Breast cancer is the most common cancer among women in Russia. The tumor occurs in 11% of women during their lifetime, while the incidence continues to grow, increasing annually by 1.2%. About 1 in 2,000 women who are pregnant or breastfeeding will also develop breast cancer. Breast cancer also occurs in men, but it is quite rare - less than 1 in every 180 cases.
This form of cancer ranks third among all causes of death among the female population of Russia after diseases of the circulatory system and accidents in all age groups.
Regular examination by a mammologist will help identify breast diseases in the early stages, provide timely assistance and maintain health.
- Breast tumors on ultrasound can be presented as a delimited formation or an area with a violation of the normal echostructure.
- Whether a breast space-occupying lesion belongs to a malignant or benign process is determined based on the following echo signs:
- • the nature of the contours (smooth, uneven, clear, fuzzy, wavy, scalloped, star-shaped).
- • relationship with surrounding tissues;
- • type of internal structure;
- • echogenicity;
- • acoustic effects observed behind the tumor;
- • nature of blood supply.
The nature of the tumor contours is one of the main differential criteria for the type of tumor growth in the breast—expanding or infiltrating.
A benign tumor does not destroy surrounding tissues, but only pushes them apart. Therefore, benign tumors are characterized by clear contours and a delimited (expanding) type of growth.
Malignant breast tumors are mostly represented by cancers. Breast cancer has a heterogeneous pathohistological structure. Most breast cancer (up to 70-80%) are invasive, ductal.
Invasive forms of breast cancer are characterized by an infiltrating type of growth, which is manifested echographically by blurring and unclear contours. With the infiltrating type of tumor growth, it can be difficult to draw a boundary between the edge of the tumor and the surrounding tissues.
Echographic signs of infiltrating growth type are never found in benign tumors. At the same time, ultrasound signs of a limited type of growth can be detected in both benign and malignant tumors.
Both benign and malignant tumors may have their own anatomical capsule, or a pseudocapsule formed by compressed or fibrotic surrounding tissues.
The echogenicity of a tumor may vary, but malignant tumors are more characterized by low echogenicity and heterogeneity of the internal structure.
Acoustic effects in breast tumors are varied: from a slight increase or decrease in ultrasound waves to the appearance of acoustic shadows behind the formation. Acoustic shadow is considered one of the leading ultrasound signs of malignancy. However, statistical data indicate that this echographic sign is detected only behind 30-65% of malignant tumors. It should be noted that in breast cancer, the frequency of occurrence of the dorsal acoustic shadow (ultrasound mammography criterion) approximately corresponds to the frequency of grouped microcalcifications (X-ray mammography criterion).
Characteristics of benign and malignant tumors
There are clear criteria:
- Delineation of the tumor from adjacent tissues.
- Growth rate.
- Ability to metastasize.
- Histological portrait of cells.
- Patient survival.
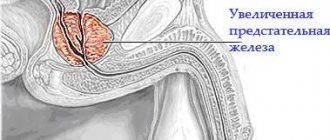
Benign tumors are clearly demarcated from healthy tissue and often have a capsule. Cancer grows into surrounding tissues, penetrates into blood vessels, and its contours are more amorphous.
Most benign tumors can grow for years without showing symptoms. Carcinomas grow quickly, disrupting organ functions and poisoning the body. Growth is accompanied by fatigue, weakness, weight loss, and pain.
Benign formations “sit” in one place, gradually grow and push apart healthy tissues, and are mobile when palpated. Cancer cells are loosely attached to each other, are easily separated and spread by lymph and blood throughout the body. They settle in the lymph nodes, bones, and internal organs, forming new tumor foci - metastases. On palpation, the node is fused to the tissues and does not move.
A biopsy provides a lot of information. The study shows that benign cells are similar to healthy ones, their structure is clearer. The structure of malignant cells is greatly altered due to pronounced mutations. The less the cells resemble the tissue from which they grew, the worse the prognosis for treatment and life.
A benign tumor, such as prostate adenoma, can be removed and a complete cure can be achieved. If a relapse occurs, it will be in the same place where the primary lesion was found. Malignant tumors are difficult to remove completely. Even one remaining cell will give rise to a new tumor either in the old place or where it got through the vessels. The survival rate of patients is significantly lower.
3.Cancer diagnosis
The earlier cancer is diagnosed, the higher the chances of successful treatment. Some types of cancer, such as skin cancer, breast cancer, oral cancer, testicular cancer, prostate cancer and colorectal cancer, can be detected independently, through self-examination, or simply by carefully observing sensations in the body. In general, before symptoms become very severe.
