Facial nerve, anatomy
The facial nerve, nervus facialis , the 7th pair of cranial (cranial) nerves is a motor nerve.
The facial nerve innervates the facial muscles of the face (except for the musculus levator palpebre superioris), as well as the muscles of the auricle and skull, the posterior belly of the digastric muscle (musculus digastricus), the stylohyoid muscle (musculus stylohyoideus), the stapedius muscle (musculus stapedius), the subcutaneous muscle of the neck (musculus platysma).
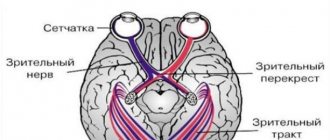
The nucleus of the facial nerve is located on the border of the lower part of the pons with the medulla oblongata, outward and anterior to the nucleus of the abducens nerve. The axons of the cells of this nucleus rise in the dorsomedial direction to the bottom of the rhomboid fossa, then loop around the nucleus of the abducens nerve located here, forming the internal knee of the facial nerve in the area of the facial tubercle . The root of the facial nerve exits the base of the brain in the cerebellopontine angle between the pons and the medulla oblongata, lateral to the olive, then, together with its companions and the cochlear part of the 8th pair of cranial nerves, enters the internal auditory foramen (miatus acusticus internus), then the nerve and its companions enter facial canal (canalis facialis) of the pyramid of the temporal bone (fallopian canal). The canal initially has a horizontal direction (parallel to the apex of the temporal bone pyramid), then bends vertically. It then opens at the base of the skull with a stylomastoid opening (foramen stylomastoideum). The bend of the facial nerve in its canal is called the “external genu of the facial nerve.” In this place there is the knee ganglion (ganglium geniculi), where the cells of the first taste sensitivity neuron for the intermediate nerve are located. After emerging from the stylomastoid foramen, the facial nerve penetrates the parotid gland and divides into many terminal branches to innervate the corresponding muscles, forming the pes anserinus. The companions of the facial nerve in the canal are the parasympathetic lacrimal fibers - the greater petrosal nerve (nervus petrosus major) and the intermediate nerve (nervus intermedius), the 13th pair of cranial nerves, the Wriesberg nerve.
Parasympathetic lacrimal fibers originate from the secretory nucleus, which is located near the nucleus of the facial nerve. Together with the facial nerve, they enter the facial canal, then are the first to leave it as part of the nervus retrosus major, which innervates the lacrimal gland. Loss of function of the greater petrosal nerve is accompanied by the following symptoms - dry eye, eye irritation, lacrimation.
The intermediate nerve is mixed, consists of efferent parasympathetic salivary fibers for the sublingual and submandibular salivary glands, afferent taste fibers for the anterior 2/3 of the tongue. Salivatory fibers originate from the superior salivatory nucleus (nucleus salivatorius superior), leave the brain in the cerebellopontine angle and enter the facial canal next to the facial nerve, then leave the canal in its descending part as part of the chorda tympani (chorda tympani). Sensitive taste fibers begin from the cells of the knee ganglion, the dendrites of which go in the facial canal along with the facial nerve, then depart from it in the descending part of the canal, participate together with salivary fibers in the formation of the tympanic chord, then enter the system of the 3rd branches of the trigeminal nerve (nervus lingualis ) and reach the taste buds of the anterior 2/3 of the tongue. The axons of the cells of the knee bridle leave the pyramid of the temporal bone through the internal auditory foramen, pass through the cerebellopontine angle and end in the taste nucleus of the solitary tract (nucleus tractussoliterii), common with the glossopharyngeal nerve, located in the medulla oblongata. Damage to the intermediate nerve and the chorda tympani, which is its continuation, leads to hypofunction of the sublingual and submandibular salivary glands and impaired taste in the anterior 2/3 of the tongue. Between the two companions in the facial canal, motor fibers are separated from the trunk of the facial nerve, which form the stapedius nerve (nervus stapedius). The stapedius nerve penetrates the tympanic cavity and innervates the stapedius muscle, which provides a certain degree of fixation of the stapes and tension of the tympanic membrane, which creates conditions for the best audibility. Damage to the stapedius nerve is accompanied by a symptom such as hyperacusis. Hyperacusis is an increased unpleasant perception of sounds, especially low tones.
The first to leave the facial canal is the facial nerve's companion, the greater petrosal nerve. The second branch of the facial nerve to leave the facial canal is the stapedius nerve. The third to leave the facial canal is the companion of the facial nerve - the intermediate nerve in the form of the chorda tympani.
There are features of connections between the facial nerve and the cerebral cortex - the lower third of the precentral gyrus. The upper half of the nucleus, which provides innervation to the facial muscles of the upper part of the face, has a bilateral cortical representation due to the partial supranuclear decussation of the corticonuclear fibers. Fibers to the lower half of the nucleus, from which the facial muscles below the palpebral fissure are innervated, originate from the opposite hemisphere. This point is an important criterion in making a topical diagnosis.
