Sinusitis occurs as a complication after the most common runny nose, flu and other infectious diseases; treatment of sinusitis is performed by ENT doctors and therapists.
Sinusitis is an inflammatory disease of the mucous membrane of one or more nasal sinuses. For example, the well-known “sinusitis” is sinusitis of the maxillary sinuses. Sinusitis occurs as a complication after a runny nose, flu and other infectious diseases; sinusitis is treated by ENT doctors and therapists.
Quite often (50–60% of cases), sinusitis may have a different origin: it is not caused by a viral infection or acute respiratory infection, but has become a complication of caries of the teeth of the upper jaw and for other dental reasons. This is the so-called odontogenic maxillary sinusitis (sinusitis), the treatment of which belongs to the field of dentistry and has long been successfully performed by specialists from the Center for Maxillofacial Surgery and Implantology (Moscow).
Sinusitis is an inflammation of the mucous membrane of the maxillary sinus, resulting from an inflammatory process in one of the chewing teeth of the upper jaw or due to an infection that entered the maxillary sinus after tooth extraction. Sinusitis requires mandatory treatment in a clinical setting, which is carried out jointly by a dental surgeon and an ENT doctor. Odontogenic sinusitis (sinusitis) occurs in adults aged 30–50 years and is distinguished by the fact that it is not bilateral, but usually occurs only on the side of the diseased tooth.
Types of chronic sinusitis
According to the form of damage to the paranasal sinuses, they are distinguished: catarrhal , purulent , parietal hyperplastic , polypous , fibrous , cystic and mixed forms. For reasons of occurrence: rhinogenic , odontogenic , traumatic .
Acute and chronic sinusitis are among the most common diseases of the ENT organs. According to the literature, 5–15% of the adult population suffer from one form or another of sinusitis. Just like with acute sinusitis, the chronic form affects the mucous membranes of the paranasal sinuses. The difference between chronic sinusitis is the duration of its course - more than 3 months.
The nature of chronic sinusitis is recurrent, i.e. the symptoms either subside or, under certain conditions, resume. Exacerbation of chronic sinusitis is usually observed against the background of a sharp weakening of the immune system, the activity of unfavorable environmental factors and the progression of certain diseases of an infectious and viral nature.
Unfortunately, despite the many options for conservative and surgical treatment of acute sinusitis, they quite often become chronic and can cause intracranial and intraorbital complications.
Classification
When our otolaryngologists make a diagnosis, they use several classifications of the pathological condition, taking into account the severity: mild, moderate, severe.
Depending on where the inflamed area is located, the disease is classified differently:
- bilateral (the left and right sinuses belonging to the same type are affected);
- unilateral (symptoms are only on the right or left);
- polysinusitis (damage to more than 2 sinuses);
- monosinusitis (inflammatory process in one of the sinuses);
- rhinosinusitis (together with the sinuses, the nasal cavity also becomes inflamed);
- hemisinusitis (inflammation is one-sided, but several cavities are affected simultaneously);
- pansinusitis (all sinuses are affected, symptoms are typical for adult patients, treated with a set of measures).
Nature of inflammation:
- Catarrhal chronic sinusitis. Symptoms and treatment for this type of disease are specific. A mucous-serous fluid flows from the nostrils. Treatment is carried out without taking antibacterial drugs.
- Purulent. The deep layers of the paranasal sinuses are inflamed. Pus is released. Have to be treated with antibiotics.
- Chronic polypous sinusitis. It is a poorly studied type of disease. It affects people who suffer from bronchial asthma or are allergic to non-steroidal anti-inflammatory drugs.
Location of inflammation:
- The maxillary sinus, located in the maxillary bone (sinusitis). It is considered the most common location of the disease. Characterized by severe headache, weakness, photophobia, and a feeling of fullness in the cheeks.
- Frontal sinus (frontitis). Symptoms: fever, photophobia, pain in the forehead, swelling of the mucous membrane.
- "Frontal labyrinth" (ethmoiditis). Symptoms include swelling of the eyelids, high body temperature, pressing pain in the nasal root, and decreased sense of smell.
- Sphenoid sinus (sphenoiditis). It is characterized by unpleasant sensations in the occipital region and eye sockets, and constant headache.
