Diseases of the nose and paranasal sinuses are a common reason for visiting an ENT doctor. According to statistics, every person suffers from rhinitis (runny nose) at least once a year. But there are many other diagnoses that are associated with the nasal cavity and cause discomfort to the patient. Nasal diseases can be congenital, traumatic or infectious. And each of them requires competent treatment, since many of them threaten the development of serious complications. Read about what diseases of the nose and paranasal sinuses there are in our new article.
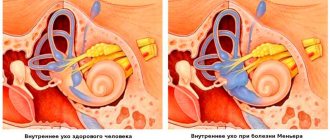
The nose is an important human organ. When we talk about the nose, we think of the visible part of it. However, the nasal cavity has a more complex structure. It is conventionally divided into two parts by the nasal septum. The nasal cavity consists of three nasal conchas, between which are the nasal passages. The entire nasal cavity is lined with mucous membrane.
Also in the front part of the skull there are special air cavities - paranasal sinuses (or otherwise - sinuses), which communicate with the nasal cavity through small openings - anastomoses.
Humans have four types of paranasal sinuses: maxillary (also known as maxillary), frontal, sphenoid, and ethmoidal labyrinth cells.
Like any other organ, the nasal cavity and sinuses are susceptible to disease.
What diagnoses are classified as diseases of the nose and sinuses, and what treatment will help in this or that case? In our new article we will look at the causes, symptoms and treatment of diseases of the nasal cavity and paranasal sinuses.
Causes
Sinusitis can be acute or chronic. In the case of an acute process, its main cause is a viral infection. Damage to the cells of the nasal mucosa by viruses leads to its swelling and cessation of normal air exchange in the nasal cavity and paranasal sinuses. There is a decrease in pressure in the sinuses below atmospheric pressure, which increases the formation of mucus. There is stagnation of the sinus contents, in which bacterial flora easily multiplies. As a result, purulent inflammation occurs.
Treatment of sinuses usually results in recovery. However, there are factors that contribute to the chronicity of the inflammatory process:
- anatomical changes - curvature of the nasal septum, hypertrophy of the nasal turbinates, which change the direction of air flow in the nasal cavity and complicate the aeration of the paranasal sinuses;
- diseases of the teeth of the upper jaw, which can cause infection to enter the maxillary sinus after tooth extraction, through blood vessels or even as a result of filling material entering the sinus;
- long-term diseases of the oral cavity and nasopharynx - rhinitis, tonsillitis, which are a constant source of pathogens.
Infections of the nose and paranasal sinuses: evolution from ARVI to acute bacterial sinusitis
00:00
Vladimir Trofimovich Ivashkin , academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences:
— Now we move on to issues of otoringology. Professor Valery Mikhailovich Svistushkin will report on infections of the nose and paranasal sinuses.
Valery Mikhailovich Svistushkin , professor:
— Good afternoon, dear colleagues and dear Vladimir Trofimovich.
We are talking today about a pressing issue in this transition period. Although the problem of acute respiratory diseases (ARI) is relevant throughout the year. At one time or another, certain viruses and bacterial agents are important and come out on top.
I would like to start with a seemingly rhetorical question: what is better to die from? The answer to this can be very different. One of the answers that may greatly satisfy us. From those reasons when we can leave this world as late as possible.
At 74, most Europeans reach their peak happiness. Their happy period begins at the age of 46. Sociological surveys of residents of European countries.
What do we have? Unfortunately, things are not so optimistic. We are behind in almost all respects. This is an otolaryngologist, so we are primarily talking about the upper respiratory tract. The difference between us and Western countries is palpable.
There really are problems. These problems are relevant for all countries. In particular, for Russia. I tried to formulate the problems of acute respiratory infections that have accumulated in our country this year.
High morbidity rate in general. We probably won’t talk about the famous H1N1 (swine flu) pandemic today. Fortunately, it is over (according to WHO experts). Although the virus, as you understand, has not gone away. According to many infectious disease specialists, it will circulate for a long time as a seasonal, epidemic virus.