Facial nerve: symptoms, lesion syndromes
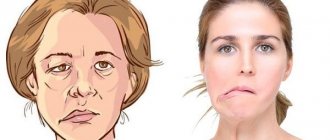
When the trunk of the facial nerve, the root of the facial nerve or the nucleus of the facial nerve is damaged, paresis of the facial muscles (muscle paresis) of the same half of the face develops - prosoplegia. Facial asymmetry occurs, which is pronounced even at rest. The entire affected side is motionless and mask-like. The forehead folds and nasolabial folds are smoothed. The palpebral fissure is widened. The corner of the mouth is downturned. Due to loss of function of the circular muscle of the eye (musculus orbicularis oculi), the eye does not close. This is lagophthalmos , or hare's eye. When you try to close your eyes, the eyeball on the affected side turns upward, the iris goes under the upper eyelid - Bell's symptom. With mild paresis of the orbicularis oculi muscle, the palpebral fissure closes, but less tightly than on the healthy side, the eyelashes remain visible (eyelash symptom). When the normal function of the lacrimal gland is preserved, lagophthalmos is usually accompanied by lacrimation, which is caused by difficulty in moving tears to the lacrimal canal due to insufficient adherence of the lower eyelid to the eyeball and impaired absorption due to displacement of the opening of the canal. Also, lacrimation is facilitated by the strengthening of the tear reflex due to the constantly open eye. Inflammatory phenomena, conjunctivitis, and keratitis often develop due to irritation of the eye membranes by air flow and dust.
The asymmetry of the face increases sharply when teeth are shown. The corner of the mouth is pulled back and it is skewed towards the healthy side - this is the phenomenon of the exclamation point, it is associated with paralysis of the musculus risorius. Due to the weakness of the orbicularis oris muscle, whistling and stretching of the lips into a tube are impossible. The patient often has difficulty speaking and eating. Liquid food on the affected side spills out of the mouth, thick food gets stuck between the cheek and teeth. When frowning and wrinkling the forehead, folds do not form on the side of paralysis, it is impossible to puff out the cheeks, and there is no tension on the musculus platysma of the neck. The brow reflex, nasopalpebral reflex, corneal reflex, and conjunctival reflex are lost or weakened. If damage to the facial nerve occurs in a child of the first year of life, then the sucking reflex, proboscis reflex, and search reflex are reduced. As with any peripheral paralysis, atrophy of the facial muscles is possible. When studying electrical excitability and myography, a degeneration reaction is noted.
Peripheral paralysis of the facial muscles is sometimes accompanied by pain in the face, ear, and mastoid process. The pain is associated with the phenomenon of repercussion. Repercussion is the irradiation of excitation from the motor branches of the facial nerve to the sensory branches of the trigeminal nerve.
Prolonged peripheral paralysis can lead to the development of contracture of the affected muscles, which is manifested by a narrowing of the palpebral fissure on the affected side and a pulling of the mouth when baring teeth towards the affected affected side. Symptoms of incipient contracture are often pathological synkenesis of the facial muscles - ocular synkenesis. They are characterized by the following symptoms. The closing of the eyes is accompanied by movement of the corner of the mouth or baring of the teeth. Baring your teeth causes the eye on the affected side to close.
In pathological processes that cause irritation of the nucleus or fibers of the facial nerve, facial hemispasm is observed - this is squinting the eye and pulling the mouth and tip of the nose to the affected side with simultaneous contraction of the chin muscles and tension of the subcutaneous muscle of the neck. Signs of irritation of the facial nerve are also tics of facial muscles and Chvostek's sign.
Symptoms
Any damage to the facial nerve can lead to a number of problems, but the most common symptoms are:
- Paralysis on one side of the face
- Face twitching
- Decreased tolerance to high-frequency sounds
- Deterioration of taste sensations
- Facial expressions do not correspond to emotional expression (one side may remain abnormally unchanged, the other side will reflect emotions)
- Difficulty closing the eye voluntarily (this can cause damage to the retina and conjunctiva and may result in loss of vision in one eye)
- Weakness and headache
- Difficulty eating (food may fall out of the mouth)
- Feeling of facial stiffness and sagging
Diagnosis of the level of damage to the facial nerve
Isolated lesions of the nucleus of the facial nerve are observed quite rarely. It is manifested by total paresis of the facial muscles and occurs in the pontine form of polio.
More often, pathological foci localized in the pons are more common and lead to the involvement of the nucleus of the facial nerve, radicular fibers, and pyramidal tract in the process, which is manifested by alternating Millard-Hübler syndrome. Simultaneous damage to the nucleus of the abducens nerve is manifested by alternating Foville syndrome.
When the pathological process is localized in the cerebellopontine angle, the symptoms of damage to the facial nerve are combined with damage to its companions (the intermediate nerve and the greater petrosal nerve) and the vestibulocochlear nerve. Paralysis of facial muscles in these cases is accompanied by dry eyes - xerophthalmia, impaired taste in the anterior 2/3 of the tongue on the affected side. Xerostomia may be felt - dry mouth, but more often it does not occur due to the functioning of other salivary glands (parotid, sublingual, submandibular on the healthy side). Hyperacusis does not occur due to concomitant damage to the cochlear nerve. Hearing loss or deafness is more common. There may be signs of dysfunction of the trigeminal nerve and abducens nerve located in the immediate vicinity, as well as cerebellar disorders.
When the facial nerve is damaged in the facial canal above the origin of the greater petrosal nerve, dry eyes, taste disorders and hyperacusis develop simultaneously with paralysis of the facial muscles.
The lesion after the departure of the greater petrosal nerve is accompanied by increased lacrimation, taste disturbance, and hyperacusis.
When the facial nerve is damaged below the origin of the stapedius nerve, but above the origin of the chorda tympani, paralysis, lacrimation, and taste disturbance are observed.
Damage to the nerve in the bony canal below the origin of the chorda tympani or after exiting the stylomastoid foramen causes only paralysis with lacrimation.
When the process is localized in the area of the outer knee of the facial nerve with involvement of the knee node, Hunt's syndrome can be detected - this is paresis of the facial muscles (facial muscles), severe pain and herpetic rashes in the area of the auricle (ear).
