Inflammation of the facial nerve is an unpleasant ailment that does not go away painlessly. The main complaints of patients are sharp attacks of pain in the face, in the upper and lower jaws.
This inflammation is considered one of the most common among facial pains. Most often, the disease proceeds without a trace, but if treatment is neglected, paralysis may occur.
The disease most often occurs in women over 50 years of age; men are treated with this disease much less frequently. People with a genetic predisposition, such as a narrow bone canal, are also at risk. Due to this anatomical feature, there is an increased risk of pinching due to impaired blood supply and various inflammations.
What is the facial nerve?
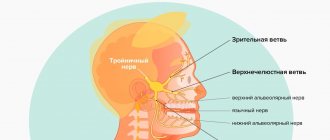
The trigeminal nerve, also known as the facial nerve, is the largest of the twelve cranial nerves. It originates in the ear, after which it branches, the first path reaches the frontal part, the second is located at the jaw. The nerve goes around almost the entire surface of the human face; it literally controls it.
Every person has two facial nerves - one on each side of the head. It is in contact with other cranial nerves and has supersensitive fibers.
Doctors divide the disease into two types - primary and secondary. The primary one manifests itself as a complication from a cold, in this case the normal nutrition of the nerve is disrupted. Secondary occurs with severe intoxication against the background of inflammatory or infectious diseases, as well as tumor processes.
Home remedies
Before treating trigeminal neuralgia at home, you should consult a doctor, since many remedies can only worsen the situation. If the specialist allows it, it is also possible to use various home recipes.
According to recommendations for trigeminal neuralgia, it is worth consuming orally or lubricating the affected side with birch sap. You need to drink 4-5 glasses per day. Heated buckwheat folded in cotton cloth will help relieve pain. The compress is made 2 times a day, keeping it at the site of inflammation until it cools down. At home, it is useful to massage the sore area: rub, stroke and lightly knead the area of inflammation.
Causes of inflammation of the trigeminal nerve on the face
Usually the disease is caused by infection or bacteria. List of reasons why inflammation of the facial nerve may occur:
- Temporomandibular joint injuries
- Tumors (benign and malignant) of the brain and facial area
- Anomalies of skull development
- Skull injuries - birth, fracture, base, damage to the face or jaw
- Polio
- Pulmonary tuberculosis
- Otitis
- Sinusitis
- Chronic caries
- Inflammation after tooth extraction or treatment
- Hypertension
- HIV and AIDS
- Poisoning
- Inflammation of the middle ear
- Severe hypothermia of the head
- Changes in hormonal levels in women
- Gum inflammation
- Ramsay Hunt syndrome
- Stroke
- Bell's palsy
Causes range from minor to life-threatening illnesses. Each of the reasons determines the further treatment of the patient. In some cases, special tests are performed for diagnosis - auditory, lacrimal, infectious, salivary or gustatory. In this way, the functioning of the receptors and sensory organs is checked.
Symptoms of inflammation of the trigeminal nerve
Experts include short-term, but acute and intense pain in different parts of the head as the main symptoms of facial neuralgia. Shooting attacks spread over the entire surface of the face - lips, eyes, nose, upper and lower jaw, gums and tongue.
Patients also report the following symptoms:
- Metallic taste in the mouth
- Muscle weakness
- 2-3 days before facial expressions are affected, pain occurs behind the outer ear, spreading to the face, back of the head and eyes
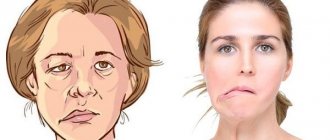
- Facial asymmetry
- Inability to close the eye on the affected side
- Drooping corner of the mouth
- Dry mouth
- Slurred speech
- Cross-eyed strabismus
- Uncontrollable tearing
- Disorders of taste buds
- Increased drooling
- Facial muscle spasms
- Increased or decreased facial sensitivity
- Temperature increase
Due to discomfort and pain, the patient begins to develop a phobia and increased anxiety. He tries to avoid poses and movements that provoke discomfort.
Diagnosis of inflammation of the trigeminal nerve
Depending on the affected area and the set of symptoms, the strategy for diagnosing the disease is determined. To determine the location of nerve damage, the severity and dynamics of recovery, doctors prescribe a hardware diagnostic method, for example, electromyography. MRI and CT scans are used to determine the presence of tumors in the brain.
The patient may also be referred for a general or biochemical blood test, x-ray of the lungs, ultrasound of soft tissues or ophthalmoscopy.
You can be confident in the quality of the procedures performed in the clinic and the high accuracy of the results of MRI, CT and other methods of diagnosing various diseases. Medunion performs magnetic resonance imaging of all types: head, spine, abdominal cavity and joints using modern equipment.
