Why are hormone tests done?
The content of the article
Almost all processes that occur in the human body are controlled to one degree or another by hormones - elements constantly produced by the secretory glands. All changes directly depend on the concentration of these substances in the body - maturation, growth, pregnancy, and so on. Even minor disruptions in the functioning of the secretory glands lead to a lack or excess of their formation, which results in pathological processes. Constancy of hormonal levels is impossible, since various hormonal elements and structures in the body are constantly being formed and destroyed.
It is to identify and eliminate such disorders that studies are carried out - on hormones. Despite the fairly high price of the tests,
It is necessary to carry out all studies recommended by the doctor.
find out what hormone tests
are needed in order to keep the intensity of substance formation under control in this article.
When do you need to donate blood for hormones?
Planning a pregnancy is an important and responsible stage that will require a full medical examination from future parents. Some couples will definitely need to undergo hormone tests.
Direct indications for their implementation are the following factors:
- The age of the spouses is over 35 years.
- Irregular menstruation in a woman.
- Failure to conceive within a year of regular sexual activity without contraception.
- History of miscarriage or miscarriage.
- Suspicion of the presence of benign and malignant formations.
- Obesity in one of the partners.
- Decreased libido.
Indications for hormone tests
As a rule, a patient is prescribed a hormone test due to the presence of the following characteristic symptoms:
- increased blood pressure;
- cardiopalmus;
- weight gain;
- menstrual irregularities;
- mood swings;
- difficulties with conceiving and so on.
Most often, these tests are prescribed to patients when various endocrine pathologies are suspected; they are needed to clarify or confirm a preliminary diagnosis.
How to get examined?
All examinations are divided into planned and urgent. A routine examination is also carried out in the complete absence of symptoms, when screening is simply necessary. For example, due to iodine deficiency in many regions, all residents should have their thyroid-stimulating hormone tested periodically. If there are deviations from normal values, you should consult an endocrinologist. He will prescribe a list of further examinations to clarify the diagnosis.
If the patient has complaints, this is an indication for urgent examination. But not in every case, hormonal imbalance has external manifestations. Therefore, you should carefully monitor your health if the following symptoms appear:
- swelling,
- pigmentation,
- brittle nails,
- constant heat or cold,
- dry skin,
- hypo- or hypertension,
- obesity or malnutrition,
- myalgia,
- joint pain,
- constant fatigue
- short or tall,
- excessive sleepiness or insomnia,
- decreased performance.
The reason for consulting an endocrinologist is menstrual irregularities. Also, special attention should be paid to the control of sex hormones during menopause.
What tests are done for hormones?
To make or confirm a patient’s diagnosis, a doctor may need to perform the following hormonal tests:
- hormones
(
somatotropic,
adrenocorticotropic, TSH,
thyroid-stimulating,
follicle-stimulating, luteinizing hormone, prolactin); - thyroid hormones (calcitonin, T3, T4, antibodies);
- pancreatic hormones (insulin);
- adrenal hormones (cortisol, norepinephrine, adrenaline, aldosterone, progesterone,
ACTH); - sex hormones (estrogens
, that is, progesterone, estradiol, hCG, and testosterone).
- tumor markers (PSA, AFP, REA);
- adrenal hormones (progesterone,
cortisol, ACTH); - prenatal diagnosis.
When you need to take hormone tests and when not, the doctor decides.
What is a hormonal study?
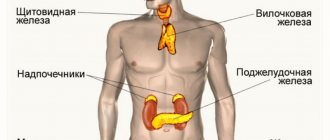
Hormones are different in chemical structure, but equally highly active biological substances secreted by the endocrine glands (thyroid, parathyroid, thymus, adrenal glands, pituitary gland, hypothalamus and others) directly into the circulatory system.
A hormonal blood test can be prescribed by a general practitioner and specialized doctors: endocrinologist, gastroenterologist, gynecologist, neurologist, urologist and others, depending on the suspicion of dysfunction of certain organs.
Tests for basic hormones
The tests most often performed in St. Petersburg are listed below.
- Follicle-stimulating hormone (FSH)
in women is responsible for the formation of estrogen and the growth of follicles in the ovaries.
The critical level of FSH, which is reached in the middle of the cycle, ensures ovulation. In men, this substance is responsible for the concentration of testosterone in the blood, the maturation of sperm, and provides male strength. Deciphering this analysis
plays an important role in determining the causes of infertility. - Luteinizing hormone or LH
in men increases testosterone levels in the blood, providing conditions for sperm maturation.