Most types of cancer, unfortunately, are diagnosed only when the symptoms of cancer become too severe and the tumor is obvious. Sometimes cancer is diagnosed accidentally, during an examination related to the detection of other diseases or their treatment.
Diagnosis of cancer begins with a thorough medical examination by an oncologist. Laboratory tests of blood, urine, and stool may reveal abnormalities that raise suspicion of cancer. If a tumor is suspected, X-rays, computed tomography, magnetic resonance imaging (MRI), ultrasound and endoscopic examination may be performed. All these methods of diagnosing cancer will allow the doctor to determine the presence of a tumor, its size and location, as well as the presence of metastases. To confirm the diagnosis of cancer, a biopsy is performed - taking a tissue sample from the suspected tumor and examining it for the presence of cancer cells.
After a cancer diagnosis, an individual cancer treatment program is developed. Treatment for cancer may include chemotherapy, radiation and surgery and be accompanied by immunotherapy.
About our clinic Chistye Prudy metro station Medintercom page!
Types of tumors
Benign:
- cysts;
- nevi or moles;
- nodules whose name has the oma suffix: fibroma, myoma, adenoma, papilloma - depending on the specific tissue.
Malignant:
- formations whose name is appended with the word carcinoma, sarcoma, blastoma, blastosis (fibroblastoma, myosarcoma, adenocarcinoma);
- oncological diseases of the blood - lymphogranulomatosis, leukemia and others;
- skin cancer - melanoma, basal cell carcinoma.
The differences are not always obvious. A thorough diagnosis is needed to look for atypical cells.
Features of cystic-solid formations
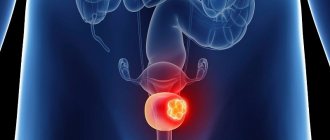
- Solid formation (cancer) is the most dangerous condition in which the chances of recovery from the disease are minimal; it has a hard shell and is filled with tissue.
- In contrast, a cystic neoplasm is easy to treat, is soft, and can grow and shrink.
- Cystic-solid formation is an intermediate link between them. It can appear in any organ, change in size or remain unchanged, and also contain both tissue and liquid substance.
Author's technique for removing a retroperitoneal tumor
The critical stages of the operation are isolation of the tumor, establishment of its connection with surrounding organs and vital structures, revision and mobilization of the tumor. I always give preference to the laparoscopic approach, which is less traumatic and effective.
A special feature of my laparoscopy technique is the method I developed for installing trocars, which allows me to place surgical instruments at an optimal manipulation angle. Excision of pathological formations in this complex area is thus quick and safe.
During surgery, I also use modern ultrasonic scissors and a device for dosed electrothermal tissue ligation “LigaSure” (USA), which eliminates the need to use surgical threads and clips. The absence of bleeding in the surgical area ensures the safety of the intervention and maximum precision when manipulating the smallest structures. In the case of a primary retroperitoneal tumor and the presence of damage to adjacent structures, radical surgery is performed as a single block. The removed tissues are sent for histological examination, which is important for further treatment and prognosis.
I have been performing laparoscopic interventions since 1997; I have performed more than 200 operations to remove retroperitoneal tumors using laparoscopic access. Any patient who contacts me can count on my knowledge and experience. Based on the examination results, I select treatment tactics in such a way as to achieve the most effective result.
Causes
At the moment, the causes of the development of retroperitoneal tumors have not been fully established. However, there are a number of factors contributing to their appearance:
- genetic abnormalities;
- exposure to harmful radiation or chemicals (such as herbicides or pesticides);
- suppression of the immune system due to the toxic effects of chemicals.
There is a version that the disease develops in patients who have undergone radiation during treatment for cancer.
To determine the type of retroperitoneal cyst, its localization to the main structures of the organ and indications for surgery, as well as choosing the correct surgical treatment tactics, you must send me a complete description of the ultrasound of the abdominal cavity, MSCT data of the retroperitoneal space with contrast, indicate your age and main complaints to your personal email address . Then I will be able to give a more accurate answer to your situation.
