of bedsores can be avoided through careful prevention and constant monitoring of the situation.
Prevention of bedsores
Prevention of bedsores for bedridden patients is to keep the place where the patient lies dry, clean, constantly treat the skin, removing biological fluids, and avoiding excessive moisture. It is imperative to change the patient’s position, monitor his temperature and general well-being, provide high-quality nutrition with a sufficient amount of protein, and monitor his body weight.
There is no single recipe against bedsores, but if all the causes described earlier are eliminated, the risk of such a pathology will decrease many times.
Complications
Complications of bedsores (especially pressure ulcers) can be life-threatening and include:
- Phlegmon
Acute purulent inflammation of the skin and soft tissues. People with nerve damage (neuropathy) or a spinal injury often feel no pain in the area affected by inflammation and pressure sores. Cellulitis can cause severe intoxication and even general blood poisoning (sepsis).
- Heel ulcer
A chronic heel wound that does not heal for a long time significantly worsens the patient’s quality of life, as it leads to impaired support and walking function. A trophic heel ulcer can occur as a result of a bedsore, not only in spinal patients, but also in postoperative and post-resuscitation patients due to their prolonged immobilization.
- Damage to bones and joints
Infection from an ulcer can affect joints and bones. Infection in the joint cavity can cause general blood poisoning. Bone infections (osteomyelitis) can lead to destruction of the heel bone.
- Cancer
Wounds that do not heal over time can eventually develop into squamous cell skin cancer.
- Sepsis
General blood poisoning develops with weakened immunity, diabetes mellitus and other severe concomitant diseases and often causes death.
How to make an appointment with a therapist for a consultation
Treatment of such a pathology, regardless of the location of the bedsores, is a process that begins with a visit to the therapist. Depending on the stage of the problem, a visit to the surgeon may be necessary, especially if the wound needs to be cleaned. The opinion of a dermatologist is often required - the doctors of our clinic will advise you on all issues.
You can make an appointment with the specialists of JSC “Medicine” (clinic of Academician Roitberg) by calling +7 (495) 775-73-60, as well as using the registration form on the website.
At the bottom of the page you see a pop-up window with an envelope - there you can leave any questions and your contact information - we will contact you during business hours.