In women, it is responsible for the secretion of estrogen, the formation of the corpus luteum, and ovulation. The ratio of FSH and LH in the body of patients, compliance with the norm
, is an important point in the examination for infertility. - Prolactin takes part in ovulation and activates lactation after childbirth. With a decreased or increased concentration of prolactin, the development of the follicle may stop, and as a result, the woman does not ovulate. Also, anabolic processes in the body depend on this substance (activates protein synthesis), it produces an immunomodulatory effect. In men, excess prolactin can lead to impotence, decreased libido, and infertility. how to do this test correctly
. - Progesterone is a prerequisite for the normal course of pregnancy, as well as for its occurrence.
- Testosterone is secreted in a woman’s body by the adrenal glands and ovaries; excess can cause early miscarriage and improper ovulation. A reduction in the level of testosterone in a man’s blood reduces the quality of sperm and causes erection problems. Proper preparation
for this study is important - Thyroid-stimulating hormone (TSH) is tested to rule out or confirm a patient's thyroid dysfunction. Detection of antibodies to this substance makes it possible to predict malfunctions of the thyroid gland.
Interpretation of test results
can only be carried out by a doctor, since it is difficult to understand without professional knowledge. The answer to the question of how many tests are done depends on the specific analysis.
Preparation and conduct of the study
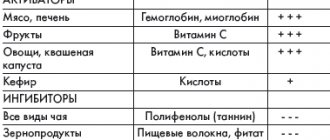
Biomaterial for hormonal blood tests is given in the morning, on an empty stomach. In order to avoid distortion of the results, it is recommended to exclude increased physical activity, alcohol and drugs that affect hormonal levels one or two days before taking the tests (you should consult your doctor about this). It is advisable not to smoke two hours before taking blood. If these conditions are met, reliable results can be obtained.
Decoding the results of hormonal studies: norm and pathology
Blood and urine are used to conduct hormonal studies. Hormone levels are usually indicated in U/l, IU/l, U/ml. In public health facilities, alternative units may be used: nanograms or picomoles per liter or milliliter of blood plasma. The content of hormones in urine is measured in daily amounts - micromoles and micrograms per day.
Pituitary
The pituitary gland is an endocrine gland weighing half a gram and the size of a little fingernail, which synthesizes the most important hormones for the body: growth (responsible for the growth of the body at a young age) and regulatory (coordinating the activity of the sex and thyroid glands, as well as the adrenal glands).
The anterior lobe of the pituitary gland synthesizes six tropic hormones, including:
Somatotropic hormone (STH)
- a key stimulator of amino acid (protein), carbohydrate (energy) and lipid (fat) metabolism, a growth hormone responsible for the normal physical development of the human body. Its normal ranges fluctuate seriously until puberty. From the age of 19, the GH norm for men and women is up to 5 ng/ml[1].
Somatomedin-C (insulin-like growth factor I - IGF-I)
- a neuropeptide modulator consisting of 70 amino acids, its functions are similar to insulin. It is an intermediary (prohormone) of the action of growth hormone and plays an important role in the aging process of the body. Its reference values are the same for women and men. Normal indicators increase significantly during puberty and gradually decrease towards old age. Thus, the norm for children under three years of age is 28–131 ng/ml, by 10–13 years of age — 95–473 ng/ml, by 13–16 years of age — 213–654 ng/ml. Then the indicators begin to decrease: from 16 to 18 years old, the norm is 195-511 ng/ml, from 18 to 22 years old - 146-472 ng/ml, at 22-35 years old - 121-388 ng/ml, 35-40 years old - 111–284 ng/ml, from 40 years of age – 89–269 ng/ml[2].
Sex (gonadotropic) hormones of the pituitary gland and prolactin:
- Follicle-stimulating hormone (FSH)
stimulates sperm production in men and follicle formation in women. Regulates sexual desire and reproductive function in both sexes. Monitoring FSH levels is extremely important during pregnancy. During puberty and during certain phases of the menstrual cycle, FSH reference values vary depending on age and gender. For women 18–60 years old, the norm is 1.70–21.50 mIU/ml, for men of the same age – 1.50–12.40 mIU/ml. After menopause, normal values for women range from 25.80 to 134.80 mIU/ml. In the first week of pregnancy, the FSH value may be less than 0.2 mIU/ml. - Luteinizing hormone (LH)
works in conjunction with FSH, so it is necessary to compare the hormone values and establish the LH/FSH proportions. In women it affects ovarian function and tarragon production, in men it affects the testicles and testosterone synthesis, spermatogenesis. For men, reference values are 1.14–8.75 mU/ml. The norm in women depends on the phase of the cycle: follicular - up to 15.00 mU/ml, ovulatory - 21.90-56.60 mU/ml, luteal - 0.61-16.30 mU/ml, postmenopausal - 14.2- 52.30 mU/ml[3]. - Prolactin (luteotropic hormone)
stimulates the proliferation of the mammary gland and milk secretion. In infants, prolactin levels are high (78–1705 mU/ml in boys and 6.3–1995 mU/ml in girls). But by the fourth to eighth week, the hormone content decreases significantly. And from year to year the normal range is 73–407 and 109–557 mU/ml for men and women, respectively.