Anaplastic thyroid cancer - symptoms
The symptoms of anaplastic cancer are very specific, and both the patient himself and a doctor of almost any specialty can suspect it. The most important symptom is the appearance of a rapidly growing tumor on the front of the neck. The growth of the tumor occurs so quickly that it is noticeable to the eye - in the morning the tumor looks larger than in the evening. Typically, anaplastic thyroid cancer is firm to the touch. The tumor quickly loses mobility due to growth into surrounding organs. Damage to the recurrent nerves by the tumor leads to loss of mobility of the vocal folds and, as a result, to deterioration of the voice (hoarseness, hoarseness, weakness of the voice). When a tumor grows into the trachea, suffocation occurs. Often, upon palpation, compacted enlarged lymph nodes on the lateral surfaces of the neck are revealed. Tumor growth into the esophagus leads to difficulty swallowing food and water.
The patient's general condition worsens - fever, weakness, and fatigue may appear. A blood test often reveals leukocytosis (increased levels of white blood cells). It should be noted that anaplastic thyroid cancer itself does not produce hormones, so the levels of TSH, T4 free, T3 free, and blood calcitonin will be within normal limits.
Treatment of solid cancer
Solid education is cancer, an extremely serious illness that requires a thorough approach and the highest level of qualifications. Only truly experienced specialists are able to make an accurate diagnosis and select the most appropriate treatment, which depends on the location, size and other characteristics of a particular tumor.
Oncology specialists are doctors who have been involved in identifying and treating cancer at various stages for many years. If you have any doubts about your health, sign up for a consultation. Remember that at the initial stage, overcoming the disease is easier, faster and painless.
Gastrointestinal stromal tumors (GIST), identified as an independent nosological unit, are no longer a rarity for oncologists. GISTs are gastrointestinal (GI) stromal tumors that share a common progenitor cell origin with interstitial cells of Cajal. The latter are located between the circular and longitudinal muscle fibers of the wall of the gastrointestinal tract and are pacemakers that regulate autonomous peristaltic activity. GISTs are the most common neoplasms in the group of mesenchymal tumors of the gastrointestinal tract.
GISTs can affect any part of the gastrointestinal tract, but are most often localized in the stomach (40-60%) and small intestine (30-35%). Less commonly, the colon and rectum are affected (5-16%), and the esophagus is extremely rare. There are primary GISTs localized outside the hollow organs, for example, in the omentum or retroperitoneum. GIST is most often diagnosed in middle-aged and elderly people. The peak incidence occurs in the 5th and 7th decades. The gender distribution is equal, with a slight predominance of men.
The algorithm for examining patients with suspected GIST includes endoscopic and radiological diagnostic methods. The main confirmation of the diagnosis is an immunohistochemical study with the determination of specific markers.
Until recently, the only treatment for GIST was surgery. However, even the operation of complete cytoreduction did not allow achieving a 5-year survival rate above 50-65%. Systemic chemotherapy has been tried as an adjuvant treatment, especially in patients with a disseminated process or in whom the integrity of the formation was disrupted during surgery. But no real improvement in patient survival was noted. Radiation therapy was used even less frequently due to low effectiveness, the possibility of radiation damage to the intestine, and limited use only in patients with GIST of the stomach and rectum. The median survival of patients with disseminated process was 10 months.
The situation has changed dramatically since 2001, when a group of Finnish oncologists led by Heikki Joensuu [1] reported the first experience of using a tyrosine kinase receptor inhibitor in a patient with GIST. They used the drug STI 571, which is now known as Gleevec (imatinib). The ineffectiveness of traditional chemotherapy regimens and the significant antitumor activity of imatinib served as the reason for the fastest registration of the drug in modern history.
From this moment on, a new era began in the treatment of patients with GIST. However, despite the obvious improvement in statistical indicators, unresolved issues are not decreasing.
Thus, the diagnosis and treatment of patients with GIST is an urgent problem in modern oncology.
Diagnosis of GIST
Esophagogastroduodenoscopy in most cases allows us to assume that the patient has a stromal tumor and, importantly, to perform a biopsy of the formation. The endoscopic picture is quite diverse, the size of non-epithelial formations varies from 1-2 cm to 20-30 cm. With a small tumor size and endoscopic ultrasound (US), it can be determined that the tumor comes from the muscle layer [2]. However, sometimes difficulties arise in the endoscopic diagnosis of GIST, which are associated with the characteristics of tumor growth. With a small size of the tumor node, the endoscopic picture may correspond, depending on the nature of growth, to an unchanged organ (with an extraorgan form), compression from the outside (with a mixed form) or a submucosal formation - with an endorgan form. With the first two forms, it is rarely possible to accurately assess the true size of the tumor node, even using endosonography. The mucous membrane in the initial stages of the disease is usually not changed, which makes forceps biopsy very difficult. Even the use of in-depth stepwise biopsy does not always provide material suitable for histological examination [3, 4].
