Facial nerve neuropathy is a disorder in the transmission of nerve impulses along a nerve due to the death of its fibers. Paresis is weakness of the facial muscles , i.e. a consequence of nerve problems. Nervous eye tics are a common reason why patients visit a doctor in search of treatment. Treatment of nervous tic (hyperkinesis) of the eye in our clinic will be based on the cause of hyperkinesis. We specialize in treating neurological problems, including facial nerve treatment.
- Treatment of the facial nerve at the Echinacea clinic
- Restore the functioning of the facial nerve: the sooner, the more completely
- Symptoms of neuritis, neuropathy, inflammation of the facial nerve
- Neuralgia of the facial nerve
- Examination for facial nerve disease - find and eliminate the cause of the disease
- If treatment does not bring results. Synkinesia and facial contracture
- Facial hemispasm. Paraspasm. Blepharospasm
general information
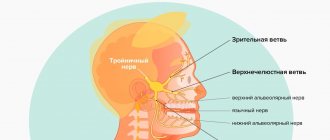
The trigeminal nerve consists of sensory and motor fibers. It originates in the structures of the brain and is divided into three branches:
- ophthalmic: responsible for the eye, forehead and upper eyelid;
- maxillary: innervates the area from the lower eyelid to the upper lip;
- mandibular: involves the chin, lower jaw, lips and gums.
With neuralgia, one or more branches of the trigeminal nerve are affected, which determines the main symptoms of the pathology. People over 45 years of age are most susceptible to the disease, and women get sick more often than men.
Make an appointment
Causes
The causes of trigeminal neuralgia can be of different nature:
- compression of the entire trigeminal nerve or its branches against the background of: enlargement of the arteries or veins of the brain (aneurysms, atherosclerosis, strokes, increased intracranial pressure due to osteochondrosis, congenital developmental features);
- tumors of the brain or facial tissues in close proximity to nerve fibers;
- congenital anomalies of bone structure, narrowed openings through which nerve branches pass;
- injuries of the skull, facial area: bone fractures, post-traumatic scars of soft tissues;
- proliferation of scar tissue after injury, surgery, inflammation;
The risk of developing trigeminal neuralgia increases significantly:
- over the age of 50;
- against the background of mental disorders;
- with regular hypothermia;
- with insufficient intake of nutrients and vitamins into the body (anorexia, bulimia, malabsorption, etc.);
- with regular overwork, stress;
- for helminthic infestations and other helminthiases;
- for acute infections: malaria, syphilis, botulism, etc.;
- for chronic inflammation in the oral cavity (caries, gingivitis, abscesses, etc.);
- against the background of autoimmune lesions;
- with excessive exposure to allergies;
- for metabolic disorders.
Causes
Trigeminal neuropathy can be associated with a variety of conditions. Neuropathy can be caused by blood vessel compression on the trigeminal nerve as it exits the brainstem. This compression causes the protective covering around the nerve (myelin sheath) to wear or become damaged. Symptoms of trigeminal neuropathy can also occur in patients with multiple sclerosis, a disease that damages the myelin sheath of the trigeminal nerve. Rarely, symptoms of neuropathy may be due to nerve compression by a tumor or arteriovenous malformation. Damage to the trigeminal nerve (possibly as a result of oral surgery, stroke, or facial trauma) can also lead to neuropathic pain.
Symptoms
The main characteristic symptom of trigeminal neuralgia is paroxysmal pain. It comes suddenly and in its intensity and speed of spread resembles an electric shock. Typically, intense pain forces the patient to freeze in place, waiting for relief. The attack can last from a few seconds to 2-3 minutes, after which there is a period of calm. The next wave of pain may come within hours, days, weeks or months.
Over time, the duration of each attack of neuralgia increases, and periods of calm are reduced until a continuous aching pain develops.
The provoking factor is irritation of trigger points:
- lips;
- wings of the nose;
- eyebrow area;
- middle part of the chin;
- cheeks;
- area of the external auditory canal;
- oral cavity;
- temporomandibular joint.
A person often provokes an attack when performing hygiene procedures (combing hair, caring for the oral cavity), chewing, laughing, talking, yawning, etc.
Depending on the location of the lesion, the pain takes over:
- the upper half of the head, temple, orbit or nose if the ophthalmic branch of the nerve is affected;
- cheeks, lips, upper jaw – if the maxillary branch is affected;
- chin, lower jaw, as well as the area in front of the ear - with neuralgia of the mandibular branch.
If the lesion affects all three branches or the nerve itself before it is divided, the pain spreads to the entire corresponding half of the face.
Painful sensations are accompanied by other sensory disturbances: numbness, tingling or crawling sensations. Hyperacusis (increased hearing sensitivity) may be observed on the affected side.