Thyroid-stimulating hormone (TSH).
Controls the functioning of the thyroid gland, “forcing” it to produce triiodothyronine (T3) and thyroxine (T4), as well as increasing the number and size of thyroid cells and their absorption of iodine, the synthesis of proteins, nucleic acids and phospholipids. Its secretion is subject to daily fluctuations: the minimum of the hormone occurs at 17-18 hours of the day, the maximum at 2-4 hours in the morning, after 6-8 hours in the morning the production of TSH begins to fall. Reference values for TSH decrease from birth until puberty, after which they remain unchanged: from the age of 20, the hormone norm is 0.3–4.2 mU/l[4].
Thyroid-stimulating hormone Thyroid-stimulating hormone is the main regulator of the thyroid gland, the content of which affects the functioning of various body systems. Testing the level of TSH in the blood THERE ARE CONTRAINDICATIONS. YOU MUST CONSULT A SPECIALIST
Adrenocorticotropic hormone (ACTH).
The target organ for the hormone is the adrenal glands. ACTH plays an important role in lipid, amino acid and energy metabolism, stimulating fat burning, protein and glucose absorption, and insulin production by the pancreas. Like TSH, adrenocorticotropic hormone is strictly dependent on the circadian rhythm; its concentrations in the blood plasma vary over a wide range, reaching a maximum at 6–8 am and a minimum at 21–22 pm. The normal ACTH value is considered to be 7.2–63.6 pg/ml[5].
Beta-lipotropic hormone is also formed in the anterior lobe of the pituitary gland.
, which is involved in the formation of ACTH and is directly involved in lipolysis (the process of fat breakdown) and energy release.
The middle lobe of the pituitary gland produces melanocyte-stimulating hormones, as well as gamma-lipotropic hormone. Hormones synthesized by the hypothalamus accumulate in the posterior lobe of the pituitary gland. The most studied hormones of the posterior lobe of the pituitary gland are vasopressin, or antidiuretic hormone (ADH), and oxytocin.
.
ADH ensures the reabsorption of water from the kidneys, that is, its return to the body, and also narrows the arterioles, resulting in increased blood pressure - thus the hormone protects the body during a sharp jump in blood pressure, preventing large blood losses and normalizing blood pressure.
Oxytocin selectively acts on smooth muscles, provoking their contraction. In this regard, it is important during childbirth, lactation and breastfeeding. Due to its psychotropic effect, oxytocin helps in building trusting relationships within a social group; deficiency of this hormone is associated with the development of autism[6].
Promotions and special offers Special offers and discounts on diagnostic laboratory services allow you to save on medical examinations. View current promotions THERE ARE CONTRAINDICATIONS. YOU MUST CONSULT A SPECIALIST
Preparing for hormone tests
Assessing a patient’s hormonal background is an important point in diagnosing many diseases. What hormone tests are needed in a particular case is determined by the doctor. The patient is only required to comply with the rules for preparing for research, which are given below.
In order to get a reliable picture as a result of hormonal tests, the patient must take into account the basic rules for preparing for them.
- For a few days, heavy physical activity is excluded, situations that cause nervous tension are prohibited.
- Two days before the study you need to give up alcoholic beverages.
- Two hours before taking biological material, you should stop smoking.
- The analysis is carried out in a state of absolute calm, therefore, you need to sit and relax 15 minutes before it is carried out.
- Distortion of the results is possible if the patient is taking medications; you should definitely discuss this situation with your doctor.
Some types of hormonal tests
It is advisable to carry out only on specific days of the cycle (if we are talking about a woman), the doctor will definitely warn you about this.
A man can take hormone tests
any day.
To obtain a correct interpretation of the results of hormone tests, strict adherence to the following rules is necessary.
- It is advisable to donate blood in the morning (8-11). The analysis must be carried out on an empty stomach, which means that at least 8 hours must pass between the collection of biological material from the patient and the last meal. At the same time, it is not prohibited to consume water in any quantity; it does not in any way affect the study on the concentration of hormones.
- On the eve of the study, it is recommended to limit yourself to a light dinner; it is advisable to avoid fatty foods in order to avoid distorting the results.
- Approximately two days before the hormone test, doctors advise you to stop drinking alcohol. Excessive physical activity is also prohibited.
- The use of medications is not recommended. In some cases, you can take medications after first discussing this with your doctor. It is advisable to conduct the study before drug treatment or two weeks after its cessation.
- About two hours before the test is due, you need to stop smoking cigarettes. You should also not drink coffee, tea, juice, or sparkling water. There should be no physical stress (climbing stairs too quickly, running), as well as emotional arousal. It is advisable to relax and rest a little 15 minutes before the analysis.