Sometimes there are cases of bilateral damage to the facial nerve. Bilateral damage to the facial nerves is called diplegia facialis. The patient's face is mask-like, his eyes are half-open, it is impossible to form his lips into a tube or close his mouth.
Diseases of the peripheral nervous system
Diseases of the peripheral nervous system (neuritis, polyneuritis, neuropathy).
Among the most frequently diagnosed diseases of the human peripheral nervous system, there are several forms of neuritis, cries, neuralgia, as well as all sorts of these pathologies, which have different topography and most often manifest as sharp and sometimes mild pain of a permanent nature. By the way, such a common radiculitis is also a peripheral lesion.
Diseases of the peripheral nervous system are the most common in neurological clinics and account for up to 50% of outpatients. Not presenting, as a rule, a threat to the lives of patients, they are the main cause of disability.
The causes of damage to the peripheral nervous system can be acute and chronic infections, trauma, intoxication, hypovitaminosis, ischemia, hypothermia, compression, and degenerative changes in the spine.
Pathomorphologically, when a peripheral nerve is damaged, swelling and disintegration of the myelin sheath, proliferation of Schwann cells are observed first, and then structural changes occur in the nerve fibers themselves. In this case, vasodilation, exudation, perivascular edema, and hemorrhages are noted in the connective tissue sheaths of the nerve.
If inflammatory phenomena predominate in etiopathogenesis, then peripheral pathology is designated with the ending “it”, if metabolic - then “ia”. If the cause of the disease is degenerative changes in the spine, then the diagnosis is supplemented with the words “vertebrogenic”, “spondylogenic”.
Pathologies of the peripheral nervous system by location
Depending on the location and pathogenesis, the following diseases of the peripheral nervous system are distinguished.
Neuritis (neuropathy)
- a disease in which pathomorphological changes in the nerve are accompanied by disturbances in motor, sensory and autonomic functions. Neuralgia is characterized by attacks of pain along the nerve without signs of organic damage.
This pathology of the peripheral nervous system is caused mainly by metabolic, degenerative processes in the nerve fiber, with minor inflammatory changes in it.
- Polyneuritis
(polyneuropathy) is damage to many nerves. - Plexitis
is a lesion of the nerve plexus. - Ganglionitis
is a lesion of the intervertebral nodes. - Radiculitis
is a lesion of the spinal cord roots. - Radiculoneuritis
is a simultaneous lesion of the spinal cord roots and nerve trunks. - Myeloradiculoneuritis
- damage to the spinal cord, roots and nerve trunks.
The most common forms of disorders of the peripheral nervous system are vertebrogenic pathology (osteochondrosis), neuritis (neuropathy) and neuralgia. Moreover, the most often affected are those nerves whose trunks pass through narrow bone canals - facial, trigeminal, sciatic.
Peripheral nervous system disorders: facial neuritis
Neuritis of the oculomotor nerve.
The disease is predominantly of vascular, inflammatory, diabetic origin. Observed in intracranial tumors.
Such peripheral neuritis is manifested by drooping of the upper eyelid (ptosis), dilation of the pupil (mydriasis), divergent strabismus and double vision (diplopia).
Treatment
according to the etiology of the disease, vitamin therapy, biostimulants.
Neuropathy (neuritis) of the facial nerve.
Lesions of other cranial nerves are more common.
The cause of the disease can be hypothermia, infection, trauma, inflammation of the ear or meninges, tumors of the base of the skull. Since the trunk of the facial nerve passes through a narrow bone canal and its terminal branches are located superficially, the nerve is easily injured, and during inflammatory processes tissue swelling develops, which leads to compression of the nerve and the vessels that supply it.
This peripheral nerve neuritis develops acutely or subacutely. There are peripheral and central facial palsy.
Peripheral paralysis is characterized by facial asymmetry - the face is skewed towards the healthy side. On the affected side, the skin folds are smoothed, the eye does not close (lagophthalmos), when trying to close the eye, the eyeball turns up (Bell's sign), food gets stuck behind the cheek, teeth are grinned more in the healthy direction. Dry eyes or watery eyes, disturbances in hearing, taste and salivation may occur.
With central paralysis, only smoothness of the nasolabial fold and drooping of the corner of the mouth are observed.
A complication of this disease of the peripheral nerves can be persistent contracture of the affected muscles and tonic muscle spasm - facial hemispasm.
Diagnostics
is based on clinical data and to clarify the diagnosis, an LOP examination, skull radiography, and computed tomography are sometimes performed.
Treatment
This disease of the peripheral nervous system must begin early and correspond to the cause of the lesion. For infectious-inflammatory origin, salicylates, methenamine, indomethacin, acyclovir, and prednisolone are prescribed.
In parallel with the etiological treatment, vasodilators are prescribed: dibazol, aminophylline, trental, nicotinic acid, decongestants (Lasix, furosemide, hypothiazide), vitamins
From 5-7 days of illness, thermal procedures (UHF, paraffin, ozokerite) are prescribed.
In the recovery period, prozerin, aloe, FiBS, ultrasound with hydrocortisone are used on the mastoid process and the affected half of the face, electrical stimulation of the facial muscles, exercise therapy, acupuncture massage, and acupuncture.
If there is no effect within 12 months, they resort to neurosurgical intervention.
Care consists of instilling moisturizing eye drops and wearing glasses during the day. At night, apply eye ointment and cover your eyes with a bandage.
Prevention:
avoid hypothermia, anti-epidemic measures.