Limitation of the possibility of virological diagnosis. In our practical activities, it is not so easy to assess which specific virus causes a particular disease. Difficulty in selecting etiotropic therapy. Increasing resistance to basic antiviral drugs. It should be emphasized that resistance is growing not only to antibiotics. It is also growing very actively towards antiviral drugs.
Emphasis on symptomatic therapy, self-medication. Insufficient use of pathogenetic therapy. Whatever inflammation we are talking about - viral or bacterial - this is inflammation. From this point of view, it is necessary to use pathogenetic treatment.
Another very serious problem is the use of drugs with unproven effectiveness. Polypharmacy, problems of prevention. We could talk and discuss each issue today for a very long time. The format of this program does not allow this, so I will allow myself to dwell on some of the most pressing issues, in my opinion.
03:21
If we are talking about specific viruses. Data may be different for different regions and cities. Data from St. Petersburg, where the largest percentage is accounted for by rhinoviruses. A large percentage of adenoviruses. Coronaviruses – sometimes more, sometimes less.
If we are talking about Moscow and the past epidemic season, then there may be adenoviruses, RS viruses, and parainfluenza virus. It doesn’t matter which viruses cause this or that disease (although this is also, of course, important), because we don’t have many etiotropic drugs for each of these viruses.
But in general I would like to emphasize the upper respiratory tract. The percentage of damage to the upper respiratory tract in any acute respiratory infection, in particular in viral pathology, is high. In any age category, it is the upper respiratory tract that primarily responds to the influence of a microbial agent.
This is especially true for runny nose and sinusitis. The data we recently received is very important. They show that in almost any acute respiratory infection, sinusitis has already occurred. It is almost always available.
Another thing is viral sinusitis. It's catarrhal, but it's already there. Where is the step before the development of bacterial inflammation. It can be very small. Then this is a purulent process. A special situation in treatment. Involvement of an otolaryngologist. During 80–90% of viral infections, these are patients who come to therapists, general practitioners, and family doctors. Including otolaryngologists.
05:18
How does it happen that the virus penetrates into the nasal cavity, the sinuses? You can trace this chain. The nasal cavity is the first barrier that the virus encounters. How this first barrier works will determine how much the systemic disease will develop and how pronounced the general processes will be. Or there will still be a more or less local situation in the form of acute rhino-sinusitis.
Reproduction of viruses, their replication, cytopathic effect, destruction of ciliary cells. Cells lose eyelashes. The mucous membrane becomes bald (as we say). A situation occurs that resembles a worn-out carpet. Eyelashes are eliminated.
Next are inflammatory mediators and cell death. The clinical picture in a detailed version. Everything will depend on how competently we carry out the treatment, how adequately the immune system works. Either this is recovery or transition to a chronic form.
Here I would like to return, probably, to the main mechanism of protection of this part of the respiratory tract. This is mucociliary transport (MCT). Famous eyelashes. The frequency of cilia beats (CBR) decreases by only 16%, and how much mucus transport decreases.
Our eyelashes were supposed to “start” today. But, unfortunately, we will not be able to see this beauty of the famous picture. Beating frequency 700 – 800 beats per minute. This is the norm.
A lot of factors influence the BBR.
(Slide show).
This is what the mucous membrane looks like during the development of a viral infection. The moment of baldness, loss of eyelashes. Hypersecretion. A large number of secretory cells.
This is quite a long process. The third day of the disease - the same bald mucous membrane. Only on day 7-8 eyelashes begin to form. The moment of completion of mucosal rehabilitation occurs at the end of the second week. At this moment, the mucous membrane becomes defenseless. Mucus accumulates here and its outflow is disrupted. Conditions arise for the development of attachment and bacterial flora. This step from catarrhal inflammation to the development of a purulent process begins here.
Although many factors influence sinusitis. Anatomical features (deformation of the nasal septum, enlarged nasal turbinates). Definitely an allergy. The influence of the allergic process on the development of sinusitis is 25 – 70%. Triggers in the form of smoking. We can talk and argue about this a lot. But there's no getting around it. The development of chronic rhinitis and factors that influence the development of sinusitis.