- Donating blood after an instrumental examination, various physiotherapeutic procedures, ultrasound or X-ray examination, massage and other medical procedures is not recommended; you need to wait a certain time.
- If laboratory parameters are checked over time, it is preferable to carry out repeated studies under the same conditions, that is, at the same time of day, in the same laboratory, and so on.
- In some cases, laboratory analysis of hormones
must be carried out strictly on certain days of the cycle.
The attending physician will warn the patient about this. As a rule, we are talking about tests for hormones of the reproductive system.
In order for anal analysis to be carried out on the main hormones
turned out to be as informative as possible, it is very important to prepare for them correctly.
How to interpret hormone tests correctly
The study of hormonal levels is necessary for the effective detection of many diseases: thyroid diseases, infertility, and so on. In addition, they are carried out to confirm the presumptive diagnosis. You can try to independently decipher a blood test for hormones
, however, it is worth leaving the final diagnosis to a specialist.
When conducting most studies and determining the norm and deviations from it, factors such as the age and gender of the patient should be kept in mind. When assessing the functions of sex hormones in female patients, it is necessary to take into account the specific phase of the menstrual cycle. Therefore, it is advisable to take blood for hormones from women of reproductive age only on certain days of the cycle.
Pregnancy also seriously changes hormonal levels. At different stages of expecting a baby, the levels of hormones in the body become different. For example, in the first trimester, more than a third of pregnant women have a decrease in thyroid-stimulating hormone.
In the first trimester, the level of human chorionic gonadotropin jumps, and so on.
Since hormones have a systemic effect, their regulation is an unusually complex process; indicators are often affected by concomitant diseases (chronic and acute) and the use of medications. And finally, it is important to take into account such aspects as the ecology of the patient’s specific area of residence and the general condition of his body. Therefore, the interpretation of the results should be left to the doctor.
How to decipher a hormone test yourself
Below are the principles of an approximate decoding of tests for the main hormones.
- Testosterone
is produced in the body of women and men, for the latter it serves as the main sex
hormone
. In a man's blood, the normal level of testosterone is 2-10 ng/ml. In women, this parameter is normally in the range of 0.2-1 ng/ml. In men, excess testosterone levels may indicate early puberty and testicular tumors. A reduction in this indicator negatively affects the quality of sperm and may be a sign of dangerous liver or kidney diseases. If the concentration of this substance in the female body exceeds the norm, this can lead to a miscarriage. - Estrogens belong to the female sex hormones: estradiol, progesterone. These substances are responsible for the menstrual cycle, fertilization, guarantee the preservation of the fetus and the development of the egg. Their content in the body is determined by the phase of the cycle. Postmenopause - 51-133 pM/l, luteal phase - 439-570 pM/l, follicular phase - 198-284 pM/l - these are the normal test results for estradiol.
For progesterone, the following indicators are normal: postemnopause - 1-1.8 nM/l, luteal phase - 23-30 nM/l, follicular phase - 1-2.2 nM/l. If the levels of these substances exceed the norm, this may indicate a tumor of the adrenal cortex, ovaries, pregnancy, or cirrhosis of the liver. A contraction may indicate sclerosis, underdevelopment of the ovaries, the threat of abortion, or lack of ovulation. - Follicle-stimulating hormone
is produced by the pituitary gland and activates the development of follicles in women and seminiferous tubules in men. For the female body, the norm is 4-150 units/l (the phase of the menstrual cycle plays a role), for the male body – 2-2\10 units/l. The concentration in the body of this substance increases when sperm production fails, during menopause, or when ovarian function decreases. FGS levels also fall under the influence of hormonal contraceptives, with prostate cancer, and during pregnancy.
- LH or luteinizing hormone activates the production of sex hormones in women and men. Normally, for women the figure is 0.61-94 units/l (the figure depends on the phase of the cycle), for men – 2-9 units/l. Taking estrogen in large doses can reduce the indicators, while malfunction of the gonads can increase it.
- Prolactin in a woman’s body controls the development of the mammary glands, and after the birth of a child, the formation of breast milk. Its normal value during pregnancy is 500-10,000 mIU/l. Depending on the stage, the indicator gradually increases. This hormone is also present in men - 58-475 mIU/l is considered normal.
- of thyroid-stimulating hormone
in the body is assessed to determine the condition of the thyroid gland. An increase in indicators is a signal of insufficient thyroid function. Their reduction indicates an oversupply. A value in the range of 0.2-3.2 MIU/l is considered normal.
A comprehensive study of steroid hormones (mineralocorticoids, glucocorticoids and sex hormones), used in the diagnosis of “virilizing syndromes” (polycystic ovary syndrome, tumors of the gonads and adrenal glands, Cushing’s disease, congenital hyperplasia of the adrenal cortex), as well as in assessing the function of the hypothalamic-pituitary- adrenal system.