Neuritis of the peripheral nerves of the extremities: symptoms and treatment of neuropathies
Neuropathies of the peripheral nerves of the extremities are most often caused by external trauma or compression of the nerve trunk. It is possible that the nerve in the bone canal may be pinched, compressed in deep sleep, when throwing back the arm, during prolonged anesthesia, or when applying a tourniquet. Also, the cause of neuritis can be infections, ischemia, and intoxication.
Radial nerve neuropathy.
It manifests itself as a symptom of a “dangling hand,” while the patient cannot straighten the arm at the wrist and elbow joints, cannot abduct the thumb and supinate the palm, the carporadial reflex decreases, and sensitivity on the dorsal surface of the 1st, 2nd, and 3rd fingers is impaired.
Ulnar nerve neuropathy is characterized by a “bird’s foot” deformity of the hand as a result of paralysis and atrophy of the small muscles of the hand; violation of adduction and abduction of fingers; pain and decreased sensitivity on the 5th and 4th fingers.
Median nerve neuropathy.
It manifests itself as a violation of flexion of the hand and fingers in the interphalangeal joints, opposition of the thumb; impaired sensitivity on the lateral surface of the palm and 1-4 fingers. Also symptoms of such peripheral neuropathy are atrophy of the muscles of the forearm and flattening of the palm like a “monkey’s paw”. The patient cannot clench his fingers into a fist. Characterized by severe pain with a causal tinge and pronounced vegetative-vascular and trophic disorders (hyperhidrosis, hyperkeratosis, brittle nails, atrophy and cyanosis of the skin).
Neuropathy of the external cutaneous nerve of the thigh (Roth disease)
. Occurs as a result of infection, intoxication (alcohol, nicotine, diabetes), atherosclerosis, and long-term nerve injury. This peripheral nerve neuropathy manifests as paresthesia and pain along the outer thigh. The pain is worse at night and especially in an upright position and when walking. Hyper- or hypoesthesia is determined along the outer surface of the thigh.
Neuropathy (neuritis) of the peroneal nerve.
It is characterized by drooping of the foot and the inability to straighten it and the toes. The patient cannot stand on his heel. The muscles of the anterior surface of the lower leg atrophy. Sensitivity on the outer surface of the lower leg and the dorsum of the foot is impaired. The gait becomes step-like, “cock-like.”
Neuropathy (neuritis) of the tibial nerve.
Leads to impaired flexion of the foot and fingers. The patient cannot stand on his toes. The muscles of the back of the lower leg atrophy, and the Achilles reflex fades. Sensitivity disturbances are noted along the back surface of the lower leg and sole; severe pain and vegetative-trophic disorders.
Treatment
peripheral neuropathy of the extremities includes the use of vitamins B, C, nicotinic acid, aloe extract, proserin, and, if necessary, analgesics.
Physiotherapy is widely used:
- UHF
- Ural Federal District
- Electrophoresis
- Ultrasound
- Laser and magnetic therapy
- Massage
- Exercise therapy
Care consists of preventing persistent paresis and contractures (suspension, bandages, splints for fixing the limb, orthopedic shoes), teaching the patient the elements of therapeutic exercises. If there is no recovery within two months, surgery is indicated.
Lesions of peripheral nerves: neuralgia
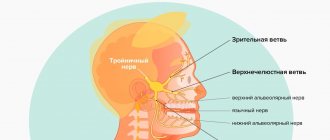
Trigeminal neuralgia.
A disease of peripheral nerves with severe pain and a relapsing course.
The cause may be infections, intoxications, atherosclerosis, hypothermia, pathological processes at the base of the skull, in the paranasal sinuses, teeth, orbits, and narrowing of the bone openings.
The main symptom of this disease of the peripheral system
- attacks of sharp shooting pain in the zone of innervation of one or more branches of the nerve. The pain lasts a few seconds, less often - minutes. Pain is provoked by excitement, chewing, talking, touching the tongue to sensitive points (triggers) of the mucous membrane of the mouth and gums. Therefore, patients may develop obsessive fear, and in order not to provoke an attack, they freeze, hold their breath, and are afraid to make the slightest movement. Attacks may be accompanied by redness of half the face, cramps of facial muscles, lacrimation, and copious nasal discharge. During the interictal period, one can detect hyperesthesia in the area of the affected branch and pain at the point of its exit.
When the trigeminal nerve ganglion is damaged, constant burning pain and herpetic rashes are observed. Herpetic keratitis is especially dangerous when the first branch of the nerve is affected.
Treatment
primarily aimed at eliminating the cause of the disease.
Next, analgesic and anti-inflammatory drugs are prescribed (analgin, sedalgin, reopirin, indomethacin, pentalgin):
To suppress neuralgic paroxysms, carbamazepine (finlepsin), trimethin, convulex clonazepam, neurontin, lamictal are used:
They also stimulate metabolic processes (retabolil, solcoseryl, actovegin, B vitamins): Baclofen is also used: For herpetic rashes, acyclovir, herpesin are prescribed:
Physiotherapy includes UHF, ultraviolet irradiation, diadynamic currents, SMT, novocaine electrophoresis, laser therapy..
Care
consists in creating a protective regime, preventing the patient from hypothermia and feeding him non-hot, well-purified food.
Neuralgia of the pterygopalatine ganglion (Slader syndrome).
The disease is caused by the same reasons as trigeminal neuralgia. Symptoms of this disease of the peripheral nervous system are attacks of pain in the eye, root of the nose, jaw, teeth spreading to the tongue, soft palate, ear, and cervicohumeral area. Sometimes the pain covers half of the head, noise, dizziness, and ringing in the ear appear. At the same time, half of the face turns red, tearing and salivation intensify. The attack lasts up to one hour.
