Blood pressure indicators are becoming an important marker in determining a person’s well-being. Moreover, doctors equally monitor both the increase and decrease in readings on the tonometer. At the same time, people often have questions. For example, since there are two indicators - upper and lower pressure - which one is more important?
Associate Professor of the Department of Hospital Therapy named after A.N. Academician P. E. Lukomsky Faculty of Medicine, Russian National Research Medical University named after. N. I. Pirogova, Ph.D., cardiologist, therapist, functional diagnostics doctor Maria Benevskaya .
Set priorities
“The first thing I would like to talk about when answering the question about which indicator is more important is what blood pressure actually is and what the measured parameters indicate. Blood pressure (also called blood pressure) is the pressure that blood exerts on the walls of blood vessels. This parameter is one of the indicators of the vital functions of the body,” notes Maria Benevskaya.
When measuring blood pressure, as the cardiologist says, two types are determined: with each heartbeat, the blood pressure fluctuates between the highest, systolic (from the ancient Greek “compression”), and the lowest, diastolic (from the ancient Greek “rarefaction”) "), which are colloquially called upper and lower. Thus, the magnitude of the force acting on the vessels is determined by two parameters: upper (systolic) and lower (diastolic) pressure. Therefore, we cannot say that any of these parameters is more important. They both have their meaning.
“Everyone knows that the normal blood pressure of a healthy person (systolic/diastolic) is 120 and 80 mmHg. Art., but we must also remember that normal boundaries change depending on age and existing diseases. The difference between systolic blood pressure and diastolic blood pressure is called pulse pressure and is normally 30-50 mmHg. Art.,” the specialist emphasizes.
We fight the pressure. 8 drinks for hypertensive patients Read more
What is the prevention of high blood pressure?
People who experience high blood pressure need to remember the need for regular checks. Often a person does not feel symptoms and does not suspect what danger blood pressure hides. Even with long-term hypertension, people ignore the condition, attributing everything to fatigue or overwork. It is important to understand that pressure increases when blood vessels narrow, when the heart has to work at “high speed.”
Foods containing large amounts of saturated fatty acids can lead to hypertension. The highest content of these substances is found in butter, cheeses, and sour cream. It is recommended to avoid products containing large amounts of palm oil. Cake, chocolate, cookies, fatty sausage, chips are all sources of saturated fatty acids. Of course, it is important to take into account physical activity; you need to eat exactly as much as the body needs to ensure normal functioning. Moreover, you need to take into account the composition of the products. Many manufacturers even indicate the percentage of EFA content per 100 grams.
The amount of salt consumed also needs to be reduced. Scientists have long noticed the effect it can have on the human body when consumed excessively. The biggest problem is that most foods sold on supermarket shelves contain quite a bit of salt. By using this additive in our diet, we expose our body to even more danger. For those who love salty foods, the best option to get rid of excess is physical activity. Salt can reduce the elasticity of blood vessels and negatively affect the kidneys and liver.
Renal or cardiac?
There is an opinion that the upper pressure indicator is cardiac, and the lower one is renal. “The top number is systolic blood pressure, it shows the pressure in the arteries at the moment when the heart contracts and pushes blood into the arteries, it depends on the force of the heart contraction, the resistance that the walls of the blood vessels exert, and the number of heartbeats per unit time. Therefore, in general, we can say that this indicator reflects the work of the heart, although, of course, other factors also take part in this process,” says Maria Benevskaya.
It is also not worth ruling out that the lower indicator reflects kidney function. “The bottom number is diastolic blood pressure, which shows the pressure in the arteries when the heart muscle relaxes. This is the minimum pressure in the arteries and reflects the resistance of peripheral vessels. Since vascular tone is regulated by chemicals and the autonomic nervous system, lower blood pressure indicates the extent to which neurohumoral regulation is carried out correctly. In turn, neurohumoral reactions occur mainly in the kidneys, which is why there is an opinion that the “lower” pressure is renal. But it would be more correct to note that lower pressure reflects the work of blood vessels and kidneys,” says the cardiologist.