Synonyms Russian
Steroid hormones, mineralocorticoids, glucocorticoids and sex hormones.
English synonyms
Steroid hormones, Serum, Mineralocorticoids, glucocorticoids and sex hormones.
Research method
High performance liquid chromatography-mass spectrometry (HPLC-MS).
Units
ng/ml (nanograms per milliliter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 12 hours before the test.
- Avoid taking estrogens and androgens 48 hours before the test.
- Avoid physical and emotional stress for 24 hours before the test.
- Do not smoke 3 hours before the test.
General information about the study
The synthesis of steroid hormones is a multi-step process during which cholesterol (cholesterol), under the action of several enzymes, is converted into active compounds that perform various functions. Depending on their physiological effects, steroid hormones are divided into mineralocorticoids, glucocorticoids and sex hormones. Mineralocorticoids and glucocorticoids are formed only in the adrenal cortex, while sex hormones are produced both in the adrenal cortex and in the gonads and adipose tissue. The body reaches a certain concentration and ratio of steroid hormones, which is necessary for the normal development of the reproductive system and sexual characteristics, maintaining water-electrolyte balance and vascular tone, as well as adaptation to environmental factors. Violation of this ratio leads to the development of a wide range of diseases, among which the most important are the so-called virilizing syndromes (polycystic ovary syndrome, Cushing's disease, adenoma and carcinoma of the adrenal cortex (Cushing's syndrome), as well as congenital hyperplasia of the adrenal cortex). It is important to note that differential diagnosis of these diseases cannot be carried out on the basis of clinical signs alone; it is based on a comprehensive determination of the level of steroid hormones and their precursors (12 compounds in total). This analysis allows for simultaneous assessment of all three groups of steroid hormones. Thus, corticosterone and deoxycorticosterone are precursors of aldosterone, and therefore measuring their concentration allows us to assess the characteristics of the synthesis of mineralocorticoids in the body. Determination of the level of 17-OH-progesterone (17-OPG), 21-deoxycortisol, cortisol and cortisone allows us to characterize the stages of glucocorticoid synthesis. Progesterone, androstenedione, dehydroepiandrosterone (DHEA) and testosterone are sex hormones.
A comprehensive analysis of steroid hormones is a mandatory component of the differential diagnosis of congenital adrenal hyperplasia - adrenogenital syndrome - a group of autosomal recessive enzymopathies accompanied by impaired synthesis of steroid hormones. Depending on the severity of the disease, adrenogenital syndrome can manifest itself in childhood, adolescence or adulthood. Its most common form (95% of cases) is caused by 21-hydroxylase deficiency, which impairs the synthesis of cortisol and aldosterone. A characteristic laboratory sign of 21-hydroxylase deficiency is a significant increase in the level of 17-OPG, DHEA, androstenedione and testosterone with a significant decrease in corticosterone, deoxycorticosterone and cortisol. It should be noted that only with the help of a comprehensive study of steroid hormones is it possible to differentiate 21-hydroxylase deficiency from another, more rare variant of adrenogenital syndrome - 11-beta-hydroxylase deficiency, since both enzymopathies have a similar clinical picture. Unlike 21-hydroxylase deficiency, 11-beta-hydroxylase deficiency is characterized by an excess of deoxycorticosterone. With the help of a comprehensive study of sex hormones, other forms of adrenogenital syndrome (17-alpha-hydroxylase, 3-beta-hydroxysteroid dehydrogenase deficiency) can be diagnosed.
In addition, a comprehensive study of steroid hormones can be used to assess the function of the hypothalamic-pituitary-adrenal axis when examining a patient with signs of adrenal insufficiency.
When interpreting the study results, some features of steroid metabolism should be taken into account. Most of the steroid hormones are in the blood in a bound state (bound to steroid-binding globulin, sulfated), that is, inactive. The proportion of active hormone depends on the physiological state of the body, the use of certain medications, and concomitant pathologies. Normally, only a third of the total amount of steroid hormones is present in a free state and is responsible for the effects manifested in target organs. The study allows you to determine the total amount of steroid hormones in the blood serum (the active and bound fractions of the hormone are not assessed separately). In addition, the effect of steroid hormones can be modified by their interaction with other hormonally active compounds at the level of binding to specific receptors, so the test result does not always correlate with the severity of the clinical manifestations of virilization syndrome. In other words, the study allows us to assess the concentration of steroid hormones, but not their bioactivity in the body.
What is the research used for?
- To diagnose diseases manifested by virilization syndrome;
- for differential diagnosis of clinical forms of adrenogenital syndrome;
- to assess the function of the hypothalamic-pituitary-adrenal system in a patient with signs of adrenal insufficiency.
When is the study scheduled?