Treatment and care
are carried out according to the same scheme as for trigeminal neuralgia. As a local therapy, the middle nasal passage is lubricated with novocaine.
Neuralgia of the glossopharyngeal nerve.
Occurs more often in older people. Causes: atherosclerosis, tumors, scars, osteophytes. This disorder of the peripheral system is characterized by attacks of severe pain in the root of the tongue, tonsils, radiating to the ear, eye, and neck. In this case, the patient experiences dry mouth, cough, and excessive salivation.
Treatment
carried out as with trigeminal neuralgia; locally - lubricating the root of the tongue with cocaine.
Neuralgia of the occipital nerve.
Caused by hypothermia, infections, degenerative processes in the spine, arachnoiditis and tumors of the posterior cranial fossa. The disease is characterized by attacks of pain in one half of the back of the head, radiating to the ear, neck, shoulder girdle, and shoulder blade. The pain intensifies with movement, coughing, sneezing. Possible forced head position. With this disorder of a peripheral nature, pain in the nerve exit points and sensitivity disorders in the occipital area are noted.
Treatment
underlying disease, pain medications, vasodilators, vitamins, locally - UV irradiation, UHF.
Intercostal neuralgia.
It can be primary and secondary, i.e. arising against the background of other diseases, especially with pathology of the spine (osteochondrosis, tumors, tuberculosis) and internal organs (lungs, pleura, liver).
The disease is characterized by girdling, shooting pains spreading from the spine along the intercostal spaces around the chest. The pain intensifies with movements and deep breaths. There are sensitivity disorders in the area of innervation of the intercostal nerves, pain in the paravertebral and intercostal points. Loss of abdominal reflexes and paresis of the abdominal muscles are possible. When the intervertebral ganglion is involved in the process, symptoms of herpes zoster appear. To clarify the diagnosis, a thorough examination of the patient is necessary in order to exclude the secondary nature of neuralgia.
Treatment includes eliminating the cause of the disease, painkillers (analgin, baralgin, diclofenac, indomethacin):
Anticonvulsants (finlepsin, 0.2 g 1-2 times a day):
Vitamins, physiotherapy (UHF, DDT),
Care
provides for the creation of a gentle regime, the choice of a comfortable position, and the prevention of hypothermia.
Shingles (ganglionitis, herpetic intercostal neuralgia).
The disease is caused by the neurotropic herpes zoster virus and is provoked by hypothermia. In the spinal nodes and their cranial analogues, an inflammatory process develops, spreading to the nerves and roots.
The disease begins with general malaise, fever and pain in the area of innervation of the affected ganglion (most often in the thoracic region). After 2-3 days, redness and rashes of very painful blisters filled with serous fluid appear at the site of pain. The vesicles often fester, forming pustules that become covered with a crust that falls off after a few days.
When the gasserian node is damaged, rashes appear on the skin of the forehead, upper eyelid, bridge of the nose and on the membranes of the eye, which can result in keratitis and blindness.
Some patients who have had herpes zoster experience pain for a long time (postherpetic neuralgia) and relapses are possible.
Treatment includes antiviral drugs (acyclovir 0.8 x 3, retrovir 0.25 x 5, valacyclovir), detoxification (hemodez), dehydration (furosemide), chimes, analgesics (azafen 0.025 x 6, pyrazidol 0.05 x 3, mexiletine , finlepsin, amitriptyline, herpesin):
Tebrofen ointment, gassipol, and ultraviolet radiation are used topically.
Polyneuritis and polyneuropathy of peripheral nerves
Polyneuritis
- multiple lesions of peripheral nerves of infectious origin.
Polyneuropathy
- toxic damage to the nerves as a result of intoxication of the body, metabolic disorders, allergic reactions, circulatory disorders. If, along with the nerves, their radicular part is affected, then polyradiculoneuritis is determined.
Anatomically, with polyradiculoneuritis, inflammatory changes (edema, hyperemia, infiltration) of the roots are determined, and signs of myelin decay and degeneration of the axial cylinders are visible in the peripheral nerves. Moreover, if the pathological process is limited to mesenchial formations of the membranes and vessels, then this is interstitial neuritis. If it is accompanied by damage to nerve fibers (demyelination, disintegration of axial cylinders), then it is interstitial-parenchymal neuritis. With polyneuropathies, degenerative changes in nerves occur with a predominance of decay of their myelin sheaths or nerve fibers.
Polyneuritis and polyneuropathy are manifested by pain and paresthesia in the distal parts of the extremities, peripheral paralysis, sensitivity disorders of the “glove” and “sock” type and vegetative-trophic disorders (dryness, thinning of the skin or its hyperkeratosis, cyanosis, trophic ulcers).
Infectious polyneuritis of viral etiology is characterized by an acute onset with general malaise, fever, pain and paresthesia in the extremities.
Subsequently, weakness, atrophy, paralysis of the muscles of the arms and legs, and sensory disturbances develop. The nerve trunks are sharply painful on palpation. Reversal of symptoms is slow.
Treatment includes antiviral drugs, antibiotics, analgesics, corticosteroids, vitamins, and biostimulants.
Acute infectious polyradiculoneuritis usually occurs in the cold season and begins acutely with a rise in temperature, catarrhal symptoms, pain and paresthesia in the distal extremities. Sensitivity disorders of the peripheral type, pain in the nerve trunks, tension symptoms, distal paralysis and vegetative-vascular disorders are determined.
One of the most common forms of multiple lesions of the nervous system is acute infectious Guillain-Barré polyradiculoneuritis. The disease begins acutely with a rise in temperature and catarrhal symptoms, usually in the cold season. Patients develop rapidly increasing weakness in the legs, difficulty walking, and pain along the nerve trunks.
