Fasting ketoacidosis: what you need to know
Fasting ketoacidosis occurs when a person has undergone an extended period of fasting.
During fasting ketoacidosis, fatty acids replace glucose as the body's primary source of fuel. Fasting ketoacidosis is rare, but some are at higher risk of developing it than others. A high-risk group includes patients with eating disorders.
Fasting ketoacidosis can be a serious condition if left untreated and can even lead to death.
This article discusses fasting ketoacidosis in more detail, including its symptoms, as well as how to treat and prevent it.
Side Effects, Misconceptions, and Potential Dangers of Ketosis
Side effects are usually observed in the first days of the keto diet and include: headaches, weakness, dizziness, irritability, cramps and constipation. This set of symptoms is sometimes called the “keto flu.” Their manifestation can be weakened by drinking plenty of fluids and electrolytes.
Is ketosis safe for anyone?
The state of ketosis is not only safe for the vast majority of people, but also has undeniable positive effects. First of all, this means losing weight, normalizing blood sugar and insulin levels, improving performance and concentration.
But, there is a category of people who should be under the supervision of a doctor during the keto diet or those for whom it is completely contraindicated. People with the following diseases and conditions require medical supervision during the keto diet:
- type 1 diabetes mellitus;
- diabetes mellitus type 2 (while taking insulin and other medications);
- hypertension (high blood pressure) and taking anti-hypertensive medications;
- some heart, liver and kidney diseases;
- patients who have undergone operations on the gastrointestinal tract (primarily on the stomach);
- pregnant women.
The following categories of people should avoid the keto diet for medical reasons:
- women during breastfeeding;
- patients with rare congenital diseases that appear from childhood (for example, a lack of enzymes that prevent the production and metabolism of ketones in the body).
“This article was translated into Russian from a foreign source, Diet Doctor, the world's largest site dedicated to low-carb diets.”
What is fasting ketoacidosis?
Ketoacidosis is a metabolic condition associated with high levels of ketones in the blood. Ketones accumulate when the body breaks down fatty acids to use them for energy instead of carbohydrates.
Fasting ketoacidosis occurs when the body does not receive enough glucose as a primary source of energy for an extended period.
There are various reasons why a person may fast for long periods of time, including:
- economic forces
- eating disorders
- difficulty swallowing
- cancer
Mild ketosis—meaning the body uses fat as an energy source—can occur after 12 to 14 hours of fasting.
Ketoacidosis occurs when the buildup of ketones causes the blood to become acidic. In fasting ketoacidosis, when the body runs out of fat, it begins to break down muscle, causing amino acids and lactate to leak into the blood. The liver then breaks them down into sugar, which is used as fuel.
The transition from ketosis to ketoacidosis can occur after 2-3 days of fasting. After another couple of days, muscle breakdown may begin.
Reason One: You're Not in Ketosis
“There is a threshold at which the body switches into ketosis and begins to use fats. And it is individual,” explains Olga Bezuglaya, Ph.D., keto diet specialist, bariatric nutritionist. Perhaps there are hidden sugars in the diet and it needs to be reviewed . Although even on a low-carbohydrate diet, when there is no ketosis, you can already feel the positive effects - due to cutting carbohydrates. But many people won’t feel the effects because they think they’ve cut carbs enough to be in ketosis, but they haven’t.”
Starvation ketoacidosis: other types
According to a 2021 article, there are three types of ketoacidosis:
- diabetic ketoacidosis
- alcoholic ketoacidosis
- ketoacidosis from fasting
Diabetic ketoacidosis
Diabetic ketoacidosis occurs when the body runs out of insulin, which can be life-threatening.
Diabetic ketoacidosis can occur in people with diabetes or type 1 diabetes, but it is more likely to affect people with type 1 diabetes.
Alcoholic ketoacidosis
According to a 2021 review, alcoholic ketoacidosis most often affects those who drink excessive amounts of alcohol and find that the resulting symptoms, such as nausea, anxiety and abdominal pain, prevent them from eating solid food for 1-3 days.
Alcoholic ketoacidosis occurs when the body is unable to use glucose from its diet.
The alcohol in their blood lowers their blood sugar and prevents the liver from producing glucose.
Reason two: keto adaptation is not complete
Elena Rybatskaya , one of the founders of the largest Facebook community in Russian dedicated to the keto diet, believes that the reason is in a hurry. “They rush to start without getting acquainted with the details, and get information about this nutrition from low-quality sources. They don’t wait quietly for adaptation to take place; for some it takes several months.
That is, they don’t know nutrition well, make mistakes and don’t give themselves time to calmly enter ketosis and let the body get used to it. The athletes are in a hurry - they can’t wait to adapt, they can’t reduce the load for the first six months.”