Treatment
Treatment of inflammation of the trigeminal nerve is carried out depending on the severity of symptoms. First, conservative therapy is prescribed. If this does not help, doctors resort to surgical methods. Their essence is to eliminate the cause of neuralgia. This may be compression of the nerve by the vessel. Surgical treatment is carried out using radiofrequency destruction, microvascular decompression or percutaneous surgery.
What drugs are most effective for the treatment of trigeminal neuralgia:
- antibiotics. Prescribed for infectious nature of the disease;
- glucocorticosteroids. Relieves severe inflammation in the body;
- non-steroidal anti-inflammatory drugs (NSAIDs). Helps suppress inflammatory processes;
- painkillers. Relieves soreness in the facial muscles;
- muscle relaxants.
To improve metabolic processes in the nervous tissue, the patient is prescribed B vitamins. How to relieve acute pain with trigeminal neuralgia:
- use anticonvulsants;
- provide physical rest, preferably bed rest;
- Apply an anti-inflammatory ointment or a warm compress to the site of pain.
Treatment for inflammation of the facial nerve
Drug treatment
Treatment of trigeminal neuritis is complex. The disease is first treated with medication - the patient is prescribed drugs that will alleviate the situation. These include painkillers, decongestants, vasodilators and B vitamins. Most often, the recommended medications are tablets, but you can speed up the recovery process by using ointments and gels. Sometimes doctors prescribe intramuscular injections.
In special cases, the recovery process of the facial nerve may be slowed down. Then the patient is prescribed glucocorticosteroids, which improve the metabolic processes of nervous tissue. Various biostimulants and hyaluronidases also contribute to a speedy recovery.
You cannot prescribe medications for yourself. Be sure to see a neurologist or neuropathologist at the first symptoms to determine the diagnosis and treatment strategy. Recovery medications are recommended to patients on a case-by-case basis, paying attention to the presence of chronic diseases, symptoms, and so on.
Surgery
Another way to treat the facial nerve is surgery. However, doctors turn to this option quite rarely - only when the trigeminal nerve is ruptured. Surgery is also required if there is no effect from the conservative method after six months or a year. Surgical intervention is only relevant during the first year of the presence of the disease; later, the muscles on the face irreversibly atrophy.
The surgical process involves suturing the damaged area of the facial nerve to restore its motor function.
Massage
The next treatment method is massage for the treatment of the facial nerve. The purpose of this method is to remove swelling, improve blood circulation, restore sensitivity and conduction of nerve impulses. Massage is contraindicated for tuberculosis, oncology, atherosclerosis and elevated temperature.
Initially, the massage therapist works only with the healthy side of the face, collar area, neck and area above the shoulders. Basically, the master uses rubbing, stroking, kneading and vibration.
For noticeable desired changes, it is necessary to conduct ten to twenty massage sessions from five to fifteen minutes. The duration is determined based on the degree of inflammation of the trigeminal nerve, the goals of therapy and the dynamics of recovery.
Physiotherapy
The next treatment method is physical therapy. It alleviates the severity of symptoms, helps to activate metabolic processes in tissues and restore the functions of the facial nerve.
Doctors prescribe this course of treatment from the first days of the onset of neuritis. The list of physical procedures includes:
- Ultrasound
- Laser irradiation of blood
- Electrophoresis of drugs
- Microwave therapy
- Exposure to ultra-high frequency electricity
- Ozocerite treatment
- Myoelectrostimulation
- Darsonvalization
This complex is indicated for the first week of treatment. Doctors prescribe it together with medication. This tandem helps speed up the process of restoration of the facial nerve. And its most important advantages are the absence of side effects and painlessness.
Alternative Methods
There are also alternative treatment methods. These are procedures aimed at restoring facial muscles and eliminating the symptoms of facial neuritis. Such procedures include:
- Clay or paraffin masks
- Acupuncture
- Reflexology
- Injections to eliminate muscle disorders
- Therapeutic baths
- Taping – stretching the face using adhesive plasters
- Immunosorption – purification of blood from antigens and antibodies
- Biofeedback – facial muscle training
Gymnastics for the face
Also, in conjunction with complex treatment, you can do facial exercises. Before this, you need to consult with a specialist; the doctor will draw up an individual list of exercises based on the severity of the process, location of the lesion and symptoms. Typically, such gymnastics takes about ten minutes a day.
A standard set of exercises includes relaxing and tensing individual facial muscles. For example, to restore articulation, it is recommended to pronounce the sounds “u”, “o”, “and”. Afterwards, you need to bring your lower lip under your upper teeth and reproduce the sounds “v” and “a”.