Considering the duration of the disease, there are three forms:
- acute (caused by influenza, infections, prolonged rhinitis);
- subacute;
- chronic.
Causes of chronic sinusitis
The following factors contribute to the development of chronic sinusitis:
- Anatomical disorders of the nasal cavity, changing aerodynamics, the passage of air through the nasal cavity and paranasal sinuses. The most common pathological anomaly is a deviated nasal septum, congenital or acquired as a result of injury.
- Enlargement (hypertrophy) of the inferior turbinates, characteristic of chronic rhinitis, also creates an obstacle to the air stream.
- Pathologies of tooth roots. Often, after tooth extraction, the maxillary sinus becomes infected with bacterial flora from the oral cavity. Very often, the cause of odontogenic sinusitis (inflammation of the nasal sinuses resulting from diseases of the teeth of the upper jaw) is the filling material that got into the maxillary sinus when filling the dental canals. Such foreign bodies create favorable conditions for the development of fungal flora (mycetoma).
- Prolonged hypothermia of the body and nose, throat, pharynx.
- Allergic alertness of the body.
- Long-term course of acute respiratory infections and other viral or infectious diseases.
- Weakening of general immunity.
Differences between chronic and acute rhinosinusitis
Chronic rhinosinusitis is characterized by a long course and usually occurs without a pronounced increase in temperature. An acute condition is always accompanied by high fever, begins unexpectedly and has more pronounced painful symptoms.
The main symptoms of chronic rhinosinusitis:
- runny nose;
- impaired nasal breathing, feeling of swelling in the nose;
- postnasal drip (accumulation or drainage of mucus in the throat, the need to cough up mucus);
- swelling and swelling of the soft tissues of the cheeks, eyelids, nose, forehead;
- deterioration (absence) of smell and taste.
Also, with chronic inflammation, a cough may appear with radiating (radiating) pain in the ear, upper jaw, and teeth.
Other symptoms of chronic rhinosinusitis:
- otalgia (ear pain);
- pain spreading to the upper jaw and teeth;
- sore throat;
- cough (may get worse at night);
- halitosis (putrid odor);
- fatigue;
- nausea.
Signs of chronic sinusitis (depending on the form of sinusitis):
- long-lasting runny nose with periods of improvement;
- persistent nasal congestion;
- headache;
- decreased sense of smell;
- postnasal drip - drainage of mucus from the nasopharynx into the oropharynx;
- purulent discharge from the nose with an unpleasant odor, felt at a distance from the patient, is observed, as a rule, with odontogenic sinusitis;
- asymptomatic (possible, for example, with small cysts of the maxillary sinuses);
- persistent nasal voice in the presence of polyps in the nasal cavity.
Read also: Questions and answers on the topic - Treatment of nasal diseases
Acute sinusitis is an inflammation of the sinuses (sinuses) surrounding the nasal cavity that lasts up to 4 weeks.
It usually manifests as nasal congestion, headache, pain or tension in the face.
Most often, acute sinusitis occurs during or immediately after a cold. Less commonly, it can be caused by a bacterial or fungal infection or allergy.
In most cases, antibiotics are not required (unless symptoms of sinusitis persist for more than 7 days in adults and more than 10 days in children).
Synonyms Russian
Acute rhinosinusitis, acute sinusitis, acute sinusitis.
English synonyms
Acute sinusitis, Acute rhinosinusitis, Acute maxillary sinusitis.
Symptoms
There is no single sign by which one can accurately determine that a patient has sinusitis, so when diagnosing this disease, a doctor takes into account all the symptoms and the history of the development of the disease.
The most typical symptoms of sinusitis are:
- nasal congestion,
- headache,
- discharge from the nose, light or yellow, green in color, as well as flowing down the back wall of the throat,
- decreased sense of smell,
- pain, tension, swelling in the facial area, corresponding to the affected sinus: around the eyes, nose, forehead,
- pain in the upper jaw, teeth,
- bad breath,
- cough, especially at night,
- increase in body temperature,
- weakness.
General information about the disease
Sinusitis is an inflammation of the sinuses (sinuses) surrounding the nasal cavity. It is called acute in cases where recovery occurs no more than 30 days from the onset of the disease, subacute - when it lasts from 4 to 12 weeks. If the symptoms of the disease persist without interruption for more than 3 months, it is chronic sinusitis.