Olga Bezuglaya confirms: “People achieve metabolic flexibility at different times, the adaptation process takes place individually and for some it takes a lot of time.”
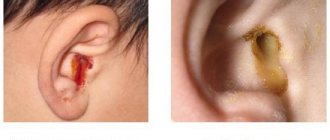
Symptoms and warning signs
Signs and symptoms of fasting ketoacidosis may include:
- decrease in muscle mass
- decrease in body temperature
- minimal amount of body fat
- low heart rate
- obvious thinness
- caries
- sparse, thin, dry hair
- low blood pressure
The 2021 case report provides information on patients with mental disorders and starvation ketoacidosis. The authors conclude that making an accurate diagnosis may be more challenging for people with mental disorders because they may be unable to provide an accurate history of their health or eating habits. As a result, there may be a delay in treatment.
Reason five: excessive energy consumption
In modern society, workaholism is a socially approved addiction. We undermine our health at work, we come to the keto diet to restore lost resources in order to spend them again at work. “Energy rises, and instead of enjoying it, people start working harder like crazy, or torturing themselves with sports in pursuit of super results ,” states Elena Rybatskaya.
And Yulia Kiltina notes that having received the energy of ketosis, we often forget about “alternative sources”: “In ketosis, you usually get better sleep and in a little less time, but this does not mean that you should neglect your daily routine. Lack of sleep is a common reason why even on a keto diet you don’t feel better.”
Risk factors
With easy access to food, the risk of developing fasting ketoacidosis is reduced.
However, intermittent fasting, especially when combined with an extreme diet such as a ketogenic diet, may put you at a higher risk of developing ketoacidosis. If you are interested in following specialized diets such as the keto diet, you should talk to your doctor before starting the diet.
And the 2021 article lists the following risk factors for developing ketoacidosis during fasting:
- difficulty swallowing, including after surgery or radiation therapy
- presence of underlying conditions or diseases that interfere with normal nutrition
- long periods of time without adequate nutrition
Ketosis and ketoacidosis. Pathobiochemical and clinical aspect
About the article
17411
0
Regular issues of "RMZh" No. 23 dated December 2, 2004 p. 1301
Category: Dermatology
Author: Lukyanchikov V.S.
For quotation:
Lukyanchikov V.S. Ketosis and ketoacidosis. Pathobiochemical and clinical aspect. RMJ. 2004;23:1301.
Overweight and obesity represent one of the most pressing medical and social problems of our time. These are the most significant risk factors, or rather the cause of cardiovascular pathology, diabetes mellitus and a number of other diseases and syndromes. The severity of this problem is growing everywhere due to the general trend towards aging of the population, and in many countries also due to the low standard of living, which, as is known, negatively affects the nutritional structure and contributes to obesity. From the point of view of the main medical requirements - safety and effectiveness - the most acceptable method of combating obesity is food restriction. In this regard, the best results are obtained by a low-calorie protein-saving diet with an energy value of about 800 kcal per day and a protein content of at least 50 g [2,8]. However, some researchers view the connection of such diets with certain undesirable and even dangerous consequences, such as hypoglycemia, hyperuricemia, hyperlipidemia, cardiac arrhythmia, cholelithiasis, osteoporosis, etc. [3,5,9,11]. Among these consequences, perhaps the greatest concern for doctors and patients is ketosis (apparently in association with diabetic ketoacidotic coma). Definition, biochemistry and pathobiochemistry of ketosis Ketone bodies are a group of organic compounds that are intermediate products of energy metabolism, i.e. metabolism of fats, proteins and carbohydrates. The term ketone bodies refers to three compounds: acetoacetic acid (acetoacetate). ? –hydroxybutyric acid (? –hydroxybutyrate) and acetone [1]. The formation of ketone bodies, or ketogenesis, is a physiological process, in other words, an essential part of energy metabolism. During this exchange, “combustion” and intertransformation of carbohydrates, fats, proteins and other energy substrates occurs with the formation of energy, which is either converted into heat in order to maintain optimal body temperature, or is accumulated in the form of AMP, ADP and ATP. These compounds, acting as energy batteries, have a low capacity, since they are located inside cells, and are also continuously consumed to ensure cellular life. Moreover, the synthesis of these energy carriers requires more energy than what is stored in them. Therefore, the real energy reserves of the body are glycogen, adipose tissue and protein structures. Biological expediency places glycogen last in the ranking of reserve energy substrates. Firstly, because in the body glycogen has no other functions other than energy. Secondly, glycogen is difficult to stabilize, i.e. stored in living tissue, and storage requires a large amount of water, which greatly reduces the energy content of glycogen, which is already lower than that of protein and fat. Obviously, for these