Lack of oxygen, loss of strength. How pressure surges affect the brain Read more
What reasons can cause high blood pressure
Medicine has established the most common causes that can cause high blood pressure in the human body. These include influencing factors such as drugs, diseases of the urinary system, endocrine diseases, aortic diseases, complications arising during pregnancy, problems with the nervous system.
Antidepressants and glucocorticosteroids (for example, prednisolone) can cause high blood pressure. Contraceptives can also have a negative impact. Risk factors that can lead to the development of hypertension include the following:
- Hereditary factors.
- Prematurity.
- A child's low weight may indicate a potential predisposition to high blood pressure.
- Large overweight.
- High salt content in food. The norm for table salt consumption is considered to be 5 grams per day.
- Drinking alcohol, smoking. Bad habits can worsen the condition of blood vessels and affect the circulatory system in the most detrimental way.
- Insufficient physical activity.
- Poor environment, daily stress, increased noise levels.
Of all these factors, it is necessary to focus a lot of attention on excess weight, bad habits, and severe stress. In most cases, these reasons increase the risk of hypertension.
Importance of indicators
So is it possible to conclude which of these indicators is more important? “As we have already figured out, each of these parameters has its own meaning, so they are both important. Currently, it is also customary to distinguish between isolated systolic hypertension, when only the upper pressure is increased, and isolated diastolic hypertension when only the lower pressure is increased. Each of these forms has its own prognostic significance and some features in treatment, so it is necessary to approach the identification and correction of these types of hypertension with equal attention,” notes Maria Benevskaya.
Detection and elimination of the disease
Diagnosis of vascular hypertension is complicated by its neurological nature. The most effective diagnostic methods remain long-term monitoring of lower pressure (symptoms are collected in different states and moods).
An important point in diagnosis and treatment is the study of the symptoms of diseases of the central nervous system. Their elimination is one of the forms of treatment for hypertension of the vasculature .
Therapeutic practice
Treating vascular hypertension with medication alone is risky for two reasons.
- Diuretics in combination with beta blockers with long-term treatment lead to kidney disorders.
- Intervention without eliminating the symptoms of the disease that caused the need for treatment of vascular hypertension and its diagnosis disrupts the process of blood pressure correction in the body.
An important role in the treatment of the disease is played by exercises - breathing, water, meditative (the goal is to calm the central nervous system). If the diagnosis has revealed the physical causes of vascular hypertension , then in the practice of its treatment it is necessary to use a diet (to reduce the level of salt consumed and equalize weight).
Taking corrective medications is possible as part of complex treatment. Diuretics may be prescribed during treatment to prevent a crisis if diagnosis has revealed a serious degree of development of the disease. Often, when treating vascular hypertension, it is recommended to take sedatives .
Attention to the gap
Of course, as experts note, it is also necessary to look at the gap between these parameters. “I repeat that the normal difference between upper and lower pressure is from 30 to 50 mm Hg. Art. All values that do not fit within these limits may indicate the presence of pathology, and this is already a reason to undergo additional examination. Although at the same time this may be due to the individual characteristics of the body and physiological conditions. But in any case, it’s better to see a doctor so as not to miss the disease,” notes Maria Benevskaya.
So, for example, the specialist emphasizes, a small difference may indicate:
- the presence of atherosclerosis of the aorta (deposition of cholesterol in the largest vessel);
- damage to the kidney vessels;
- aortic aneurysm (pathological expansion of a separate section of the aorta with the possibility of rupture or dissection of the walls due to excessive load);
- anemia (decreased hemoglobin levels in the blood) and many other conditions.
“An increase in the difference may be a consequence of osteochondrosis of the cervical spine, aggravated by a malnutrition of the brain (most often vertebrobasilar insufficiency). Diseases of the musculoskeletal system lead to weakening of cerebral blood flow. Hence the problems with upper and lower pressure in general,” notes the cardiologist.
Also, as Maria Benevskaya says, various endocrine diseases can lead to changes in pulse pressure. And this is not the entire range of pathologies that affect this parameter. A change in this indicator can be a “bell” to pay attention to your health.