In such a situation, a simple and very effective method is transabdominal ultrasound with targeted tumor biopsy. The echographic picture of GIST typically consists of single or multiple nodular formations associated with the wall of the stomach or intestine. In our observations, the extraorgan form of GIST growth was mainly noted. The contour of formations at the initial stage of the disease with a node size of up to 4 cm is smooth and clear. At later stages, in places where the tumor grows into adjacent organs and the peritoneum, the contour becomes uneven and unclear, which is an echographic sign of invasive growth. The structure of the tumor nodes is solid, of medium echogenicity, with a pronounced vascular network. Characteristic of GIST is the presence in the structure of the tumor of liquid inclusions with a smooth wall, with homogeneous anechoic content. The cavities can be different, from single small ones to multi-centimeter ones, occupying up to 90% of the tumor volume.
To perform a puncture biopsy, it is optimal to use a biopsy gun, which is equipped with disposable removable needles. The most suitable size are needles with a length of 20 cm and a caliber of 16-18G. When the biopsy device is triggered, there is a sequential release of the inner and then the outer part of the needle with a short (less than 0.1 s) interval. In this case, a fragment of tissue in the form of a “column”, about 2 cm long and 1-1.5 mm thick, is retained in the needle groove. This amount of material is usually sufficient for histological and immunohistochemical studies. The puncture biopsy technique is carried out as follows. After antiseptic treatment of the skin along the intended puncture route with an anesthetic solution, layer-by-layer infiltration anesthesia is performed. A sharp-pointed scalpel is used to make an incision in the skin. Then, under constant on-screen control, the biopsy needle is brought to the border of the tumor formation and the biopsy gun mechanism is activated (see figure).
Figure 1. Echograms. Percutaneous biopsy of gastric GIST (arrows indicate biopsy needle). Applying the biopsy needle (a); collection of material (b).
Thus, transabdominal ultrasound, taking into account ultrasound semiotics, allows us to predict GIST in the patient being examined, as well as to accurately assess the local extent of the process. Targeted puncture of a nodular formation in the wall of a hollow organ, subject to the described conditions, is safe and allows one to obtain material for histological confirmation of the diagnosis at the preoperative stage of treatment.
Particular attention in the GIST diagnostic algorithm is paid to computed tomography (CT), which is used as a clarifying diagnosis, as it gives a clearer idea of the size, nature of tumor growth, invasion of neighboring organs and structures, as well as the presence of metastases. Equally important is the use of CT when conducting follow-up examinations of patients after and during treatment. On a computed tomogram, GISTs appear as single or multiple volumetric formations with a heterogeneous internal structure and clear contours. Areas of low density in the central regions of tumors may be due to intratumoral necrosis, hemorrhage, or cystic degeneration. With intravenous contrast, a pronounced uneven “enhancement” of tumor masses is observed in the early phases of the study. Unlike adenocarcinomas, gastrointestinal stomal tumors do not exhibit concentric narrowing of the lumen of the affected intestine. Invasion of the great vessels and venous thrombosis, as a rule, are not observed. Despite the fact that the primary tumor is hypervascular, most intrahepatic metastases appear as low-density foci with signs of weak enhancement of their peripheral parts in the arterial phase. However, both hypo- and hypervascular lesions can occur in the same patient. In the largest metastases, there may be areas of necrosis, sometimes areas of hemorrhage and calcifications (the latter, as a rule, after chemotherapy treatment) [5].
Since 1983, when M. Mazur and H. Clark [6] first identified a special subgroup of gastrointestinal nonepithelial tumors, differing in their immunohistochemical and ultrastructural characteristics from tumors with true neurogenic and smooth muscle differentiation and called them GIST, the mechanism of occurrence of these tumors has long been remained unclear. The discovery of S. Hirota et al. in 1998 [8] of the molecular mechanisms responsible for the appearance of GIST, made it possible to make a significant breakthrough in understanding the pathogenesis of this disease. It was found that this type of sarcoma is characterized by abnormal activation and overexpression of the KIT gene (4q12), the protein product of which c-Kit (CD117, KIT) belongs to type III of the plasma transmembrane receptor tyrosine kinase family. Mutations in the KIT gene occur in gastrointestinal tumors in 56–92% of patients [9]. As a rule, they are localized in the 9, 11, 13, 14 and 17th exons of the gene.