reasons, a person’s glycogen reserves are small, amounting to approximately 500–700 g. The energy equivalent of these reserves is 2–3 thousand kcal, which does not even cover a person’s daily energy needs. Body proteins have the greatest energy potential. In an adult, their total mass reaches 35–40 kg, which is equivalent to 150–170 thousand kcal. But for obvious reasons, using your own proteins as an energy source is extremely undesirable. As a result, the most optimal way to maintain energy reserves is the synthesis and deposition of fat. Apparently, this is the main reason for people’s tendency to obesity and its high prevalence. The amount of adipose tissue in an adult is a very variable and highly individual characteristic. According to rough estimates, the mass of adipose tissue in a person of average fatness is 15–18 kg. Taking into account the high energy content (9 kcal per 1 g), the total energy value of this amount of fat is practically not inferior to the energy content of body proteins. At the same time, adipose tissue performs many other important functions in the body: synthesis and metabolism of hormones and bioactive substances, heat production, insulation and preservation of heat, giving elasticity to soft tissues, fixation of organs, and much more. Thus, a person has good reason to care about maintaining fat reserves. And it is no coincidence that the system for regulating energy metabolism is more focused on creating fat reserves than on wasting them. This priority is the second significant reason for the high incidence of obesity and why obesity is so difficult to combat. A schematic diagram of energy metabolism, including the formation of ketone bodies, is presented in Figure 1. The main regulators of energy exchange are given in Table 1. Analyzing the diagram and table, two key points should be highlighted. Firstly, energy metabolism is conventionally divided into the anabolic phase (synthesis of fat and glycogen) and the catabolic phase (glycolysis - oxidation of fatty acids, mobilization and deamination of amino acids). In this case, the main stimulator of the anabolic part of metabolism is insulin, while catabolic processes are enhanced by numerous counter-insular hormones. Secondly, acetyl-CoA is a key substrate for energy metabolism and at the same time the starting substance for the synthesis of keto acids. It is the content of acetyl-CoA that determines the direction of cellular metabolism at a given moment, namely, whether the synthesis and accumulation of glycogen, fat and protein synthesis will occur or, on the contrary, previously accumulated energy reserves will be consumed. And this, first of all, depends on the amount of food entering the body. If there is a lot of food and its quantity exceeds current energy expenditure, part of the food energy is converted mainly into fat, since glycogen reserves, as already noted, are small, and this “pantry” quickly fills up. If there is little or no food, the body makes up for the deficiency by using previously made reserves - first glycogen, then fat. It is known that some tissues and organs, in particular the renal cortex, red blood cells and, most importantly, the brain, use only carbohydrates (more precisely, glucose) as an energy source. This requires about 200 g of glucose per day, which the body obtains by breaking down glycogen. True, with the breakdown of 100 g of adipose tissue, about 10 g of glycerol is also released, but this is too little. As a result, lipolysis and ? – oxidation of fat breakdown products, which are the main source of energy in conditions of food shortage, is not able to provide energy to a number of the most important structures of the body. There are two alternative ways to solve this problem. Firstly, gluconeogenesis, i.e. endogenous glycogen synthesis. Secondly, the synthesis of keto acids, which are successfully absorbed by the brain and other tissues with limited metabolic capabilities and thereby serve as a replacement for glucose. Let us recall that keto acids are a product of the metabolism of acetyl-CoA, which, in the event of food deficiency, is formed either from its own proteins or from fat. Of the two named endogenous sources of energy supply to the brain, ketogenesis is preferable. The fact is that gluconeogenesis requires the amino acid alanine, which, in conditions of food deficiency, the body receives only through the destruction of its own proteins, carried out by glucocorticoid hormones of the adrenal glands (Table 1). Therefore, it is quite natural, or more correctly, in accordance with the law of biological expediency, energy exchange during food deficiency is accompanied by increased formation of keto acids and an increase in their concentration in the blood, i.e. ketosis. It should be noted that these metabolic events are not only expedient, but even preferable for the body, and at the same time rationally organized. Accumulating in the blood, keto acids suppress the secretion and specific activity of glucocorticoids [10], thereby preventing proteolysis, i.e. destruction of structural proteins of the body. Along with this, ketosis inhibits the secretion and action of glucagon [1,6], the main stimulator of gluconeogenesis and ketogenesis. Thus, by inhibiting proteolysis and gluconeogenesis, keto acids preserve the structural proteins of the body, and