Since the trigeminal nerve contains not only sensory, but also motor pathways for the transmission of impulses, with neuralgia the corresponding symptoms are observed:
- twitching of facial muscles;
- spasms of the muscles of the eyelids, masticatory muscles;
The third group of manifestations of neuralgia are trophic disorders. They are associated with a sharp deterioration in blood circulation and lymph outflow. The skin becomes dry, begins to peel, and wrinkles appear. Local graying and even hair loss in the affected area is observed. Not only the scalp suffers, but also the eyebrows and eyelashes. Impaired blood supply to the gums leads to the development of periodontal disease. At the time of the attack, the patient notes lacrimation and drooling, swelling of the facial tissues.
Constant spasms of muscle fibers on the diseased side lead to facial asymmetry: narrowing of the palpebral fissure, drooping of the upper eyelid and eyebrow, upward movement of the corner of the mouth on the healthy side or drooping on the diseased side.
The patient himself gradually becomes nervous and irritable, and often limits himself to food, since chewing can cause another attack.
Symptoms of neuritis, neuropathy, inflammation of the facial nerve
The essence of the symptoms is the disconnection from the brain of those areas whose function is controlled by the facial nerve:
- Weakness or paralysis of the facial muscles of one half of the face, which is expressed in the inability to raise the eyebrows, close the eyes, blink, wrinkle the nose, smile, puff out the cheeks (sail symptom); sometimes you feel the chin being pulled down, tension in the subcutaneous muscle of the neck;
- As a result of the disconnection of the facial muscles, a drooping of the corner of the mouth and smoothness of the nasolabial fold may be noticeable;
- As a result of the shutdown of the cheek muscles, it may be difficult to eat liquid foods;
- Sometimes the symptoms described above are accompanied by dry eyes or lacrimation, increased sensitivity to sounds (booming in the ear), decreased taste sensitivity, increased or decreased sensitivity of the facial skin on the affected side.
Diagnostics
A neurologist diagnoses trigeminal neuralgia. During the first visit, he carefully interviews the patient to find out:
- complaints: nature of pain, its intensity and localization, conditions and frequency of attacks, their duration;
- medical history: when pain attacks first appeared, how they changed over time, etc.;
- life history: the presence of chronic diseases, previous injuries and operations is clarified, special attention is paid to dental diseases and interventions.
A basic examination includes assessing the condition of the skin and muscles, identifying asymmetry and other characteristic signs, checking the quality of reflexes and skin sensitivity.
To confirm the diagnosis, the following is carried out:
- MRI of the brain and spinal cord with or without contrast: allows you to identify tumors, consequences of injuries, vascular disorders; sometimes the study is replaced by computed tomography (CT), but it is not as informative;
- electroneurography: study of the speed of nerve impulse transmission through fibers; allows you to identify the fact of nerve damage, assess the level of the defect and its features;
- electroneuromyography: not only the speed of impulse passage along the nerve bundle is studied, but also the reaction of muscle fibers to it; allows you to assess nerve damage, as well as determine the sensitivity threshold of trigger zones;
- electroencephalography (EEG): assessment of the bioelectrical activity of the brain.
Laboratory diagnostics includes only general studies to exclude other causes of painful attacks, as well as to assess the condition of the body as a whole (usually a general blood and urine test is prescribed, as well as a standard set of biochemical blood tests). If the infectious nature of the disease is suspected, tests are carried out to identify specific pathogens or antibodies to them.
Additionally, consultations with specialized specialists are prescribed: ENT specialist (if there are signs of nasopharynx pathology), a neurosurgeon (if there are signs of a tumor or injury), and a dentist.
Treatment of trigeminal neuralgia
Treatment is aimed at:
- to eliminate the cause of damage;
- to alleviate the patient's condition;
- to stimulate the restoration of nerve structures;
- to reduce the excitability of trigger zones.
Properly selected treatment can reduce the frequency, intensity and duration of pain waves, and ideally achieve stable remission.
Drug treatment
Trigeminal neuralgia requires complex treatment using drugs from several groups:
- anticonvulsants (carbamazepine and analogues): reduce the excitability of nerve fibers;
- muscle relaxants (baclofen, mydocalm): reduce muscle spasms, improve blood circulation, reduce pain;
- B vitamins (neuromultivit, milgamma): stimulate the restoration of nerve fibers, have an antidepressant effect;
- antihistamines (diphenhydramine): enhance the effect of anticonvulsants;
- sedatives and antidepressants (glycine, aminazine): stabilize the patient’s emotional state.
For severe pain, narcotic analgesics may be prescribed. Previously, drug blockades (injecting the problem area with anesthetics) were actively used, but today this method of treatment is almost never used. It contributes to additional damage to nerve fibers.
Treatment of the root cause of the disease is mandatory: elimination of dental problems, taking medications to improve cerebral circulation, etc.
Physiotherapy and other non-drug methods
Non-drug methods complement drug therapy well and help stabilize patients’ condition. Depending on the condition and concomitant diseases, the following may be prescribed:
- ultraviolet irradiation: inhibits the passage of impulses along nerve fibers, providing an analgesic effect;
- laser therapy: reduces pain;
- UHF therapy: improves microcirculation and prevents muscle atrophy;
- electrophoresis with analgesics or antispasmodics to relieve pain and relax muscles;
- diadynamic currents: reduce the conductivity of nerve fibers, significantly increase the intervals between attacks;
- massage of the face, head, cervical-collar area: improves blood circulation and lymph outflow, improving tissue nutrition; must be carried out with caution so as not to touch trigger zones and provoke an attack; the course is carried out only during the period of remission;
- acupuncture: helps relieve pain.