In 3-8% of cases, a mutation is detected in the PDGFRA gene (exons 12, 14 and 18), encoding the platelet factor α receptor. It is extremely rare that mutations are localized in the BRAF gene (less than 1%). In approximately 12-15% of GISTs, mutations in the above genes cannot be detected. In this case, they speak of a wild type mutation [3, 5, 8, 10].
The CD117 marker is expressed in up to 95% of all GISTs. Other markers that help immunophenotype and differentiate GIST from other gastrointestinal tumors of mesenchymal origin are: DOG1 (from the English “discovered on GIST 1”), which is detected in 87% of cases, CD34 (receptor for hematopoietic stem cells and endothelial cells) is detected in 60 -70% of tumors, smooth muscle actin - in 30-40%. Some tumors express S100 (5%), desmin (1–2%), and total keratin (1–2%) [3, 7, 10]. It is necessary to note the importance of the marker of proliferative activity Ki-67, the level of expression of which significantly increases with the increase in the “risk of aggressiveness” of GIST, which is used to assess the degree of malignancy and prognosis [11].
According to the recommendations of leading oncology societies (ESMO, NCCN, Canadian Advisory Committee on GISTs, etc.), the diagnosis of GIST is established on the basis of a morphological examination of biopsies with the obligatory immunohistochemical study for the above markers. However, NCCN and ESMO recommend mandatory removal of stromal tumors measuring 2 cm or more, while Canadian experts believe that all formations suspicious for GIST should be removed, even if their size does not exceed 1 cm, since such tumors are prone to metastasis [12 -15].
Currently, evidence has accumulated showing that tumors with mutations localized in the 11th exon of the KIT gene are more sensitive to targeted therapy with Gleevec than tumors that do not have these mutations [9]. Tumors with some mutations in the PDGFRA gene are resistant to Gleevec. Thus, molecular diagnosis of GIST is an important prognostic study that allows us to judge the clinical course, the expected tumor response to the drug and the starting chemotherapy dose. Mutational analysis is not mandatory, however, to clarify the prognosis of the disease and when prescribing targeted therapy, this data is extremely important.
GISTs are not subject to TNM classification; the definition of “risk of disease recurrence” or “risk of tumor aggressiveness” is used to determine prognosis. Over the past 10 years, a large amount of material has been accumulated on this nosology. During this time, a huge number of studies have been conducted to evaluate the influence of various factors on the prognosis of the disease. Currently, the main predictors are the size and location of the tumor, the number of mitoses per 50 fields of view, the nature of the mutation, and the presence of rupture of the tumor capsule before or during surgery.
Treatment. Resectable GIST
Surgery currently remains the main treatment method for patients with localized and locally advanced forms of GIST. When treating stromal tumors of the gastrointestinal tract, it is necessary to strictly adhere to the signs of oncological radicalism [12-15]. Resection of organs is performed at a distance of 2 cm from the macroscopically defined edges of the tumor. Unlike cancerous tumors, lymphadenectomy is not indicated for GIST unless there are clear signs of lymph node involvement. This is due to the fact that the frequency of lymphatic metastasis in stromal tumors does not exceed 3%. It is very important to avoid rupture of the tumor capsule at the stages of mobilization and removal, since in this case the prognosis of the disease becomes comparable to metastatic forms of GIST. Caution should be exercised in laparoscopic interventions for large GISTs due to the high risk of capsule damage. Some authors recommend fundamental removal of the greater omentum for all stromal tumors of the gastrointestinal tract.
Compliance with the principles of radicalism in the surgical treatment of localized and locally advanced GIST allows one to achieve an overall 5-year survival rate in 54-65% of patients (subject to complete cytoreduction). In the presence of residual tumor (surgeries in the scope of R1-R2), the median survival before the introduction of targeted therapy did not exceed 12 months [16-18].
Recurrent and metastatic GIST
Until recently, treatment of patients with recurrent and metastatic forms of GIST represented a serious problem due to the extremely low sensitivity of gastrointestinal stromal tumors to existing cytostatics and radiation therapy. The 5-year survival rate after surgical treatment with complete cytoreduction of the tumor was 35% [19]. The situation changed with the introduction of Gleevec and later Sutent (sunitinib) into clinical practice. Currently, tyrosine kinase inhibitors are the gold standard for the treatment of recurrent, unresectable and metastatic forms of GIST.