Characterized by symmetrical flaccid paralysis, starting from the lower extremities and covering the muscles of the trunk, upper extremities, neck, lesions of the cranial nerves, sensitivity disorders and sharp protein cell dissociation in the cerebrospinal fluid. The course of this form of the disease is benign.
Another type of polyradiculoneuritis is ascending Landry's palsy.
, in which the anterior roots are predominantly affected. Characterized by an acute onset and rapid course of the disease. The disease begins with paresthesia, pain, weakness, and paralysis of the legs, which quickly, within 2-3 days, spread to the upper limbs and cranial nerves, primarily the bulbar ones. In this case, speech and swallowing are impaired, breathing and cardiac problems occur. Death is common.
Treatment consists of suppressing the autoimmune inflammatory reaction (prednisolone, or its analogues, intravenous bolus up to 1.5-2.1 g per day for the first 3 days, followed by a dose reduction and switching to tablet drugs), administration of antibiotics (benzylpenicillin up to 20 million units per day, gentamicin, rifampicin) and hexamethylenetetramine: Reducing pain (analgin, voltaren): Detoxification (hemodez, glucose): Improving neuromuscular transmission (prozerin intramuscularly 1-2 ml twice a day, galantamine, ATP, B vitamins) :Immunoglobulin and plasmapheresis are also used:
If swallowing is impaired, glucose, albumin, and hydrolysine are administered intravenously; If breathing is impaired, resuscitation measures are carried out. After the acute phenomena subside, ultraviolet irradiation, UHF sessions, light massage, passive movements are carried out, biostimulants and vitamins are administered. 2-3 months after the process has subsided, hydrogen sulfide and radon baths, mud applications, and exercise therapy can be prescribed. Diphtheria polyneuritis occurs two to three weeks after diphtheria. It mainly affects the cranial nerves - the vagus, facial and abducens. The appearance of bulbar disorders is especially dangerous. After recovery, the voice may remain deaf for many years. Treatment is carried out by urgent administration of anti-diphtheria serum (5-10 thousand units). To prevent an anaphylactic reaction, 0.5-1.0 ml of serum is first injected under the skin, and after 12-24 hours the entire dose is injected.
Allergic (anti-rabies) polyneuritis
is a consequence of an allergic reaction to the vaccine. After the start of vaccinations, the patient develops dizziness, weakness, dyspepsia, and diffuse pain. Then the temperature rises; vomiting, uncontrollable, severe headache appear, flaccid paralysis of the limbs and pelvic disorders develop. Reversal of symptoms is rapid.
Diabetic polyneuropathy develops against the background of hyperglycemia.
It is characterized by paresthesia, itching and pain in the legs, sensitivity disorders in the distal extremities, and extinction of the Achilles and knee reflexes. Possible damage to the oculomotor nerves and autonomic ganglia.
Treatment includes correction of hyperglycemia (diabetes, insulin), vitamins, trental, coplamine, nootropics, analgesics, biostimulants, anabolic steroids, lipostabils, thioctacid:
Alcoholic polyneuropathy
develops subacutely with chronic alcohol intoxication. The disease begins with paresthesia, burning pain in the feet against the background of pronounced autonomic disorders (cyanosis, coldness, sweating) of the extremities.
In the distal sections, paresis develops, superficial and deep sensitivity is impaired (sensitive ataxia), and muscle atrophy appears. Korsakov's syndrome is very characteristic - loss of memory for recent and current events, confabulation, temporal and spatial disorganization.
Treatment consists of eliminating alcohol, prescribing large doses of B vitamins, benfogamma, mil-gamma, vasodilators (spasvin) and other drugs used for polyneuropathies.
Polyneuropathy in pregnant women is associated with impaired vitamin metabolism and liver failure. Characterized by paresis, peripheral sensitivity disorders, extinction of reflexes, disorders of autonomic innervation in the form of hyperhidrosis, coldness of the extremities. Possible Landry syndrome.
Lesions of the peripheral nervous system: plexitis
Cervical plexitis
Caused by infections, tumors, tuberculosis and injuries to the cervical spine. It manifests itself as pain and sensory disturbances in the back of the head, ear, neck, upper scapula and shoulder. Disturbances in the function of the phrenic nerve are characteristic (breathing problems, hiccups, complete or partial immobility of the diaphragm).
Brachial plexitis
occurs after shoulder injuries, collarbone fractures, infections, pathologies of the spine and lungs. Depending on the location of the lesion, upper, lower and total brachial plexitis are distinguished.
Upper (Duchenne-Erb palsy)
manifested by pain in the upper third of the shoulder, decreased reflex with the biceps, difficulty in shoulder abduction, supination, flexion of the arm at the elbow joint, as well as impaired sensitivity on the outer surface of the shoulder and forearm.
Lower (Dejerine-Klumpke palsy)
characterized by pain and sensitivity disorders on the inner surface of the shoulder and forearm, paresis and atrophy of the muscles of the hand and forearm, and a decrease in the carporadial reflex. Possible Horner-Bernard syndrome.
Total plexitis
is rare, characterized by pain in the supra- and subclavian region, radiating to the arm, loss of reflex
c, paresis and sensory impairment in the entire arm, severe vegetative-vascular disorders.
Lumbosacral plexitis
occurs as a result of infections, intoxications, diseases of the pelvic and abdominal organs, during pregnancy, during pathological childbirth and injuries to the spine and pelvic bones. Clinically, plexitis is manifested by pain and loss of sensitivity in the buttock, thigh and lower leg, loss of the knee and Achilles reflexes, paresis of the foot and atrophy of the muscles of the buttocks and thighs.