by suppressing glucagon, they prevent excessive formation and dangerous accumulation of ketone bodies in the blood. Unfortunately, the intensity of ketogenesis and the rate of absorption of keto acids by tissues are extremely variable, individual values that cannot be predicted or quantified. What further complicates the assessment of ketosis is that the main of the three keto acids, namely ? –hydroxybutyrate, is synthesized both from acetoacetate and directly from acetyl-CoA (Fig. 1). Meanwhile, the nitroprusside method used in the clinic for determining keto acids detects only acetoacetate, and when its concentration reaches 2.5–3 mmol/l. Obviously, therefore, there are no clear laboratory criteria for the upper limit of the normal content of keto acids in the blood, i.e. physiological ketosis, which is a compensatory-adaptive reaction designed to eliminate the lack of glucose necessary to nourish the brain. For the same reason, in clinical practice the terms ketosis and ketoacidosis are often equated, which, of course, is incorrect. Acidosis, including ketoacidosis, is a uniquely pathological condition, namely a form of disturbance of the acid-base state of the body, when the ratio between acid anions and base cations shifts towards an increase in anions [7]. By definition, acidosis is a laboratory term. Its laboratory criteria are a blood pH below 7.35 and a standard serum bicarbonate concentration of less than 21 mmol/L. To verify metabolic acidosis, which includes ketoacidosis, the anion difference indicator is used [1,7]. Normally, the anion difference of blood serum does not exceed 14 mmol/l, and with ketoacidosis it increases to 15–20 mmol/l. Thus, enhanced ketogenesis and moderate ketosis, which accompany prolonged fasting or chronic malnutrition, initially do not represent a pathological disorder of energy metabolism, but a compensatory-adaptive reaction. At the same time, it must be admitted that in clinical practice there are many cases where overly expressed compensatory reactions acquire a completely pathological character, turning into so-called adaptation diseases. In relation to the problem under discussion, this possibility is discussed below. Clinical forms of ketosis and ketoacidosis Taking into account the compensatory-adaptive role of ketogenesis, obviously, there are many clinical situations that can be accompanied by the development of ketosis and ketoacidosis. The most common of them, in other words, the etiological classification of ketosis and ketoacidosis with an assessment of the probability of transition from ketosis to ketoacidosis is presented in Table 2. The most common cause of ketosis and ketoacidosis is decompensation of type 1 diabetes mellitus. Enhanced ketogenesis in this case is due, on the one hand, to a deficiency of insulin, on the other, to an excess of counter-insular hormones: glucagon, catecholamines, cortisol and growth hormone (GH). As already noted, contrainsular hormones activate mainly the catabolic part of energy metabolism, therefore, under conditions of insulin deficiency, glycolysis, glycogenolysis, gluconeogenesis and lipolysis increase. Massive lipolysis is accompanied by an increase in the blood level of free fatty acids (FFA), from which ketone acids are synthesized in excess in the liver under the influence of glucagon. And since with a lack of insulin, all anabolic processes slow down, including the utilization of keto acids, the latter accumulate in the blood with the inevitable development of metabolic acidosis, i.e. ketoacidosis (Fig. 2). Ketosis, especially ketoacidosis in type 2 diabetes mellitus, is a rare phenomenon, since in this type of diabetes there is no insulin deficiency. It would be more correct to say that there is relative insulin deficiency, which implies a weakened action of insulin in organs and tissues. It should be taken into account that the effect of insulin on adipose tissue is tens of times stronger than on other tissues, therefore, with decompensation of type 2 diabetes, there is (mainly) an increase in glycemia, and lipolysis and ketogenesis almost do not increase [1]. However, if decompensation of type 2 diabetes mellitus occurs against the background of ketogenic factors or conditions (Table 2), ketosis and even ketoacidosis are quite likely. Overproduction of ketoacids and ketoacidosis during chronic alcohol intoxication, more precisely, 1–2 days after excessive alcohol consumption, are such frequent phenomena that even the special term “alcoholic ketoacidosis” has been adopted. The metabolism of ethanol in the body is carried out by the liver enzyme alcohol dehydrogenase. This enzyme converts ethanol into acetaldehyde, which, in turn, activates the formation of NAD–H, and the latter promotes the synthesis of acetoacetate and especially ? –hydroxybutyrate. Another consequence of alcohol intoxication is inhibition of gluconeogenesis and a decrease in blood glucose levels. Hypoglycemia stimulates lipolysis, which also promotes enhanced ketogenesis. In addition, withdrawal syndrome is characterized by dehydration, which also contributes to the development of ketoacidosis. Unlike ketoacidosis of another nature, patients with alcoholic ketoacidosis are usually in a soporous state. Moreover, due to preferential education. ? -hydroxybutyrate, the nitroprusside test for determining keto