Sinusitis is very common at any time of the year, but it is more common in winter.
In fact, it is more correct to talk about rhinosinusitis (from the Greek rhinos - “nose”), since inflammation in the sinuses is always accompanied by inflammation in the nasal cavity itself, which is called rhinitis, or, more simply, a runny nose.
The paranasal sinuses are air-filled cavities in the bones of the skull that connect to the nasal cavity. They are also called paranasal sinuses.
There are 4 groups of paranasal sinuses, and according to their damage, the following types of sinusitis are distinguished:
- sinusitis - inflammation of the maxillary (maxillary) sinuses, located on the right and left sides of the nasal cavity, in the upper jaw,
- ethmoiditis - inflammation of the ethmoid sinuses located between the eyes,
- frontal sinusitis - inflammation of the frontal sinuses located above the eyes
- sphenoiditis is an inflammation of the sphenoid (main) sinus, which is located behind the nasal cavity, close to the base of the brain.
Several sinuses can be affected at the same time, but the maxillary sinuses are most often affected.
The exact function of the sinuses is unknown; it is assumed that they, among other things, are involved in warming and humidifying the inhaled air. They are covered with a mucous membrane with cilia, which produces mucus. This mucus, due to the movement of the cilia, is removed through small holes that connect the sinuses with the nasal cavity. Normally, mucus moves in only one direction, which keeps the sinuses sterile, despite the fact that the nasal cavity connected to them is inhabited by bacteria.
If the mucus exit holes are blocked or the cilia of the sinus mucosa are disrupted, the fluid stagnates and fills the sinuses, causing symptoms of sinusitis: nasal congestion, headache. The accumulation of fluid in the sinuses becomes a favorable environment for the proliferation of bacteria, which makes the disease more severe and complications can develop.
Causes of acute sinusitis
- Infection
- Viral. Most often, acute sinusitis occurs during or immediately after a cold. A cold is accompanied by inflammation of the sinus mucosa in most patients, but the addition of a bacterial infection is noted in less than 1% of cases.
- Bacterial. Much less commonly, acute sinusitis is caused by bacteria. Most often they complicate viral inflammation, although they can also be the primary cause of sinusitis. Sinusitis is considered to be caused by bacterial inflammation if symptoms persist for 7 days or more in adults and 10 days or more in children.
- Fungal. Fungi can cause extremely severe, life-threatening sinusitis. People with weakened immune systems, such as HIV-infected people, are most susceptible to fungal infections.
- Allergy. Swelling of the nasal mucosa due to allergies (for example, to pollen) can block the flow of mucus from the sinuses.
- Anatomical causes, in particular a deviated nasal septum, consequences of injury, or polyps - abnormal growths of the mucous membrane inside the nose.
- Chronic heartburn.
- Chemical agents, including those contained in tobacco smoke, can impair the functioning of the cilia of the sinus mucosa.
Sinusitis can lead to the following complications.
- Meningitis. In this case, the infection spreads to the membranes of the brain.
- Abscesses inside the skull are purulent foci that cause an increase in temperature to 39-40 degrees and severe pain.
- Eye complications. When inflammation spreads to the orbital area, vision may be impaired up to complete blindness.
- Chronic sinusitis, indicated by persistence of symptoms for more than 12 weeks.
Who is at risk?
- Having a deviated nasal septum, polyps in the nasal cavity
- Suffering from allergic rhinitis.
- Suffering from chronic heartburn.
- HIV-infected and other patients with reduced immunity.
- Active and passive smokers.
Diagnostics
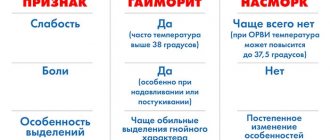
The diagnosis of “acute sinusitis” is made based on a study of all symptoms and the course of the disease. There are no specific signs that alone would accurately indicate sinusitis. It is important to distinguish it from the common cold, which can also present with a runny nose and nasal congestion.