08:38
Very beautiful picture. It clearly shows how passive smoking affects our body. The death grip in the larynx has already worked at the level of the nasal cavity and paranasal sinuses. I think the slogan of the French Anti-Smoking League is very successful:
“Everyone can smoke as much as they want. Even if he dies from this, he should not disturb others with his smoke.”
Let's return to bacterial processes. The main source of bacterial infection is the microflora of the nasal passages. Next is one or another microorganism.
A study that evaluates how bacterial levels have changed recently tells us that betahemolytic streptococci are moving into second to third position. Haemophilus influenzae, M. Catarrhalis and streptococcus with pneumonia come out on top. This is not only our data, but also that of our Western colleagues. Streptococcus with pneumonia, M. Catarrhalis, hemophilus influenzae are the microorganisms that are leading in the development of the purulent process.
Everything is not so clear. Research in recent years, carried out in closed groups, has shown that Haemophilus influenzae has a fairly decent percentage and is ahead of streptococcus with pneumonia. If we talk about atypical flora, then any specialist involved in the lower respiratory tract will say that up to 30% of community-acquired pneumonia is the typical flora of mycoplasma pneumonia, chlamydophila, and so on.
Otolaryngologists may not evaluate this section of the bacterial flora in the same way. We understand perfectly well that we have a single breathing tube. If this problem exists in relation to the lower respiratory tract, then it is also relevant in relation to the upper sections.
10:39
How can we navigate when we talk about catarrhal viral inflammation, when about purulent. The diagram seems to me very simple and quite clear. If during the first five days of the development of acute rhinosinusitis we are talking about a viral infection. If there is a surge of symptoms, then the addition of bacterial flora takes place.
If this picture persists for 10 days, despite the treatment, the clinic does not change, then in this situation we can also talk about the development of a bacterial infection. Then we are talking about adding systemic antibacterial therapy.
If we talk about severity, then there are also quite clear visual analog scales that say that we can talk about a bacterial process if the symptoms are more than three points. The patient clearly indicates this interval from three to seven. This is still an outpatient situation.
If the symptoms become so severe that it can be assessed as more than seven points, this is a hospital. This is the parenteral route of administration of antibiotics and so on.
What should we do in this situation? WHO recommendations are clear. Whatever the etiological factor (virus or bacteria), we must carry out etiotropic treatment. For viruses, timely and rapid treatment with antiviral drugs helps to alleviate the entire situation.
A study that was carried out in Moscow. Professor Lyudmila Vasilyevna Kolobukhina showed how the percentage of complications of a viral infection increases if adequate timely antiviral treatment is not carried out.
With regard to acute rhinosinusitis, this is probably most relevant, because if treatment is timely, then in 40–45% of cases we do not end up using systemic antibiotics.
The range of antiviral drugs that we now use most often in our practice. Probably, each will have a problem or several problems in general. We could talk for a long time on this topic.
13:05
The most acute situation regarding the evidence base. Regarding resistance, they said that this problem is also very pressing. The most common drug that we can talk about a lot is Tamiflu. Resistance to it has increased greatly recently.
The evidence base is quite ambiguous. We do not have randomized trials for a number of drugs. Or the effectiveness of the drugs is not determined. We can now safely classify these drugs as drugs that cause a placebo effect.
The most common antiviral drugs and their effectiveness. Not everything is so clear. The most common in our practice are Ingavirin and Arbidol. These studies show that things are far from clear cut.
Another problem is the toxicity of antiviral drugs. Not in every case, when we prescribe this or that drug, we think about the fact that each of them has a toxic effect to a greater or lesser extent.
Principles of treatment of acute sinusitis. Etiotropic treatment is fundamental here. Many other points: from unloading therapy, elimination therapy. Since this is viscous mucus, a disruption of mucociliary clearance, it is necessary to use drugs that improve MCT. This is elimination therapy.
Our Western colleagues give us such a situation that antibiotics are taken internally. If we are talking about treating patients after 5 days, these are intranasal steroids (very popular nowadays).
Briefly about systemic antibiotics. The problems are the same. These are either beta-lactams in an acute situation, or macrolides, or fluoroquinolones. Here, too, everything is not so simple.