The dosage of the drug and the effectiveness of treatment directly depend on the type of mutation in the KIT gene. Tumors with mutations in exon 11 and some mutations in exon 13 are highly sensitive to targeted therapy, so treatment with Gleevec is started at a dosage of 400 mg/day. For mutations in exon 9, the initial dose is increased to 800 mg/day, which is due to a lower objective response rate and worse prognosis. If genetic typing of GIST is not possible, treatment begins with 400 mg, since it is known that most stromal tumors have a mutation in exon 11 (up to 70%) [20, 21]. In case of disease progression at a dose of 400 mg/day, a transition to 800 mg/day is recommended [13-15, 22-27].
Tumors with mutations in the 12th and 18th exons of the PDGFRA gene have increased sensitivity to imatinib, with the exception of the p.D842V mutation, which, on the contrary, indicates resistance. Resistance to Gleevec is also indicated by secondary mutations in the 13th and 17th exons of the KIT gene, which arise as a result of taking the drug after some time. Thus, when choosing a treatment regimen, it is necessary to take into account the type of mutations in the KIT and PDGFRA genes and genotyping of primary tumors, in particular those with a high risk of metastasis, to identify mutant types with primary resistance to imatinib. Analysis of secondary mutations in GIST while taking Gleevec can be performed to monitor drug resistance.
In the works of J. Gold et al. (2007) [4] and S. Blanke et al. (2008) [23] presented the results of treatment of patients with recurrent and metastatic forms of GIST. In the first study, patients received only surgical treatment. At the same time, the overall 2-year survival rate was 41%, and the median survival rate was 19 months. In the second study, when surgical treatment was combined with adjuvant therapy with Gleevec, similar rates were 72-76% and 51-55 months, respectively.
With further progression of the disease on high doses of Gleevec or with the development of uncontrolled side effects, a second line of therapy is indicated. The drug of choice in this case is Sutent, an oral multitarget tyrosine kinase inhibitor with antitumor and antiangiogenic activity [28–30]. The drug has proven effective when taken at a dose of 50 mg/day for 4 weeks followed by a two-week break. According to G. Demetri et al. [28], sutent increased the time to progression from 6.4 to 27.3 weeks (p<0.0001). Partial tumor resorption was observed in 6.8% of patients, stabilization of the process for more than 22 weeks - in 17.4%.
Adjuvant targeted therapy
During surgical treatment of localized and locally advanced GIST, approximately half of patients develop disease relapse within 5 years, which dictates the need for adjuvant therapy in high-risk groups [17]. A number of studies conducted in Europe and the USA have shown the possibility of successful use of imatinib as adjuvant therapy after surgical treatment of stromal tumors. Thus, the randomized, placebo-controlled phase III trial Z9001 (ACOSOG) assessed the effectiveness of adjuvant therapy with Gleevec 400 mg for 1 year in patients with c-KIT-positive GIST compared with placebo. According to the study results, adjuvant therapy significantly increased disease-free survival from 83 to 98%, respectively, compared with placebo (p<0.0001). However, no improvement in overall survival was noted, which may be due to insufficient follow-up [31–33]. Thus, adjuvant targeted therapy for 1 year is recommended for all patients with GIST at high risk of progression. For low-risk tumors, dynamic observation is indicated.
The main criteria when assessing the risk of recurrence of stromal tumors after surgical treatment are the location and size of the tumor, the presence of tumor perforation, the frequency of mitoses and the type of mutation. The worst prognostic factors are tumor localization in the small intestine, size more than 10 cm, mitotic rate more than 5 per 50 fields of view at high microscope magnification, mutation in the 9th exon of the KIT gene [15, 34, 35].
Improvement in disease-free survival alone without improvement in overall survival could not satisfy the investigators, and therefore several protocols were initiated to use Gleevec as adjuvant therapy for a longer period of time. Thus, the EORTC 62024 protocol studied the effectiveness of taking imatinib for 2 years compared with surgical treatment in patients with an intermediate or high risk of relapse. The results of the Scandinavian-German study SSG XVIII/AIO have now been published. According to the presented data, adjuvant therapy with Gleevec for 3 years compared to 1 year statistically significantly increases not only relapse-free, but also overall survival of patients with a high risk of relapse (p = 0.019). At the same time, such therapy is well tolerated by patients, and serious adverse events occur extremely rarely. Thus, the new gold standard in the treatment of this group of patients after surgical treatment is adjuvant therapy for 3 years [36, 37].