Gymnastics for inflammation of the trigeminal nerve:
- Close eyes
- Raise your eyebrows
- Frown
- Squint
- Smile with your mouth closed
- Smile with your mouth open
- Puff up your cheeks
- Pull them back
- Whistle
- Widen your nostrils
- Curl your lips
- Raise your upper lip and return to the starting position
- Lower your lower lip and return to the starting position
- Take water into your mouth
- Rinse your mouth
- Close your mouth
- Run the tip of your tongue along your gums
- Move your tongue right and left
- Surgery
- Oncology
- Neurosurgery
- Radiology and Radiation Therapy
- Gynecology and new reproductive technologies
- Traumatology and Orthopedics
- Cardiology
- Neurology
- Laser surgery
- Urology, andrology and microsurgery
- Plastic surgery
- Mammalogy
- Lithotripsy
- Psychological support service
- ECO
- Weight loss
- Pressure chamber
- Endovascular surgery
- Pituitary adenomas
- Arnold-Chiari malformation and syringomyelia
- Parkinson's disease
- Hydrocephalus
- Hemifacial spasm
- Herniated discs
- Violent movements
- Brain tumors
- Vascular diseases of the brain
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Essential tremor
The trigeminal nerve (V pair of cranial nerves) contains sensory, motor and autonomic fibers (Fig. 1). The nuclei of the trigeminal nerve are located in the brain stem, at the exit from which the fibers that make up the large root reach the top of the pyramid of the temporal bone, where the trigeminal ganglion (Gasserian ganglion) lies, from which 3 branches extend: the orbital (sensory) nerve leaves the skull through the superior orbital gap, innervates the upper eyelid, conjunctiva of the eye, skin of the forehead and scalp in front; the maxillary (sensitive) nerve leaves the skull through the round foramen, penetrates the pterygopalatine fossa, innervates the skin of the lower eyelid, cheeks and nose, mucous membrane of the nasal cavity, upper jaw, etc.; The mandibular nerve (the small root of the trigeminal nerve, containing motor fibers, joins it) leaves the skull through the foramen ovale, innervates the skin of the lower part of the face, the mucous membrane of the cheeks, tongue, lower jaw, masticatory muscles, etc. The trigeminal nerve takes part in many reflexes ( corneal, mandibular, etc.). Fig. 1 Anatomy of the trigeminal nerve and its branches. Trigeminal neuralgia is a disease accompanied by paroxysmal intense unilateral facial pain in the area of the chin, lips, gums, cheeks, eyes, lasting several seconds or minutes. As a rule, middle-aged and elderly people suffer. A characteristic feature is the ability to cause pain by touching a specific area of the face or mouth.
Clinic and diagnostics.
The first attack of pain seems subjectively so pronounced and unexpected that, as a rule, patients well remember all the circumstances of the initial paroxysm even after many years. Sometimes the disease begins gradually with a slight unpleasant feeling of twitching, “electrification” in a certain area of the face, or with a toothache, which forces you to seek help from a dentist. Only the characteristic paroxysmal pain that subsequently appears allows a correct clinical diagnosis to be made and appropriate examination and treatment to be carried out. Trigger zones for the development of an attack (trigger zones) with trigeminal neuralgia are localized close to the midline, covering the lips, wings of the nose, eyebrows and chin, in rare cases located in the external auditory canal. Localization of trigger zones on the gums, tongue and palate makes it impossible to eat, talk, and perform basic hygiene requirements. Some patients with a similar arrangement of the trigger zones and severe pain lose weight, become weak and fall into a depressive state, sometimes leading to suicide attempts. The attacks recur day and night for several weeks, and then often subside. After some time, the disease appears again, and after a few years the attacks become permanent. The diagnosis of trigeminal neuralgia is confirmed by relief of pain when taking carbamazepine drugs (finlepsin, tegretol). After several years of taking carbamazepine, the effectiveness of the previous dosage usually decreases and there is a need to increase the dose of medication. Some patients cannot tolerate this drug due to side effects such as drowsiness, dizziness and staggering when walking, pain in the liver, suppression of white blood cells (leukopenia). The cause of such facial pain in most cases is compression of the trigeminal nerve root by an arterial vessel at the level of the posterior cranial fossa. Less commonly, trigeminal neuralgia can be caused by brain tumors or multiple sclerosis. Trigeminal neuralgia in multiple sclerosis, tens of times lower in frequency than typical trigeminal neuralgia, occurs as a result of demyelination of trigeminal sensory structures, mainly the entrance zone of the sensory root and the descending tract of the trigeminal nerve. It is likely that the subsequent replacement of foci of demyelination by glial cells, causing an increase in the excitability of neighboring sensory fibers, also contributes to the persistence of the pain syndrome. In addition, the development of trigeminal neuralgia in patients with multiple sclerosis may be due to vascular compression of the trigeminal sensory root. Trigeminal neuralgia in brain tumors can occur with tumors of the posterior and middle cranial fossa, pituitary tumors, epidermoids in the case where tumor growth leads to direct compression of the trigeminal nerve root or changes the spatial relationship of vessels and nerves in such a way that one of the vessels leads to compression of the trigeminal nerve root (Fig. 2). Fig. 2 Trigeminal neuralgia with epidermoid tumor. Intraoperative photography. 1 – tumor. 2 – trigeminal nerve root. To exclude a brain tumor, vascular pathology, or multiple sclerosis, all patients undergo magnetic resonance imaging (MRI) of the brain. Often in such photographs you can see the “culprit” vessel compressing the trigeminal nerve root.