According to studies that were carried out in our country, resistance 10 years ago in relation to the group of macrolides. After 10 years, it has grown almost 2-5 times. This is food for thought. It allows us to think about which groups we should use first. Data regarding streptococci with pneumonia.
15:50
Data regarding Haemophilus influenzae. We must remember that Haemophilus influenzae is naturally resistant to the group of macrolides. Perhaps here we should reflect on how much this is the first line of defense. Resistance to Haemophilus influenzae is increasing in a number of modern pathogens.
If we evaluate the spectrum of antibacterial drugs, we are talking about beta-lactams, macrolides (neomacrolides) and fluoroquinolones. Errors do occur.
Data for Moscow. Errors regarding "Lincomycin" are a problem that we have been struggling with for many years. Fortunately, this has become less common. But this problem occurs. It is found in different cities. Or this is the parenteral route of drug administration in the treatment of moderately severe patients. Outpatient problem. This is a serious mistake when we talk about the parenteral route of administration.
Or this is local antibacterial therapy for patients when the prescription of systemic antibiotics is required. Almost all recommendations - domestic and our foreign colleagues - are similar in this regard. Beta-lactams, fluoroquinolones as a reserve drug or macrolides.
Initial therapy and meta-analysis of a very large number of studies show that the first drug (when we talk about the treatment of patients with acute purulent sinusitis) is the penicillin series. More specifically, amino-protected penicillins. Research shows that they are superior to the non-combination form of beta-lactams.
Another point that must be fundamentally remembered is that for infections associated with Haemophilus influenzae, the microbiological effectiveness of amino-protected penicillins is superior to the group of macrolides. As we remember from the famous film, amino-protected ones are far from identical in their bioavailability. The line of flexmoxins is significantly superior to other amino-protected forms.
18:11
Macrolides are naturally resistant to Haemophilus influenzae. If we are talking about atypical flora, then this is probably the first line of defense. For respiratory quinolones this is a reserve. It has its undoubted advantages. Very wide range of activities. Of course, it has its disadvantages in the form of side effects. We know them very well.
Resilience is growing. This can be seen using an example. The more often we use certain groups of antibiotics, specific drugs, the more resistance to them will increase.
There are many ways to overcome this resistance. Creating new antibiotics is probably not the way to go, because it requires a huge amount of material investment and time.
The development of inhibitors similar to the introduction of clavulanic acid provides us with some help. Increasing the single daily dose – this situation exists among our Western colleagues. For example, among American colleagues the daily dose increases to 3-4 grams per day. But for now we have recommendations of up to 2 grams. We do not have the same resistance problem that exists in those countries.
Development of new delivery forms. In this regard, the line of solutes is very indicative. Such new technologies make it possible to maximize the absorption of the drug and reduce side effects. Thus, the maximum amount of the drug ends up in the blood and tissues. This bacteriocidal or bacteriostatic effect also manifests itself.
Studies that have been conducted in our country and abroad show how effective new forms of antibiotics are. This is also associated with a reduction in undesirable phenomena, side effects that arise primarily from the gastrointestinal tract. These studies, in my opinion, are very eloquent.
In conclusion, I would like to say that for our country the method of drainage and establishment of puncture outflow is very relevant. Almost always a puncture is performed. Here you can argue with your Western colleagues: whether it is necessary or not. One of the good drainage methods.
But we also have modern methods. For example, balloon-catheter sinusotomy. Under the control of endoscopes, a special balloon is inserted into the paranasal sinus, and the natural opening is expanded. This opening, through which the sinus drains, remains dilated. Then you can rinse your sinus.
A method that has already been registered in Russia since the fall of this year. We are actively starting to use it. We have very high hopes for such a minimally invasive, almost surgical method of treatment.
21:20
We probably won’t show the film today. This is information for our new meetings.
In conclusion, I would like to say that indeed the problem of acute respiratory infections will always be relevant. Including the problem of treating acute rhinosinusitis. This is a comprehensive approach. Use of innovative forms and medications. Of course, new surgical technologies.
Thanks a lot.
Vladimir Ivashkin : Thank you very much, Valery Mikhailovich. You have a lot of questions. You will cope with them if you answer very briefly, otherwise it will be a second lecture.