acids usually gives a negative result. All this makes it very difficult to diagnose alcoholic ketoacidosis. Ketosis during prolonged vomiting, malnutrition or starvation is a classic compensatory process designed to compensate for the energy deficit, more precisely, the lack of carbohydrates, due to alternative energy substrates - keto acids. This mechanism was discussed above. It is appropriate to repeat here that keto acids inhibit their own production based on an allosteric mechanism, so their excessive accumulation and the development of ketoacidosis in this situation is unlikely. At the same time, if severe dehydration occurs during toxicosis of pregnancy or uncontrollable vomiting of another nature, then ketoacidosis is possible [4]. The pathogenesis of ketosis during thyrotoxicosis, excess glucocorticoids or deficiency of gluconeogenesis enzymes is essentially similar to the already discussed mechanisms of hyperproduction of ketoacids due to an excess of contrainsular hormones or due to a deficiency of endogenous glucose synthesis. Interest in ketogenic diets continues unabated because... It is ketosis that is the most effective mechanism of adipose tissue catabolism. Given the popularity of diet therapy and at the same time the acute problem of obesity, the European Parliament instructed its commission on food safety to consider the most popular and scientifically based diets in Europe. A group of 18 scientists representing 12 European countries was formed. This group comprehensively reviewed about 15 low-calorie diets (RCDs) from the point of view of safety of use, indications, absolute and relative contraindications, side effects, complications and other aspects [12]. Three chapters of this report were devoted to ketosis; ketosis and protein catabolism with NCD (6.4), ketosis and calcium balance with NCD (6.5), and ketosis and hyperuricemia with NCD (chapter 6.6). In September 2002, the expert report was approved at a meeting of the European Parliament commission [12]. The report found that despite obvious contraindications, most diets are distributed through grocery department stores or pharmacies. Four diets are distributed through medical consultants, and one is used only under medical supervision. Only a doctor can prescribe this low-calorie diet. This diet is the French Insudiet - in Europe better known as the Eurodiet [13,14]. According to the manufacturers, the first two phases of this diet are ketogenic, therefore, the diet should not be accompanied by a feeling of hunger and should be quite effective. Like any medical technology, procedure or medicine, any method of losing excess weight must undergo registration, certification and clinical trials in the Russian Federation. In the Department of Clinical Diagnostics and Prevention of Nutritional Disorders of the Clinical Nutrition Clinic of the State Research Institute of Nutrition of the Russian Academy of Medical Sciences, in the summer of 2003, clinical trials of high-protein products “Eurodiet ® ” were conducted using the “Eurodiet ® ” method, produced in France [15]. Clinical analysis of the patients’ urine confirmed the appearance of ketone bodies during diet therapy, which confirms the mechanism of weight loss due to lipolysis while taking hypocaloric high-protein products “Eurodiet ®”. The resulting ketone bodies, acting on the hunger center, contribute to the manifestation of their double action. The anorexigenic effect was that ketone bodies, in addition to stimulating the satiety center in the hypothalamus, caused a physiological appetite suppressant effect. Keton bodies provide about 80% of the entire needs of the brain for energy and have psychotonic properties in the form of an antidepressant effect. In conclusion, it is necessary to emphasize once again that ketosis is an initially compensatory phenomenon, which means physiological. Usually, with starvation or hypocaloric diet, ketosis does not pose a danger, because does not reach the degree of ketoacidosis. Such a development of ketosis is possible only as a result of the action of additional ketogenic factors, for example, dehydration or alcohol intoxication. Accurate compliance with diet therapy conditions in combination with qualified laboratory and medical monitoring guarantee the safety of a hypocaloric diet, at least in relation to ketoacidosis.
Literature 1. Lukyanchikov V.S., Zefirova G.S., Korolevskaya L.I. Emergency conditions of an endocrine-metabolic nature. -Moscow. SIP RIA: – 2003. – 340 pp. 2. Bistrian BR, Sherman M., Young V. // The mechanism of nitrogen sparing in fasting supplemented by protein and carbohydrate. J. Clin. Endocr. Metab. –1981.–Vol. 53.– No. 3. – P.874–878. 3. Davie MW, Abraham RR, Hewins B., Wynn V. // Changes in bone and muscle constituents during dieting for obesity. Clin. Sci. – 1986. – Vol.70. – No. 1. – P.285–293. 4. Davies HJ, Baird IM, Fowler J, et al. // Metabolic response to low– and very–low–calorie diets. Amer.J. Clin.Nutr. – 1989.– Vol.49.– No. 2. – P.745–751. 5. Festi D., Colecchia A., Orsini M., et al. // Gallbludder motility and gallstone formation in obese patients following very low calorie diets. Use it (fat) or lose it (well). Int. J. Obes.Relat. Metab.Disod. – 1998. – Vol.22. – P.592–600. 6. Foster DW C diabetes mellitus. In the book: Internal diseases (translated from English). Red E. Braunwald and others. Moscow. Medicine: – 1997. – T.9. pp. 185–232. 