- When examining a patient with symptoms of hyperandrogenism (hair growth above the upper lip, on the chin, the “white line” of the abdomen, severe acne, changes in voice timbre, clitoromegaly, increased muscle mass);
- when examining an infant with signs of impaired gender differentiation (external genitalia with characteristics of both female and male gender);
- when examining a patient with signs of adrenal insufficiency (weakness, fatigue, nausea, vomiting, loss of muscle mass and weight, appetite disturbances, hypotension, disturbances of consciousness).
What do the results mean?
Reference values
- Cortisone
| Age | Reference values |
| 1-7 days | 26-156 ng/ml |
| 7-14 days | 3-45 ng/ml |
| 2 weeks — 3 months | 9-54 ng/ml |
| 3 months - 1 year | 7-46 ng/ml |
| 1 year - 17 years | 6-30 ng/ml |
| Adults (morning) | 12-35 ng/ml |
| Adults (evening) | 6-28 ng/ml |
- Cortisol
| Age | Reference values |
| 1 month — 1 year (morning) | 46-230 ng/ml |
| 1 year - 6 years (morning) | 60-250 ng/ml |
| 6 – 18 years (morning) | 46-150 ng/ml |
| Adults (morning) | 46-206 ng/ml |
| Adults (evening) | 18-136 ng/ml |
- Corticosterone
| Age | Reference values |
| 1 – 17 years (morning) | 1.35-18.6 ng/ml |
| 1 – 17 years (evening) | 0.7-6.2 ng/ml |
| Over 17 years old (morning) | 1.3-8.2 ng/ml |
| Over 17 years old (evening) | 0.6-2.2 ng/ml |
- Deoxycorticosterone
| Age | Reference values |
| 1 month - 1 year | 0.07-0.49 ng/ml |
| 1-7 years | 0-0.37 ng/ml |
| 7-14 years | 0-0.34 ng/ml |
| More than 14 years | 0-0.19 ng/ml |
- 21-deoxycortisol
| Floor | Age | Reference values |
| Female | 7-10 years | 0-0.94 ng/ml |
| 10-13 years | 0-0.74 ng/ml | |
| 13-16 years old | 0-0.64 ng/ml | |
| 16-18 years old | 0-0.47 ng/ml | |
| Over 18 years old | 0-0.33 ng/ml | |
| Male | 7-10 years | 0-0.59 ng/ml |
| 10-13 years | 0-0.89 ng/ml | |
| 13-16 years old | 0-0.71 ng/ml | |
| 16-18 years old | 0-0.88 ng/ml | |
| Over 18 years old | 0-0.68 ng/ml |
- Progesterone, ng/ml
| Male | 1-17 years | 0.0-0.15 |
| Over 17 years | 0.0-0.11 | |
| Female | 1-11 years | 0.0-0.26 |
| 11-12 years old | 0.0-2.55 | |
| 12-13 years old | 0.0-8.56 | |
| 13-14 years old | 0.0-6.93 | |
| 14-15 years old | 0.0-12.04 | |
| 15-16 years old | 0.0-10.76 | |
| 16-17 years old | 0.0-12.94 | |
| More than 17 years, by cycle phases | Menstrual (1-6th day) | 0.0-0.17 |
| Folliculin (proliferative) (3-14th day) | 0.0-1.35 | |
| Ovulatory (day 13-15) | 0.0-15.63 | |
| Luteal (15th day - beginning of menstruation) | 0.0-25.55 | |
| Postmenopause | 0.0-0.1 | |
| 1-12th week Bertie | 6.25-45.46 | |
| 12-24th week. Bertie | 15.4-52.1 | |
| 24 or more weeks Bertie | 24.99-99.92 |
- 17-OH-progesterone
| Floor | Age | Reference values | |
| Female | 4 days – 1 month | 0.07-1.06 ng/ml | |
| 1 month – 1 year | 0.13-1.6 ng/ml | ||
| 1-7 years | 0.04-1.15 ng/ml | ||
| 7-10 years | 0-0.71 ng/ml | ||
| 10-13 years | 0-1.29 ng/ml | ||
| 13-16 years old | 0.09-2.08 ng/ml | ||
| 16-18 years old | 0-1.78 ng/ml | ||
| Over 18 years old | 0-2.07 ng/ml | ||
| Cycle phase | Folliculin (proliferative) | 0.15-0.7 ng/ml | |
| Luteal (day 15 – before the start of menstruation) | 0.35-2.9 ng/ml | ||
| Menstrual (1-6 days) | 0.15-0.7 ng/ml | ||
| Male | 4 days – 2 months | 0-2 ng/ml | |
| 2-12 months | 0.03-0.9 ng/ml | ||
| 1-7 years | 0.04-1.15 ng/ml | ||
| 7-10 years | 0-0.63 ng/ml | ||
| 10-13 years | 0-0.79 ng/ml | ||
| 13-16 years old | 0.09-1.4 ng/ml | ||
| 16-18 years old | 0.24-1.92 ng/ml | ||