Treatment.
The diagnosis of neuralgia is confirmed by relief of pain when taking carbamazepine drugs (finlepsin, tegretol). After several years of taking carbamazepine, the effectiveness of the previous dosage usually decreases and there is a need to increase the dose of medication. Some patients cannot tolerate this drug due to side effects such as drowsiness, dizziness and staggering when walking, pain in the liver area. Surgical treatment is indicated for patients who cannot tolerate carbamazepine drugs or when their effectiveness decreases. Our center is a leading institution in Russia performing all types of surgical interventions for trigeminal neuralgia with more than 20 years of experience in the diagnosis and treatment of this disease. A method of treating pathology that has proven to be highly effective is percutaneous radiofrequency trigeminal rhizotomy, an operation that involves partial destruction of the trigeminal nerve root under local anesthesia. The procedure is carried out as follows: a) a thin needle is passed through the face to the base of the skull under X-ray control (Fig. 3). Fig. 3 Percutaneous high-frequency trigeminal rhizotomy in a patient with trigeminal neuralgia of the I-II branches. Intraoperative radiography (lateral projection), confirming the correct position of the curved electrode b) stimulation of the root is carried out, which is accompanied by a pain attack in the “sick” area of the face. This stage of surgery is the most unpleasant for patients. c) partial destruction of the root is carried out due to setting an increased temperature at the tip of the needle until sensitivity in the desired area of the face decreases. Such an operation may be preferable for elderly people, those who are afraid of open surgery, and those with multiple sclerosis. In most patients, after a few years (on average 5–7 years), the numbness in the face disappears, and facial pain reappears. A more physiological operation that does not lead to numbness in the area of innervation of the trigeminal nerve is the operation of vascular decompression of the facial nerve root (Microvascular decompression). This is a microsurgical operation performed under general anesthesia, in which, after performing a small trepanation behind the ear on the side of pain, the vessel is diverted from the trigeminal nerve root in the posterior cranial fossa (Fig. 4 and 5). The effectiveness of this technique is more than 90% if patients are correctly selected for surgery. Fig. 4 Intraoperative photo of a patient with trigeminal neuralgia. The arrow indicates compression of the input zone of the trigeminal nerve root by the loops of the superior cerebellar artery (V - trigeminal nerve, SMA - 2 branches of the superior cerebellar artery, CV - petrosal vein) Fig. 5 Intraoperative photo: decompression of the input zone of the trigeminal nerve root at the brain stem was performed (V - trigeminal nerve, SMA - loop of the superior cerebellar artery, M - fragment of muscle tissue) The recovery process after microvascular decompression surgery rarely takes more than a week, after which patients are discharged home and forget about their disease forever.
Disease prevention
Doctors recommend eliminating effects on the body that cause inflammation of the trigeminal nerve. Here are some recommendations to help avoid illness:
- Avoid drafts and hypothermia
- Keep your head warm during the cold season
- Monitor your blood pressure
- Timely treatment of infectious and bacterial diseases
- Have a routine check-up with an oncologist
- Avoid skull and head injuries
You can sign up for an individual consultation, take tests or undergo treatment at the Medunion private clinic. You can easily make an appointment with us by calling 202-95-54 or online, directly on the website, by clicking on the “Online booking” button.
We have been working in Krasnoyarsk since 2006 and provide high-quality medical services to the population. The staff consists of highly qualified doctors of broad and narrow specialization.
Possible complications
Over time, symptoms of inflammation of the trigeminal nerve can give rise to neuropathic complications and lead to the development of secondary pain syndrome in the head. In the chronic form of the disease, the auditory and facial nerves are irritated. Without treatment, trigeminal neuralgia can lead to more serious complications:
- dystrophy of masticatory muscles;
- decreased sensitivity of the affected area;
- Sykinesia (cooperative movements in which one nerve controls many muscles);
- contracture and spontaneous contraction of the facial muscles;
- conjunctivitis.