Most sinusitis is caused by viruses and does not require antibiotics (as they do not treat viral infections), while bacterial sinusitis is treated with antibiotics. This is why it is important to distinguish between viral and bacterial sinusitis. In practice, however, this is extremely difficult to do, since there are no clear criteria for the addition of a bacterial infection. You need to know that thick, purulent yellow or green nasal discharge is not a sign of a bacterial infection and is often observed with the common cold, which is caused by viruses. Currently, bacterial and viral sinusitis are conventionally defined by the duration of the disease. If symptoms persist for more than 7 days in adults and more than 10-14 days in children, sinusitis is considered bacterial.
Usually no additional examination is required, but in controversial cases it can be useful in making a correct diagnosis.
Laboratory research
- General blood analysis. An increased number of leukocytes may indirectly indicate the bacterial nature of sinusitis.
- Erythrocyte sedimentation rate (ESR). It can be significantly increased with severe bacterial inflammation.
- C-reactive protein is an indicator characterizing the activity of inflammation. With sinusitis it may be elevated, but this is not specific to this disease.
- Rhinocytogram - taking a smear from the nasal cavity, followed by staining and examination under a microscope. Based on the ratio of cells in this analysis, one can judge the allergic or infectious nature of sinusitis, although the reliability of the results is not very high.
- Sowing the contents of the paranasal sinuses. In case of prolonged sinusitis or ineffectiveness of antibiotics, as well as in patients with reduced immunity, contents can be taken from the paranasal sinuses for subsequent culture on nutrient media, where bacteria multiply so that they can be recognized. The most reliable results are obtained with direct puncture of the sinus.
Other research methods
- X-ray of the skull. Allows you to identify thickening of the sinus mucosa or detect fluid in them. Currently, however, it is not recommended because its reliability in diagnosing sinusitis is quite low.
- Computed tomography (CT) of the paranasal sinuses. The most reliable way to study for sinusitis. Particularly useful in case of complications.
- Endoscopic examination of the sinuses. A thin tube is inserted into the nasal cavity to visually assess the condition of the paranasal sinuses. This method can be informative for fungal infections, tumors, polyps, and developmental abnormalities.
Treatment
A disease with moderate symptoms does not require seeing a doctor.
Most patients recover without antibiotics. Treatment in this case includes the use of vasoconstrictors (no more than 3-5 days), rinsing the nasal cavity, inhaling warm steam, warm compresses on the sinus area, painkillers, and taking a sufficient amount of fluid.
Antibiotics are generally only required for severe illness, when bacterial infection is clearly suspected, or when symptoms persist for a long time, and are usually administered for at least 10 days. In approximately 10-15% of patients they do not help, then a puncture of the sinus followed by rinsing it can be used. It may also be indicated if complications develop.
In case of severe purulent complications, operations are performed aimed at eliminating the purulent focus, simultaneously with intravenous antibiotics.
Prevention
- Avoid contact with people with colds, wash your hands before eating.
- Get an annual flu vaccination.
- Proper treatment of allergic rhinitis (incorrect treatment is, for example, uncontrolled and prolonged use of vasoconstrictor drops).
- Use a humidifier at home and ventilate the room (moisturizing the nasal passages increases the resistance of tissues to microbes).
- Do not smoke, avoid contact with tobacco smoke.
Recommended tests
- General blood analysis
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein, quantitative
- Microscopic examination of a smear from the nasal mucosa
- Culture of flora with determination of sensitivity to antibiotics
Literature
- Dan L. Longo, Dennis L. Kasper, J. Larry Jameson, Anthony S. Fauci, Harrison's principles of internal medicine (18th ed.). New York: McGraw-Hill Medical Publishing Division, 2011.
Complications of chronic sinusitis that occur without timely and adequate treatment:
- orbital, causing inflammation of the eye tissue and membranes of the eyeball with subsequent loss of vision;
- intracranial, the most common of which is meningitis, inflammation of the meninges. This disease, as a complication of sinusitis, most often occurs with inflammation of the ethmoid labyrinth and sphenoid sinus. With frontal sinusitis (inflammation of the frontal sinus), an epidural abscess or, less commonly, a subdural brain abscess may develop.
- osteomyelitis of the upper jaw: the spread of inflammation deeper can lead to bone damage and the development of osteomyelitis.