Neoadjuvant therapy
A promising direction in the treatment of stromal tumors is neoadjuvant therapy with tyrosine kinase inhibitors followed by surgery. The goal of preoperative intervention is to reduce the tumor mass, increase resectability and the frequency of organ-sparing operations, as well as reduce the risk of relapse [4, 19]. According to R. Andtbacka et al. [38], the use of neoadjuvant therapy with imatinib in a group of patients with recurrent or metastatic GIST can increase tumor resectability in case of response to therapy. Thus, with partial tumor resorption, the frequency of radical operations (R0) was 91%, while with progression during therapy - only 4% (p <0.001). The main indications for neoadjuvant therapy are conditionally resectable locally advanced and metastatic forms of GIST. The duration of preoperative imatinib therapy varies from 6 to 12 months. This time interval was chosen based on data from the EORTC 62024 protocol, which showed that 80% of responses to imatinib therapy were obtained within 6 months after initiation of treatment, and the median time to progression was 18 months [36]. Moreover, according to S. Bonvalot et al. [39], the frequency of complete cytoreductions performed in the period from 6 to 12 months after the start of imatinib therapy is 80%, and in the period from 12 to 18 months - only 20%.
Conclusion
Gastrointestinal stromal tumors are the most common mesenchymal tumors of the gastrointestinal tract. Most soft tissue lesions previously classified as leiomyomas, schwannomas, leiomyosarcomas, and others are now classified as GIST based on the results of immunohistochemical studies. The widespread introduction of molecular diagnostics, as well as the emergence of targeted therapy drugs, have significantly changed approaches to treatment and the prognosis of the disease in patients with GIST.
For localized stromal tumors, surgery remains the mainstay of treatment, supplemented by adjuvant targeted therapy in high-risk groups. In unresectable and metastatic forms, treatment begins with conservative therapy with a further solution to the issue of surgical treatment in case of significant tumor resorption. The use of modern treatment algorithms for patients with GIST, including surgical treatment and targeted therapy, allows us to achieve 5-year survival even with an advanced tumor process.
The main causes of solid formations in cancer
A solid formation is a cancer that can appear in almost any system of the body. However, there are a number of reasons that, according to experts, are peculiar provocateurs and stimulate the appearance and spread of metastases.
Solid formation (cancer) can occur due to the following phenomena:
- unfavorable environmental conditions, especially in densely populated cities and cities with large plants and factories;
- an abundance of stress and excessive psychological stress;
- alcoholism and smoking;
- bad heredity;
- weak immune system;
- frequent fractures and other injuries.
Symptoms
The disease can be asymptomatic for a long time, without disrupting the functioning of nearby organs. The first symptom of a retroperitoneal tumor, with which a patient first consults a doctor, is abdominal pain: from mild - dull and aching, to paroxysmal and intense.
But there are no specific signs; the manifestations are caused not by the type of tumor, but by its localization - in the upper, lower or lateral part of the retroperitoneal space, the proximity of nerves, blood vessels, lymphatic pathways, etc. However, disruption of the functioning of nearby organs develops when the formation reaches an impressive size and begins to compress nearby structures.
Nausea and vomiting, alternating diarrhea with constipation, rumbling and bloating may occur. When the bladder is compressed, urinary dysfunction occurs, and when pressure is placed on the diaphragm, shortness of breath occurs. In some cases, signs of hypothermia and hyperhidrosis of the lower limb - excessive sweating - may appear on the affected side. Compression of large vessels of the retroperitoneal space by the tumor leads to edema of the lower extremities.
During the malignant process, the following are noted: loss of appetite, nausea, fatigue, and at a later stage - weight loss, fever. Tumors of the retroperitoneal space of a malignant nature can metastasize, most often metastases are found in the liver and lungs.
Classification of solid formations
Any solid formation (oncology) belongs to one of the following categories: benign or malignant.
Benign tumor
It grows slowly and can decrease on its own without additional intervention. There are no metastases.
The main problem that this solid formation (cancer) poses is the compression of neighboring organs or tissues.
Malignant tumor
It consists of tirelessly dividing cells that have changed their appearance and structure and can grow to considerable sizes.
The phenomenon manifests itself in an extremely aggressive manner, spreading metastases even in the earliest stages of the disease.