Valery Svistushkin : I will try to be very short. Question from Saratov.
Question: Does resistance to Josamycin vary across geographic regions?
Yes, such data exists. In general, such resistance is not expressed, so one of the options for using this drug is in the treatment of patients with acute tonsillitis. This is another problem that should apparently be considered separately.
Question: Is tonsillectomy still relevant today?
It is always relevant. It was and remains. During the testimony, we carried it out the same way we carry it out. There are modern, new technological methods of treating patients with chronic tonsillitis, but no one has canceled tonsillectomy.
22:38
Question: Is it necessary to immediately prescribe antibiotics to patients with ARVI who have chronic tonsillitis in order to avoid the development of complications?
All studies that have been conducted here and abroad show that preventive administration of systemic antibiotics does not reduce the risk of developing bacterial tonsillitis. We begin to prescribe antiviral drugs in the same way as in the case of viral sinusitis. Next we assess the situation.
Question: Do you recommend the use of macrolides in pediatric practice, especially for diphtheria?
No one has canceled the macrolide group of antibiotics. But in each specific case it is necessary to assess which pathogen causes a particular disease. We talk about this a lot and will continue to talk about it. In a number of cases, macrolides are the first line of defense.
Question: How to treat bacterial sinusitis in children under two years of age?
I hope that in my conversation I answered this question.
Question: Evidence base for the effectiveness of Arbidol and Oscillococcinum.
She exists. In particular, with regard to Oscillococcinum, there are also double placebo-controlled randomized studies. With regard to Arbidol, everything is not so clear, although there have been such studies.
Question: How do intranasal administrations of lactobacilli affect the creation of nasopharyngeal microflora and subsequent morbidity?
In no case can this replace the main methods of treatment, including etiotropic therapy.
Question: Is there any point in the prophylactic use of Oxolinic ointment for acute respiratory infections?
None. Absolutely. We already said today that this is the placebo effect.
Question: When should you start prescribing antibacterial drugs for acute respiratory infections?
I tried to answer this question. In particular, with acute rhinosinusitis, the watershed is 5-6 days, and then clinical symptoms must be assessed.
Symptoms
Inflammation of the paranasal sinuses is accompanied by the following clinical manifestations:
- difficulty breathing through the nose, nasal congestion;
- headache and/or pain in the inflamed sinus area (forehead, bridge of the nose, upper jaw);
- moderate mucous or mucopurulent nasal discharge;
- drainage of mucus down the back of the throat (postnasal drip), which may be accompanied by a cough;
- fever, weakness, and sweating are possible in acute sinusitis caused by microbial flora.
Symptoms and treatment of diseases of the nose and paranasal sinuses
Let's start with rhinitis. People call it a runny nose. By the way, 90% of the planet's inhabitants still suffer from this disease. A runny nose is an inflammation of the nasal mucosa. There are many reasons for its development - allergies, microbes, viruses, adenoids. Without treatment, rhinitis quickly becomes chronic. Its main symptoms are sneezing, watery eyes, and nasal discharge. Chronic nasal congestion leads to swelling of the mucous membrane and decreased sense of smell. Rhinitis is treated conservatively: with vasoconstrictor drops, inhalations and rinses.
Sinusitis has several types and three forms: acute, subacute and chronic. Develop due to infections and allergies. The main symptoms include headache, fever and nasal congestion. Additionally, they are accompanied by a feeling of pressure on the eyes, lack of smell, radiating pain and neuralgia. Treatment of sinusitis directly depends on its symptoms and type. The disease develops quite quickly, but is treated more slowly. The danger lies in the fact that pus from the sinuses and nasal cavity can move into the tissues adjacent to the brain, which threatens the development of an abscess. If we talk about surgical intervention, today there are minimally invasive and non-invasive methods for clearing the nasal passages of exudate.
Chronic inflammation can lead to the formation of polyps
– benign neoplasms on the mucous membrane. As polyps grow, they block the nasal passages, making breathing difficult. Polyposis is characterized by frequent diseases of the nasopharynx, since the tumor pinches the vessels, thereby preventing the mucous membrane from performing its protective functions. These are accompanied by a nasal voice, hearing and smell impairment. In the early stages, you can try to treat the disease conservatively, but in most cases surgery is more effective. Interestingly, women suffer from this disease four times more often than men.