Sinusitis in children
Sometimes sinusitis in children is more difficult to see than sinusitis in adults. The disease usually develops after an infection: influenza or sore throat, and is often accompanied by otitis media. The symptoms are somewhat blurred and appear weaker than in adults. Here are the main ones:
- purulent or mucous discharge from the nose;
- general weakness, malaise;
- pungent odor from the mouth.
With sinusitis in children, one side of the face is often inflamed. While sinusitis in adults is often accompanied by headaches, headaches in children are extremely rare.
Diagnosis of chronic sinusitis
- collection of patient complaints and anamnesis (medical history);
- rhinoscopy, or examination of the nasal cavity in the traditional way using a reflector;
- An endoscopic examination of the nasal cavity, which helps the doctor see areas of the nasal cavity that are hidden during normal examination and identify abnormalities that contribute to the development of sinusitis. In addition, the patient sees with his own eyes on a video monitor attached to the endoscope the condition of his nasopharynx, nasal mucosa, abnormalities in the development of the nasal septum and other structures;
- X-ray, computed tomography of the paranasal sinuses is a highly informative research method that absolutely clearly shows all the sinuses of the nose, their structural features, the condition of the mucous membrane in the sinuses, the presence of fluid, cysts or polyps in them. The method also makes it possible to assess the condition of the dental system for the involvement of the upper jaw teeth in inflammation in the sinuses;
- endonasal diagnostic puncture (puncture) of the maxillary sinuses;
- if necessary, the ENT doctor refers the patient to a consultation with a dental surgeon.
Read more about the methods for diagnosing sinusitis in our clinic here.
Symptoms and signs of manifestation
The clinical picture resembles a cold. Therefore, many people visit the doctor when the disease is already advanced. The following symptoms should be considered:
- duration of runny nose more than 2 weeks;
- the discharge has a yellow-green tint (pus);
- decreased sense of smell, difficulty breathing;
- pain in the head, intensifying when a person tilts his head;
- in the projections of the sinuses there is a feeling of distension;
- fever, increased body temperature (acute form).
Possible complications
As with other forms of inflammation of the paranasal sinuses, ethmoiditis can lead to complications such as:
- Loss of smell - anosmia.
- Eye infections (diseases), including blindness.
- Bone infections – osteitis, osteomyelitis.
- Cyst formation.
- Sepsis (blood poisoning).
- Increased risk of asthma.
- Brain (membranes) – meningitis, encephalitis, etc.
- Heart diseases – pericarditis, endocarditis, etc.
Although many of the risks mentioned are rare, it is important to get timely treatment in any case. Even with the acute form of ethmoiditis, it is important to treat inflammation at an early stage, and not lead to a chronic course.
Prevention
Preventive measures for chronic odontogenic sinusitis include:
- improving the functioning of the immune system;
- timely elimination of colds and runny nose;
- maintaining a healthy lifestyle;
- hardening;
- no contact with substances that cause an allergic reaction;
- daily exposure to fresh air;
- taking minerals and vitamins;
- dental care;
- use of an air humidifier (room temperature should be 19-22 degrees Celsius, humidity – 60%).
If you have snot, experts recommend rinsing your nose with saline solution, monitoring the duration of the runny nose and the shade of the secretion.
Treatment
Treatment of acute ethmoiditis
Conservative therapy is the main treatment for acute ethmoiditis . In the acute period, the following are prescribed:
- Intranasal vasoconstrictors (sprays or drops) – up to 5 days,
- Mucolytic agents - to soften the contents of the ethmoid sinus,
- Systemic antibacterial drugs - taking antibiotics. Injectable forms may be recommended.
Additionally, nasal sprays with anti-edematous and anti-inflammatory effects are recommended.
Surgical correction of the nasal cavity is recommended after the acute period of ethmoiditis has stopped.
Treatment of chronic ethmoiditis
If chronic ethmoiditis occurs, surgical treatment . It is primarily necessary to remove the contents of the sinus, as well as to correct the anatomical structures of the nasal cavity that provoke this condition.
The most effective method of this type of treatment is endoscopic sinus surgery or ethmoidotomy. This method not only reduces the risk of postoperative complications, but also significantly reduces the recovery period and the patient’s hospital stay.
Sign up for a consultation