Surgery
The help of surgeons is indispensable when it is necessary to eliminate nerve compression. If indicated, the following is carried out:
- removal of tumors;
- displacement or removal of dilated vessels pressing on the nerve (microvascular decompression);
- expansion of the bone canals in which the branches of the nerve pass.
A number of operations are aimed at reducing nerve fiber conductivity:
- exposure to a gamma knife or cyber knife;
- balloon compression of the trigeminal node: compression of the node using an air-filled balloon installed in close proximity to it, followed by death of the nerve fibers; surgery often leads to partial loss of sensation and decreased muscle movement;
- resection of the trigeminal node: rarely performed due to the complexity and large number of complications.
Make an appointment
Diagnosis and treatment
The main diagnostic methods include:
- CT or MRI (magnetic resonance imaging), which can rule out other causes of pain and identify vascular compression of the trigeminal nerve root;
- radiography of the paranasal sinuses to identify chronic inflammatory and other pathological processes;
- consultation with a neurologist;
- OPTG (orthopantomogram), to assess the width of the bone canals;
- dentist consultation;
- general blood analysis.
Treatment of neuralgia includes the following main methods:
- medicinal;
- surgical treatment.
Drug therapy is selected individually for each patient, depending on the severity of the pathology. Surgical treatment is recommended in the absence of clinical effect from drug therapy.
Complications
Without treatment, trigeminal neuralgia gradually progresses. Over time, a pathological pain focus forms in one of the parts of the brain. As a result, the pain covers the entire face, is provoked by any minor irritant and even the memory of an attack, and subsequently becomes permanent. Vegetative-trophic disorders progress:
- irreversible atrophy of the facial muscles is formed;
- teeth become loose and begin to fall out due to advanced periodontal disease;
- baldness is increasing.
Due to constant pain, the patient's sleep is disturbed and severe depression develops. In severe cases, patients may commit suicide.
Clinical manifestations of neuralgia
The following symptoms are characteristic of trigeminal neuralgia:
- attacks of severe pain;
- increased pain during any actions with the mouth (chewing, opening, etc.);
- facial distortion;
- concentration of pain in the eyes, ears, teeth, mouth;
- teak.
Trigeminal facial neuralgia is characterized by attacks of stabbing, cutting, pulling pain lasting up to 1 minute. In the vast majority of cases, one side of the face is affected, but there are cases when pathological processes spread to the entire face. Painful sensations can be projected into the teeth and can cause the removal of a completely healthy tooth.
Prevention
Prevention of trigeminal neuralgia is a set of simple measures that significantly reduce the risk of developing pathology. Doctors recommend:
- undergo regular preventive examinations;
- at the first signs of the disease, seek help (the sooner treatment is started, the greater its effect will be);
- eat right, get the required amount of vitamins, minerals, unsaturated fatty acids;
- regularly engage in light sports and gymnastics;
- get enough sleep and rest;
- minimize stress and physical overload;
- avoid hypothermia and harden yourself;
- to refuse from bad habits.
Treatment at the Energy of Health clinic
If you or your relative are bothered by severe pain in one or another part of the face, the neurologists of the Health Energy clinic will come to the rescue. We will conduct a full diagnosis to identify the causes of the pathology and prescribe comprehensive treatment. At your service:
- modern drug regimens to reduce the frequency and intensity of attacks;
- physiotherapeutic procedures: magnetotherapy, laser therapy, electrophoresis, phonophoresis, etc.;
- delicate therapeutic massage;
- acupuncture;
- help from a psychologist if necessary.
Neuralgia of the facial nerve
Neuralgia is a pain syndrome. The diagnosis of “facial neuralgia” is usually made incorrectly instead of the diagnosis of “trigeminal neuralgia”. The facial nerve contains only motor nerve fibers and does not transmit sensory impulses. Therefore, neuralgia, i.e. There is no pain in the facial nerve system. The facial nerve transmits commands from the brain to the facial muscles, and the symptoms of its suffering are weakness or paralysis of the facial muscles (facial nerve paresis).
Read more about trigeminal neuralgia
Advantages of the Health Energy Clinic
The Health Energy Clinic is a multidisciplinary medical center where every patient has access to:
- screening diagnostic programs aimed at early detection of diseases and pathologies;
- targeted diagnostics using modern equipment and laboratory tests;
- consultations with experienced specialists, including foreign ones;
- modern and effective comprehensive treatment;
- necessary certificates and extracts;
- documents and appointments for spa treatment.
Trigeminal neuralgia is a serious pathology that can seriously disrupt a person’s normal lifestyle. Don't let pain and fear take over your thoughts, get treatment at Health Energy.