Treatment is similar to that of polyneuropathy.
« Back to previous page
Facial nerve: treatment in children
Damage to the facial nerve in children is more common than damage to other cranial nerves, which is due to its anatomical features. The facial nerve is supplied with blood from the external carotid artery system, therefore, when the head is hypothermic, spasm of the external carotid artery leads to nerve ischemia, swelling and compression of the facial nerve. Compression of the facial nerve develops especially easily when the process is localized in the narrow canal of the temporal bone pyramid. The facial nerve canal is connected to the tympanic cavity and the pneumatic cells of the mastoid process. The outflow of lymph from the trunk of the facial nerve occurs in the cervical lymph nodes. In childhood, damage to the cervical lymph nodes is often observed.
Pathogenesis
The triggering factor for FLN is irritation of the vessels of the craniocervical region, which contributes to the development of vasospasm of the vertebral and branches of the external carotid artery, which leads to primary ischemia of the FLN root. Increasing disturbances of microcirculation in the structures of the FN lead to anoxic swelling of the nerve . This, in turn, leads to compression (squeezing) of the nervous tissue in the facial (fallopian) canal of the temporal bone, disruption of neuromuscular conduction caused by blockade of the process of release of acetylcholine and a disorder in the interaction of acetylcholine with receptors located on the postsynaptic membrane. As disorders increase in the nervous tissue, secondary ischemia of the FN develops.
Facial nerve: causes of damage, causes of neuritis, neuralgia, neuropathy, paresis, paralysis
The main causes of damage to the facial nerve a are inflammatory diseases (diseases) leading to primary damage to the facial nerve and its involvement in the process secondary to pathological changes in adjacent formations. Meningitis, arachnoiditis of the cerebellopontine angle, inflammatory processes in the area of the eustachian tube (eustacheitis) and mastoid process (mastoiditis), inflammation of the ear (otitis), jaw arthritis, lymphadenitis, mumps can cause the development of neuritis, paresis, paralysis, inflammation of the facial nerve. Also the cause of damage to the facial nerve are primary and secondary polyradiculoneuritis. Traumatic damage to the facial nerve occurs during traumatic brain injury with a fracture of the base of the skull in the area of the temporal bone, during surgical operations on the ear. The cause of paralysis and paresis of the facial nerve in children can be birth trauma, the application of obstetric forceps, or facial presentation. The facial nerve suffers from various tumors of the cerebellopontine ganglion region. Neuroma of the facial nerve, Recklinghausen's neurofibromatosis, tumor of the parotid salivary gland, infiltration due to leukemia are also causes of damage to the facial nerve.
In rare cases, congenital aplasia of the facial nerve nucleus and congenital narrowness of the facial nerve canal occur.
Central palsy - facial nerve
Central paralysis of the facial muscles (facial muscles) is observed as a result of damage to the corticonuclear fibers going to the nucleus of the facial nerve. Central paralysis is characterized by dysfunction of the muscles of the lower half of the face, which have unilateral cortical innervation. The main symptom of central paralysis is the smoothness of the nasolabial fold on the side opposite to the lesion. In some patients with central paralysis of the facial muscles, mild deficiency of the orbicularis oculi muscle can be detected. Central paresis of the facial muscles is usually observed in combination with central hemiparesis, or hemiplegia. In contrast to peripheral paralysis, with central paralysis of the facial muscles, the conjunctival reflex, brow reflex, and corneal reflex are preserved, and there is no degeneration reaction.
Primary neuritis of the facial nerve
Primary facial paralysis is caused by herpes viruses, mumps, enteroviruses, and adenoviruses. Bell's palsy can develop with general or local hypothermia of the face. Bell's palsy is characterized by acute development within 3 to 24 hours. The leading role in the development of Bell's palsy belongs to ischemia, which develops due to vasospasm, or vasodilation with the development of swelling of the facial nerve and compression of the nerve.
Often, neuritis of the facial nerve occurs for no apparent reason against the background of absolute complete health. Sarklinik observed many cases where the first symptoms of facial neuritis appeared after a person slept, at the moment of awakening. This may be due to the activation of chronic infection with weakened immunity, the development of various allergic reactions.
How to speed up recovery
In order for the restoration of damaged nerves to occur faster, it is advisable to supplement the treatment prescribed by the doctor with gymnastics. It allows you to use the areas of the face affected by the affected nerve. The set of exercises consists of puffing out the cheeks, moving the tongue to the sides, frowning the eyebrows and forehead, circular movements of the eyes, pulling in and out the lips, cheeks and many other movements.
At home, you can warm up by applying a thick fabric bag to the sore spot on the face, into which salt or sand heated in the microwave is poured. The duration of warming up should be no more than 30 minutes, the procedure is carried out before bedtime for a month. However, such procedures, like physical therapy, can be started no earlier than a week after the onset of inflammation.
It is advisable for patients with neuritis to avoid hypothermia and exposure to drafts, to protect themselves from viral diseases and stress, and also to ensure that their diet contains enough protein foods, vegetables and fruits.
Neuritis of the facial nerve secondary
Secondary neuritis of the facial nerve is most often of otogenic origin, observed after or during otitis, mastoiditis, eustacheitis. In these cases, reactive inflammation of the nerve trunk develops. Also, the inflammatory process can penetrate directly into the facial nerve itself due to the penetration of infectious agents into it. This is often observed with purulent epidemic partitis, lymphadenitis of the stylomastoid area. Secondary neuritis of the facial nerve can occur with infectious mononucleosis, toxoplasmosis, typhus, tuberculous meningitis, acute leukemia, cranial polyneuritis, polyradiculoneuritis.