If previous diseases have a rather short period of development from one condition to another, then scleroma
develops over the years. The main cause of the disease is infection. Initially, nodules form in the mucous membrane, which scar over time. The new, dense tissue narrows the nasal passages and makes breathing difficult. Scleroma is characterized by nasal congestion, hoarse voice, drowsiness, weakness, and frequent headaches. The pathology is treated with medications and physiotherapy. Surgery can only be prescribed if the disease has become severe.
Kinds
Sinusitis is classified according to different criteria. For example, the duration distinguishes between acute form (less than 3 months) and chronic form (more than 3 months). If the disease in its acute form recurs several times a year, it is referred to as recurrent sinusitis.
Chronic inflammation of the sinuses has varying degrees of morphological changes and can be catarrhal, purulent, polyposis, allergic, necrotic; There are other, rarer options.
Exacerbation of chronic sinusitis refers to the addition of new symptoms and/or increased severity of existing ones.
There are mild, moderate and severe sinusitis. Depending on the affected sinus, sinusitis, frontal sinusitis, ethmoiditis, sphenoiditis or their combinations occur.
Depending on the causative agent of the pathology, the following types of sinusitis are distinguished:
- viral, caused by adeno, rhino-, coronaviruses, influenza virus, parainfluenza, respiratory syncytial and other causes of ARVI;
- bacterial, most often caused by pneumococcus, moraxella or Haemophilus influenzae; Among this group, sinusitis is distinguished against the background of immunodeficiency, nosocomial (developed during a hospital stay), odontogenic (associated with dental diseases);
- fungal, more often occurring during long-term irrational treatment with antibiotics or when affected by highly pathogenic species of fungus, including systemic mycoses.
Treatment of inflammation of the sinuses is carried out taking into account the duration, severity of the disease and its causative agent.
Deviated nasal septum: how it is treated
A deviated nasal septum is a fairly common pathology. The cause is a physiological feature or injury. The severity of the symptoms of the disease is determined by how much the septum is curved. A minor curvature may have no symptoms and require no treatment. With a significant curvature of the septum, the following may be observed:
- Difficulty in nasal breathing
- Snore
- Dry nose
- Headache
- Discharge (including bleeding) from the nose
- Frequent inflammation of the paranasal sinuses
- Polyps
Typically, in the clinic, when a deviated septum is accompanied by severe symptoms, surgical intervention is prescribed. The operation is performed by clinic specialists using different methods:
- Septoplasty. Endoscopic modern minimally invasive surgery.
- Laser treatment. This operation is possible only if only the cartilaginous part of the septum is bent.
Since this disease can cause inflammation of the nasal cavity, paranasal sinuses, nasopharynx or ear, you should not delay the treatment of a deviated septum.
Diagnostics
To carry out full treatment of sinuses, you need to contact an ENT doctor to diagnose the disease. The doctor evaluates the patient’s complaints, takes into account risk factors (hypothermia, dental disease, concomitant ENT pathology), and conducts an examination of the nasal cavity. Then additional diagnostic tests are prescribed:
- video endoscopy of the nasal cavity to examine its walls and sinus outlets;
- X-ray to detect fluid or swelling in the maxillary or frontal sinuses;
- computed tomography of the paranasal sinuses is the most accurate diagnostic test, providing information about the condition of all paranasal sinuses;
- Ultrasound can be used as a screening test to quickly determine the affected sinus.
If treatment of inflammation of the sinuses is ineffective, a microbiological examination of the contents, which can be obtained by puncture, is necessary.
Why is it better not to treat yourself?
Even ordinary acute rhinitis, if not treated correctly, can become chronic or cause inflammation of the paranasal sinuses. Therefore, for the treatment of a runny nose, it is better to use remedies prescribed by a specialist.
For more serious diseases, diagnosing the pathology and adequate treatment are even more necessary measures. It is better not to treat sinusitis or rhinitis, as well as other nasal diseases, on your own, since even if the symptoms decrease, the inflammatory processes will only progress, posing a threat to your health.