7. Marino PL Intensive care (translated from English). Moscow. GEOTAR, Medicine: –1998. –639 pp. 8. National Task Force on the Prevention and Treatment of Obesity. National Institutes of Health. Very low-calorie diets/JAMA. – 1993. – Vol.270. – P.967–974. 9. Nishizawa Y., Koyama H., Shoji T., et al. // Altered calcium homeostasis ac–companying changes of regional bone mineral during a very–low–calorie diet. Amer.J.Clin.Nutr. –1992. –Vol.56. –P.2655–2675. 10. Sherwin RS, Hendler RG, Felig P. // Effect of ketone infusions on aminoacids and nitrogen metabolism in man. J.Clin. Invest.–1975. –Vol.55. –P.1382–1390. 11. Van Itallie TB, Yang M–U // Cardiac dysfunction in obese dieters: a potentially lethal complication of rapid massive weight loss. Amer.J.Clin.Nutr. – 1984. – Vol. 39. – P.695–702. 12. Report of medical experts on special therapeutic nutrition for the Commission of the European Parliament on the safety of therapeutic low-calorie nutrition: https://europa.eu.int/comm/food/fs/scoop/7.3_en.pdf 13. Link to the website: www. eurodiet.com 14. Link to the website: www.eurodiet.ru 15. Report on clinical trials of Eurodiet® products using the Eurodiet® method, France. Prepared by the head of the department of therapeutic and preventive nutrition of the State Research Institute of Nutrition of the Russian Academy of Medical Sciences A.N. Stenin, head of the department of clinical and instrumental research methods, Doctor of Biological Sciences. A.V. Vasilyev, Head of the Department of Clinical Diagnostics and Prevention of Nutritional Disorders M.V. Chebotareva; approved by the Director of the State Research Institute of Nutrition of the Russian Academy of Medical Sciences, Academician of the Russian Academy of Medical Sciences, Professor V.A. Tutelyan. Moscow, 2003.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Diagnostics
Fasting ketoacidosis is uncommon in healthy people, as it occurs due to a lack of glucose in the diet after long periods of fasting.
Therefore, when fasting ketoacidosis occurs, the doctor may look for other causes of weight loss, which may delay diagnosis and treatment.
If you experience unexplained weight loss, be sure to tell your doctor about:
- any other symptoms
- your diet
- any underlying diseases
According to the 2021 article, the doctor first needs to stabilize the patient before performing necessary tests, including blood tests to check for electrolyte abnormalities and vitamin deficiencies. If a patient is diagnosed with fasting ketoacidosis, the doctor will prescribe appropriate treatment.
Reason four: micronutrient deficiencies and health problems
“When your brain (neurons) get a boost of fresh energy from ketones, you feel fresher in your thoughts. It’s like a breath of clean air in conditions of thick urban (carbohydrate) smog - it seems that you can’t say it better than Anatoly Nikolaev, general practitioner, nutritionist, member of the Association of Preventive and Anti-aging Medicine of Ukraine. – But if keto exists, but there is no effect, I would look towards intoxications, deficiencies or hormonal disorders. I would take it as a symptom.”
Geneticist, Candidate of Medical Sciences, Karina Fomicheva explains: “The reasons for the lack of miracle effects of ketosis may be that you have any undiagnosed health problems that are not solved by the keto diet, for example, hypothyroidism or chronic fatigue syndrome. Or you have mineral and vitamin deficiencies, which are often the same thing.
Yulia Kiltina, general practitioner, agrees: “Undiagnosed hypothyroidism is possible. To check this, you need a TSH test. Above 4 – you should contact an endocrinologist to compensate for the thyroid gland.
The second probable cause is unresolved deficiencies, most often iron deficiency. Hemoglobin may be normal in case of latent deficiency; you need to look at ferritin. Below 15 is a definite deficit, below 45 is a probable deficit. Iron supplements as prescribed by a doctor will correct the situation.”
Elena Rybatskaya also notes insufficient attention to electrolytes as the reason for the lack of vigor and productivity on keto.
And Olga Bezuglaya recommends paying attention to common deficiency conditions - lack of vitamins B, C, E, D, A, zinc, iron and omega-3.
Treatment
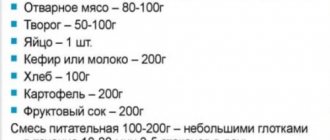
Fasting ketoacidosis occurs when the body is deprived of essential food and energy for an extended period. While food may seem like an obvious treatment, it can be dangerous for those who have been undernourished for a long time.
When a doctor treats a patient for fasting ketoacidosis, he or she needs to carefully monitor electrolytes. During the process of introducing food, doctors will need to check and restore the patient's potassium, phosphate and magnesium.
One case study involved an anorexic patient who developed fasting ketoacidosis. Doctors treated him with dextrose solution for 15 hours, during which time his ketoacidosis improved.
With proper treatment, including treatment for underlying conditions such as anorexia, the patient should make a full recovery.
What is the ketogenic diet
The ketogenic or keto diet is a low-carbohydrate, high-fat, moderate-protein diet. It involves consuming less than 50g of carbohydrates per day, with the standard norm being 200–300g.