| Over 18 years old | 0.15-0.7 ng/ml | ||
- Testosterone, ng/ml
| Female | Up to 30 days | 0.2-0.64 |
| 1-6 months | 0.0-0.2 | |
| 6 months - 2 years | 0.0-0.09 | |
| 2-4 years | 0.0-0.2 | |
| 4-6 years | 0.0-0.3 | |
| 6-8 years | 0.0-0.07 | |
| 8-10 years | 0.01-0.11 | |
| 10-12 years | 0.03-0.32 | |
| 12-14 years old | 0.06-0.5 | |
| 14-16 years old | 0.06-0.52 | |
| 16-18 years old | 0.09-0.58 | |
| 18-60 years | 0.09-0.55 | |
| Over 60 years | 0.05-0.32 | |
| Male | Up to 1 month | 0.75-4 |
| 1-6 months | 0.14-3.63 | |
| 6 months - 2 years | 0-0.37 | |
| 2-4 years | 0-0.15 | |
| 4-6 years | 0-0.19 | |
| 6-8 years | 0-0.13 | |
| 8-10 years | 0.02-0.08 | |
| 10-12 years | 0.02-1.65 | |
| 12-14 years old | 0.03-6.19 | |
| 14-16 years old | 0.31-7.33 | |
| 16-18 years old | 1.58-8.26 | |
| 18-40 years old | 3-10.80 | |
| 40-60 years | 3-8.9 | |
| Over 60 years | 3-7.2 |
- Dehydroepiandrosterone, ng/ml
| Female | Up to 2 days | 0-11 | |
| 2-7 days | 0-8.7 | ||
| 7 days - 1 month | 0-5.8 | ||
| 1-6 months | 0-2.9 | ||
| 6 months — 2 years | 0-1.99 | ||
| 2-4 years | 0-0.85 | ||
| 4-5 years | 0-1.03 | ||
| 6-8 years | 0-1.79 | ||
| 8-10 years | 0.14-2.35 | ||
| 10-12 years | 0.43-3.78 | ||
| 12-14 years old | 0.89-6.21 | ||
| 14-16 years old | 1.22-7.01 | ||
| 16-18 years old | 1.42-9.00 | ||
| 18-40 years old | 1.33-7.78 | ||
| More than 40 years | 0.63-4.70 | ||
| More than 40 years | Postmenopause | 0.6-5.73 | |
| By cycle phases | 18-40 years old | Menstrual (1-6th day) | 1.33-7.78 |
| Folliculin (proliferative) (3-14th day) | 1.33-7.78 | ||
| Ovulatory (day 13-15) | 1.33-7.78 | ||
| Luteal (15th day - beginning of menstruation) | 1.33-7.78 | ||
| Pregnancy | 1.33-7.78 | ||
| Premenopause | 1.33-7.78 | ||
| More than 40 years | Menstrual (1-6th day) | 0.63-4.70 | |
| Folliculin (proliferative) (3-14th day) | 0.63-4.70 | ||
| Ovulatory (day 13-15) | 0.63-4.70 | ||
| Luteal (15th day - beginning of menstruation) | 0.63-4.70 | ||
| Pregnancy | 0.63-4.70 | ||
| Premenopause | 0.63-4.70 | ||
| Male | Up to 2 days | 0-11 | |
| 2-7 days | 0-8.7 | ||
| 7 days - 1 month. | 0-5.8 | ||
| 1-6 months | 0-2.9 | ||
| 6 days - 2 years | 0-2.5 | ||
| 2-4 years | 0-0.63 | ||
| 4-6 years | 0-0.95 | ||
| 6-8 years | 0.06-1.93 | ||
| 8-10 years | 0.10-2.08 | ||
| 10-12 years | 0.32-3.08 | ||
| 12-14 years old | 0.57-4.10 | ||
| 14-16 years old | 0.93-6.04 | ||
| 16-18 years old | 1.17-6.52 | ||
| 18-40 years old | 1.33-7.78 | ||
| More than 40 years | 0.63-4.70 |
- Androstenedione
| Female | Up to 8 days | 0.2-2.9 |
| 8 days — 1 month | 0.18-0.8 | |
| 1-6 months | 0.06-0.68 | |
| 6 months - 2 years | 0-0.15 | |
| 2-4 years | 0-0.16 | |
| 4-6 years | 0.02-0.21 | |
| 6-8 years | 0.02-0.28 | |
| 8-10 years | 0.04-0.42 | |
| 10-12 years | 0.09-1.23 | |
| 12-14 years old | 0.24-1.73 | |
| 16-18 years old | 0.35-2.12 | |
| 18-40 years old | 0.26-2.14 | |
| More than 40 years | 0.13-0.82 | |
| Male | Up to 8 days | 0.2-2.9 |
| 8 days — 1 month | 0.18-0.8 | |
| 1-6 months | 0.06-0.68 | |
| 6 months - 2 years | 0.03-0.15 | |
| 2-4 years | 0-0.11 | |
| 4-6 years | 0.02-0.17 | |
| 6-8 years | 0.01-0.29 | |
| 8-10 years | 0.03-0.30 | |
| 10-12 years | 0.7-0.39 | |
| 12-14 years old | 0.1-0.64 | |
| 14-16 years old | 0.18-0.94 | |
| 16-18 years old | 0.3-1.13 | |
| 18-40 years old | 0.33-1.34 | |
| More than 40 years | 0.23-0.89 |
- 11-deoxycortisol
| Floor | Age | Reference values, ng /ml |