Treatment
Therapeutic measures for sinusitis are aimed at fighting infection, interrupting the pathological mechanisms of the disease and relieving symptoms. It is performed on an outpatient basis. The patient is hospitalized in the following situations:
- severe infectious process with fever, intoxication, especially in children and the elderly;
- the appearance of severe headache, blurred vision or neurological symptoms;
- spread of pain to the orbital area;
- long-term use of immunosuppressants or glucocorticoids, as well as other immunodeficiencies.
Treatment at home
Home remedies can help relieve the pain and fullness of acute sinusitis. They improve sinus drainage and increase the effectiveness of other treatments. Basic recommendations:
- drink more warm liquids to keep the nasal mucosa hydrated;
- breathe warm, moist air, use humidifiers, do not go out into the cold;
- rinse your nose with a solution of table or sea salt, and also gargle with it;
- if necessary, blow your nose, do it carefully, without closing any of the nostrils;
- do not drink alcohol, which causes swelling of the nasal mucosa.
Drug therapy
The mainstay of treatment for sinus inflammation is antibiotics. Amoxicillin, amoxicillin clavulanate, cephalosporins, macrolides, and fluoroquinolones are used. For fungal infections, amphotericin B and fluconazole are used.
Additional medications for sinusitis:
- decongestants in the form of nasal drops or sprays for no more than 5 days; these drugs constrict blood vessels, relieve swelling of the mucous membrane and create conditions for the outflow of pathological sinus contents;
- antihistamines are indicated for bacterial sinusitis with signs of an allergic reaction; they dry out the mucous membrane and relieve swelling;
- painkillers, such as NSAIDs;
- local use of antiseptics (rinsing the nose with furatsilin solution), irrigation therapy (Miramistin, Aqualor, Dolphin, products based on sea water or saline with the addition of iodine);
- for chronic sinusitis (except for the odontogenic variant), a course of use of glucocorticoid-based sprays that suppress inflammation is acceptable; a doctor must prescribe them.
Traditional medicine
Such recipes help improve nasal breathing, relieve inflammation and swelling, and strengthen local immunity. They should only be used in combination with drug therapy after consultation with a doctor. The following tools may help:
- inhalation based on crushed garlic mixed with apple cider vinegar;
- insertion into the nose of tampons soaked in a mixture of onion juice, honey and sunflower oil;
- instillation of aloe juice, radish, onion, a mixture of beet juice and honey, propolis into the nose;
- compresses on the affected sinus area with a decoction of calendula, plantain, and chamomile.
Operation
Such surgical intervention as puncture of the affected sinus with removal of pus and rinsing the cavity with antiseptics is now rarely performed. It is believed that this is an invasive intervention, which is often accompanied by complications (damage to the orbit, upper jaw, air embolism, and others). It is usually indicated for patients with severe acute sinusitis
For the treatment of chronic sinusitis, other surgical techniques are used, both traditional with open intervention on the sinuses, and minimally invasive using endoscopic techniques:
- interventions aimed at eliminating anatomical deformations - septoplasty, removal of adenoids and others;
- intranasal antrostomy - creating an opening in the wall of the maxillary sinus into the nasal cavity;
- radical antrostomy - creation of a permanent drainage hole with removal of part of the bony wall of the sinus.
Prevention
To prevent the development of sinusitis, the following preventive measures are recommended:
- timely treatment of rhinitis and other conditions accompanied by nasal congestion;
- prevention of acute respiratory viral infections, avoidance of contact with sick people, frequent hand washing during the cold season;
- quitting smoking, including passive smoking;
- for allergic sinusitis – treatment of allergies, courses of allergen-specific immunotherapy;
- using humidifiers at home and at work;
- vaccination against influenza and pneumococcus;
- restorative measures, healthy lifestyle, proper nutrition.
NIKIO Medical Center invites all patients with acute or chronic sinusitis for consultation and treatment. The most experienced doctors work here, using modern diagnostic and treatment techniques. Timely contact with specialists greatly increases the likelihood of a cure for sinusitis, including its chronic forms.