The diet was developed in the 1920s to treat childhood epilepsy. It was observed that fasting reduced the frequency of epileptic seizures in children and adolescents. Since fasting is only possible for a short time, it was decided to simulate hunger by eliminating the main source of energy - glucose. With proper adherence to the ketogenic diet, seizures stop completely in 60% of children, and are reduced by half in 35%.
Because the keto diet involves eating almost exclusively fat, it has certain health risks. Therefore, nowadays it is prescribed only in case of failure of treatment with antiepileptic drugs.
Dieting for medical purposes is taught in a hospital setting. After this, at least three specialists guide and observe the patient. If effective, keto nutrition is followed for another 1–2 years, no more. Even such patients do not live on keto for years. Doesn't all this indicate the seriousness of the process?
Since 1960, diet has been considered an effective way to reduce excess weight. Today it is still very popular despite all the risks it carries.
Conclusion
Fasting ketoacidosis is an uncommon form of ketoacidosis. It occurs when you don't eat enough food regularly or your body can't absorb nutrients properly.
A doctor can check for fasting ketoacidosis with blood tests and will need to monitor the patient as they begin to eat again.
Most healthy people are not at risk. However, those who suffer from eating disorders and those who have undergone certain medical procedures may be at higher risk of developing fasting ketoacidosis.
Full recovery is usually possible after treatment.
Reason six: not enough food
The mantra of the keto diet is to eat until you are full. But switching to a high-fat, low-carbohydrate diet can be psychologically difficult after many years on a “proper diet,” where you had to eat a portion and a little. “A common story is that you eat a keto diet according to keto proportions, but count yourself such a ridiculous amount of calories that you have no strength to think or move,” notes Olena Islamkina, a keto diet specialist and creator of the “Weight Loss on a Keto Diet” course. “Paradoxically, if you don’t eat enough on a keto diet, you won’t lose weight or experience those pleasant bonuses that we love keto so much for.”
Short-term fatigue
Switching to a ketogenic diet can come with a number of side effects. These include weakness and fatigue. Because of this, people often leave the keto diet without getting everything that full-fledged ketosis could give them. It usually takes 7-30 days to achieve full ketosis, sometimes longer, depending on your age and body characteristics. To reduce fatigue, take extra electrolytes, which are lost due to the rapid drainage of water held by carbohydrates in the body. Use 2000-4000 mg sodium per day, 1000 mg potassium and 300 mg magnesium .
NB: You may initially suffer from fatigue and loss of energy, but this will pass as you adapt to the ketones. At this time, you should not engage in exhausting sports activities.
Test strips for determining ketosis.
Another way to check whether you are in a state of ketosis is to use special test strips, explain experts from the University of Rochester Medical Center . They are widely available both in stores and online. The principle of their operation is the same as that of pregnancy tests. They analyze the composition of the urine, turning dark purple if the result is positive.
Wash your hands thoroughly both before and after using the test strips. They themselves are made of paper. Therefore, they can be flushed down the toilet and the plastic shell thrown into a bucket.
If the test turns dark purple and your urine is very dark, your body is dehydrated. You need to immediately increase the amount of water you drink. Drink a full glass, fill a bottle and keep it with you at all times, sipping periodically throughout the day. Especially if you start to have a headache, become irritable, or feel dizzy.
What to do if you fall out of ketosis
It is natural for our body to switch from one type of fuel to another. It was created and improved when there was little food, for the sake of it one had to go far, run, and fight. When your ancient ancestor came across raspberry bushes, he peeled them clean and did not think about how he could return to ketosis. This happened on its own when he was starving or stealing eggs from nests. What our body is not used to is an abundance of carbohydrates. Therefore, you need to make sure that you do not leave ketosis, but that the amount of carbohydrates is generally small, even if on some days it exceeds 20-25 g. If you have openly violated the regime, there is nothing special (except for conclusions about why it happened), there is no need to do it.
What to do with failures on keto?
Ketosis gives you a lot of energy, helps reduce inflammation in the body, improves mood and brain function. On the keto diet, you will be cheerful and energetic, and gain independence from food. Learn to listen to your body and determine ketosis by pleasant signs , not by instruments. Eat whole, natural foods without industrial processing, think about the quality of food, not the quantity.
Share this post:
Digestive problems
Switching to a ketogenic diet involves making significant food changes. A fairly common side effect when starting a keto diet is constipation and diarrhea. These problems should subside after the adaptation phase, but it is important to be aware of which foods may cause digestive problems. For example, too much nuts can cause diarrhea, and too much protein can cause constipation. Remember to eat plenty of green, leafy vegetables, which are high in fiber. There is a lot of it in shirataki noodles and psyllium.
NB: These side effects occur frequently, but not always.