Neuritis of the facial nerve occurs with fractures and cracks of the base of the skull passing through the pyramid of the temporal bone (post-traumatic neuritis of the facial nerve). Hereditary factors and congenital developmental anomalies play a major role in the occurrence of paresis of the facial muscles. There are aplasia of the facial nerve trunk and aplasia of the nucleus of the facial nerve. In this case, there may be unilateral and bilateral violations.
The occurrence of neuritis of the facial nerve is facilitated by a narrowing of the fallopian canal and an increase in the size of the styloid process.
Damage to the facial nerve can be one of the signs of such syndromes as Melkersson-Rosenthal syndrome, Mobius syndrome.
No complications
We often hear that nerves do not recover, so when faced with neuritis, many patients believe that their disease cannot be treated. Fortunately, this is not true. The functionality of the nerve after neuritis is restored, but this happens quite slowly. The recovery period can take about a year - and during this time it is important to strictly follow the doctor’s recommendations and not neglect the prescribed treatment. Otherwise, complications may occur.
Article on the topic
A blow to the nerves. Why do neuropathic pain occur?
The most common of these is contraction of the facial muscles, which can distort the face. Muscle atrophy on the side of inflammation may also occur. In this case, the muscles weaken and seem to sag, causing facial paralysis. In addition, the result of untreated neuritis can be twitching of the facial muscles, excessive lacrimation, inability to close the eye, prolonged conjunctivitis or keratitis (inflammation of the cornea of the eye).
To avoid complications, it is necessary to undergo medication and physical therapy. Depending on the causes of inflammation and symptoms, the complex of medications will include anti-inflammatory drugs, antiviral, neurotropic and anticholinesterase agents, B vitamins, diuretics and antispasmodics.
After 7–10 days from the onset of inflammation, physiotherapy is prescribed, which is also selected individually. Phototherapy and laser therapy, electrophoresis, ultraphonophoresis, pulse and decimeter therapy, paraffin and ozokerite applications are successfully used.
An average course of physiotherapy consists of 20 procedures. Sometimes several courses are needed.
Often, for neuritis of the facial nerve, massage is prescribed, but such treatment can be started no earlier than 7 days after the onset of inflammation. It is advisable to massage not only the affected part of the face, but also the neck-collar area. Usually 10–20 massage sessions are needed.
Article on the topic
The root of the problems. How to treat a damaged nerve
If conservative treatment fails within 8–10 months, surgery may be necessary. At the same time, it is impossible to delay surgical intervention - the operation is effective only in the first year of treatment, since later irreversible changes in the muscle tissue on the side of the affected nerve may occur.
Neuritis of the facial nerve diagnosis
Diagnosis of facial nerve neuritis is based on an analysis of the symptoms preceding and accompanying diseases of the nerve damage. Neurologists, neuropathologists, and reflexologists distinguish such forms of damage as neuritis of the facial nerve and neuropathy of the facial nerve. According to pathogenesis, neuritis is divided into primary and secondary.
Neuritis of the facial nerve must be differentiated from isolated damage to the motor nucleus of the nerve, a variety of common pathological processes in the area of the cerebellopontine angle. Damage to the nucleus of the facial nerve is accompanied by isolated paresis of the facial muscles of the same half of the face without autonomic and sensory disorders, which occurs mainly in the pontine form of poliomyelitis or poliomyelitis-like diseases, tick-borne encephalitis.
When the lower parts of the bridge are damaged, which occurs with tumors, encephalitis, vascular diseases, along with the nucleus of the facial nerve, the pyramidal tract is involved in the pathological process. In such cases, peripheral paresis of the facial muscles is combined with central hemiparesis of the opposite side (Millard-Hübler syndrome). If the nucleus of the abducens nerve is affected, then paresis of the external rectus muscle of the eye (Fauville syndrome) is added to the above symptoms.
Isolated neuritis of the facial nerve is differentiated from processes in the area of the cerebellopontine angle, which develop, for example, with arachnoiditis, tumors of the vestibulocochlear nerve, which is manifested by decreased hearing, deafness, paresis of the facial muscles, sometimes dysfunction of the trigeminal nerve, contralateral spastic hemiparesis.
Polyneuritis and polyradiculoneuritis often involve lesions of the facial nerve. Usually the lesion in these cases is bilateral, often asymmetrical, accompanied by limited or diffuse damage to other parts of the human peripheral nervous system.
List of sources
- Alperovich P.M. Bell's palsy (etiology, pathogenesis, clinical picture, course, outcome) / P.M. Alperovich, A.G. Korneychuk, T.I.
- Konstantinovich and others //J. neuropathology and psychiatry named after. S.S. Korsakov. 1978. - T.78, No. 6. -WITH. 836-846.
- Batysheva T.T., Kostenko E.V., Boyko A.N. Complex treatment of facial nerve neuropathy using neuromidin and antioxidant therapy // Journal. psychiatrist, and psychopharmacologist. - 2008. No. 4. - P. 199-201.
- Complex treatment of patients with facial neuropathy and trigeminal neuralgia. Guidelines. - M., 2005. - 32 p.
- Maksimova M. Yu., Sharov M. N., Domashenko M. A. et al. Neuropathy of the facial nerve // Pharmateka. - 2011. - No. 14. - P. 46-51.
- Markin S.P. Neuropathy of the facial nerve // Neurology and Rheumatology. Supplement to the journal Consilium Medicum. - 2010. - No. 1. - P. 10-14.