| Female | 1-6 months | 0,1 — 2 |
| 6 months - 1 year | 0,1 — 2,76 | |
| 1-4 years | 0,07 — 2,47 | |
| 4-7 years | 0,08 — 2,91 | |
| 7-10 years | 0 — 0,94 | |
| 10-13 years | 0 — 1,23 | |
| 13-16 years old | 0 — 1,07 | |
| 16-18 years old | 0 — 0,47 | |
| Over 18 years old | 0 — 0,55 | |
| Male | 1-6 months | 0,1 — 2 |
| 6 months - 1 year | 0,1 — 2,76 | |
| 1-4 years | 0,07 — 2,02 | |
| 4-7 years | 0,08 — 2,35 | |
| 7-10 years | 0 — 1,2 | |
| 10-13 years | 0 — 0,92 | |
| 13-16 years old | 0 — 0,95 | |
| 16-18 years old | 0 — 1,06 | |
| Over 18 years old | 0 — 0,59 |
- 17-OH-pregnenolone
| Floor | Age | Reference values, ng /ml |
| Female | 1-6 months | 2,29 — 31,04 |
| 6 months – 1 year 1 month. | 0 — 9,17 | |
| 1 year 1 month - 2 years | 0 — 5,92 | |
| 2-5 years | 0 — 2,8 | |
| 5-7 years | 0 — 3,5 | |
| 7-10 years | 0 — 2,12 | |
| 10-13 years | 0 — 3,98 | |
| 13-16 years old | 0 — 4,07 | |
| 16-18 years old | 0 — 4,23 | |
| Over 18 years old | 0 — 2,26 | |
| Male | 1-6 months | 2,29 — 31,04 |
| 6 months – 1 year 1 month. | 0 — 9,17 | |
| 1 year 1 month - 2 years | 0 — 5,92 | |
| 2-5 years | 0 — 2,49 | |
| 5-7 years | 0 — 3,19 | |
| 7-10 years | 0 — 1,87 | |
| 10-13 years | 0 — 3,98 | |
| 13-16 years old | 0,35 — 4,65 | |
| 16-18 years old | 0,32 — 4,78 | |
| Over 18 years old | 0 — 4,42 |
Characteristic laboratory parameters for the most common “virilizing syndromes”
- Polycystic ovary syndrome: increased concentrations of testosterone, dehydroepiandrosterone and androstenedione with normal values of glucocorticoids and mineralocorticoids.
- Cushing's syndrome: increased concentrations of cortisol and cortisone with normal values of mineralocorticoids and sex hormones.
- Congenital adrenal hyperplasia (21-hydroxylase deficiency): increased levels of 17-OH-progesterone, dehydroepiandrosterone, androstenedione and testosterone with a significant decrease in corticosterone, deoxycorticosterone and cortisol.
- Congenital adrenal hyperplasia (11-hydroxylase deficiency): increased levels of 17-OH-progesterone, dehydroepiandrosterone, androstenedione, testosterone and deoxycorticosterone with a significant decrease in corticosterone and cortisol.
Typical laboratory parameters for primary adrenal insufficiency:
- Decreased levels of corticosterone, deoxycorticosterone, 17-OH-progesterone, 21-deoxycortisol, cortisol and cortisone with normal concentrations of sex hormones.
What can influence the result?
- The result of the analysis may be influenced by the performance of diagnostic studies using radiocontrast agents within 7 days before the examination.
- The concentration of steroid hormones depends on the time of day - it reaches a maximum in the morning and decreases in the evening.
Where are hormone tests done?
Diana Medical Center offers its patients a full range of hormone tests. The drug and hardware base of our laboratory allows us to quickly and reliably determine the concentration of hormones in blood, urine and other biological fluids. In addition, the results are deciphered by our specialists, who, if necessary, will develop an optimal scheme for correcting hormonal levels.
Get tested for hormones
You can skip the line for adults, children, and pregnant women at a convenient time by making an appointment on any day - we work seven days a week. You can find out the cost of the listed studies on our website in the price list of services.
If you find an error, please select a piece of text and press Ctrl+Enter