Diet for ketosis
High carbohydrate diet
- Efficiency: when following a strict diet, weight loss is 3-5 kg in 7 days
- Time frame: 7 days
- Cost of products: 1300-1400 rubles. in Week
Although ketosis is a physiological adaptive reaction, at its first signs it is recommended to introduce foods containing carbohydrates, as well as reduce fat intake, eat more often and in small portions. The diet should be based on such products as:
- dietary meat;
- berries and fruits - can be consumed in the form of compotes, juices, salads, etc.;
- fresh vegetables and puree soups;
- porridge.
How to Determine Ketosis
You don't have to buy keto strips or spend money on lab tests. A ketogenic person can tell when ketosis begins by the following signs:
Energy
This is one of the most pleasant keto effects: strength is overflowing, laziness goes away. This is especially clear if you had to go through a period of keto flu. Expect to first feel exhausted and then work like a nuclear reactor.
No hunger
Keto diet gurus can eat once a day (don't try to force this feat). A side effect of ketosis is a prolonged feeling of fullness. This is due to the fact that B-hydroxybutyrate affects the production of ghrelin, the hunger hormone, and cholecystokinin, a neurotransmitter that brings a signal of satiety.
Thirst
An unpleasant consequence of ketosis is that you want to drink more than usual. Insulin (carbohydrates) holds fluid in the body. When its indicators return to normal, the water is retained for a short time and requires constant replenishment. Drinking regularly also helps get rid of the acetone smell that sometimes appears in ketosis. True, another sign of ketosis that people don’t like to talk about is that you will run to the toilet more often, but somewhere you have to put all that water.
Why do you feel thirsty on keto?
Bright head
This is noted by everyone who switches to the keto diet. The “fog” that was on the carbohydrate diet goes away, thoughts become clearer. Moreover, only with the transition to the keto diet do many people understand that before this the thought process was not at full capacity.
General information
Ketosis is a state of the body that occurs during cellular carbohydrate starvation . The mechanism is based on the switching of metabolism in the absence of carbohydrates to the breakdown of fats for energy, which occurs with the formation of a significant amount of ketone (acetone) bodies .
This adaptive reaction is activated when carbohydrate food enters the body in insufficient quantities. An evolutionary adaptation in the form of ketosis made it possible for people to survive when there was a shortage of carbohydrate-rich foods of plant origin and they had to switch to eating foods of animal origin - the keto-adaptation effect developed. In this case, ketone bodies are formed exactly as much as the released energy is needed for the body.
Ketosis in humans is a normal physiological state, in contrast to ketoacidosis , a pathological condition characterized by such a high content of ketone bodies in the bloodstream ( hyperketonemia ), which causes a shift in the acid-base balance of the body towards acidic pH values, which even pose a threat to life, because the ketone bodies formed not everyone undergoes the breakdown as in ketosis. The body’s attempts to intensively remove their excesses through urine ( ketonuria ), through skin pores and breathing, through excretion, do not give the necessary effect and completely restore the acid-base balance.
Scientific research
Proponents of keto nutrition promise quick and easy loss of the first kilograms. Is it so?
Indeed, even at the very beginning of following the keto diet, it is capable of reducing weight by 2 or more kg faster than other diets. But not due to fat. And due to the depletion of glycogen reserves and associated water.
When it comes to weight loss in general, high-quality studies have shown no significant difference in weight loss between low-carb and low-fat diets. However, the ketogenic diet increased blood cholesterol.
A meta-analysis published in 2021 showed how the amount of carbohydrate consumption and mortality are related . It turned out that participants with low consumption had the highest risks of death from cardiovascular diseases and cancer.
Other 25-year studies and meta-analyses involving nearly 500,000 participants have reached the same conclusions. They showed that low (less than 40%) as well as high (more than 70%) carbohydrate intake is associated with an increased risk of death. Moreover, we are talking about significantly higher consumption than the keto diet recommends.
Scientists and doctors recommend sticking to a healthy middle range of 45-55% carbohydrates in your diet. It is this quantity that brings all the benefits. The World Health Organization recommends consuming at least 400 g of vegetables, herbs and fruits, as well as whole grains, daily.
Thus, the potential risks outweigh the slightly faster weight loss benefits of the keto diet.
Research into the treatment of neurological diseases such as Alzheimer's, Parkinson's, and multiple sclerosis continues. There is not yet enough data to declare their effectiveness.
Research has not yet confirmed any metabolic benefits.
In addition, the role of the ketogenic diet in the management of insulin-dependent diabetes is being explored. The website of the global diabetes community already has advice on using a low-carbohydrate diet to lower blood glucose levels in type 1 and type 2 diabetes.
However, the long-term effectiveness, safety, and benefits of the keto diet have not been fully studied. Therefore, it is too early to draw conclusions, much less recommend keto nutrition to anyone for a long period of time.