Hot towel and vinegar. What folk remedies quickly reduce blood pressure? More details
In recent years, when assessing the impact of various antihypertensive therapy (AHT) regimens on the clinical outcomes of arterial hypertension (AH), their impact on the values of central aortic pressure (CAP) and reflected wave index (augmentation index - AI) began to be considered. Previously, a number of smaller and shorter-term studies have shown that antihypertensive drugs have different effects on the pulse wave pattern and central hemodynamic parameters, despite the same ability to reduce blood pressure (BP) in the brachial artery. The ongoing debate about the varying clinical effectiveness of antihypertensive drugs [1, 3], in addition to their metabolic effects, really forces us to pay closer attention to the hemodynamic mechanisms of their action [2].
Pressure level and distribution of blood volumes in various parts of the vascular bed of the systemic circulation
The value of CDA is the most integrative hemodynamic indicator [5], the value of which depends on cardiac output, peripheral vascular resistance, the stiffness of large and medium-sized arteries, as well as the magnitude of the reflected wave.
In this regard, it seems very important to understand the morphofunctional characteristics of various vessels of the circulatory system, the meaning of CDA and the terminology of indicators characterizing the elasticity of large arteries. It should be remembered that about 85% of the total blood volume is concentrated in the systemic circulation, and about 15% in the pulmonary circulation and the heart (Fig. 1).
Shock-absorbing vessels include elastic-type arteries (aorta, pulmonary artery and adjacent sections of large main arteries). Their wall contains many elastic fibers, which allows them to absorb (smooth out) significant fluctuations in blood pressure caused by the systolic ejection of blood into the aorta and pulmonary artery (compression chamber effect). The maximum severity of pulsating oscillations is observed precisely at the level of the aorta and large arteries. The pulsating nature of pressure changes in the aorta is due to the fact that with each contraction of the heart a volume of blood equal to the magnitude of the stroke ejection enters it. The distensibility of the aorta is equal to the quotient of the change in volume divided by the change in pressure. With an increase in pulse blood pressure and/or stroke volume, a sharp decrease in aortic distensibility occurs (Fig. 2), which further increases pulse blood pressure (stroke volume/aortic distensibility). The negative consequences of increased pulse blood pressure in terms of its impact on the risk of developing cardiovascular complications are well known. In addition, as follows from the presented data, the maximum level of blood pressure is observed in the aorta and then gradually decreases to zero level in the vena cava.
Resistive vessels include mainly arteries and arterioles, which are characterized by a relatively small lumen and powerful smooth muscle walls. They account for about 50% of the total vascular resistance to blood flow, although their total capacity is relatively small. In the terminal arteries and arterioles, the blood pressure level decreases by approximately 1.5–2.0 times compared to the pressure in the aorta, and the pulsating blood flow gradually becomes continuous. In the capillaries, where about 6% of the blood volume is located, its flow is uniform in different phases of the cardiac cycle.
The increase in pulse blood pressure occurs from the center to the periphery and is caused by an increase in reflected waves of pulse oscillations from the walls of the aorta and large arteries (Fig. 3).
It is known that the heart works as a pulse pump, pumping blood into the aorta in portions during each period of ejection (systole). Communication between the heart and the aorta is interrupted during the period of relaxation (diastole) when the aortic valve is closed. Therefore, changes in blood pressure in the aorta are pulsating in nature (Fig. 4). The maximum level of blood pressure corresponds to the largest integrated volume of blood entering the aorta during systole. The pressure of the blood in the distal slowly narrowing arteries decreases only to the diastolic level during each diastole. In the next expulsion phase, the whole process is repeated again. The level of systolic blood pressure is determined by the volume and viscosity of the blood, the rate of contraction of the heart muscle and the volume of the arterial bed. The level of diastolic blood pressure depends not only on blood volume and viscosity, but also on vascular resistance. If the heart worked as a constant rather than pulsating pump, blood pressure and blood flow would remain at the same constant level.
Relationship between aortic distensibility and blood pressure
Propagation and amplification of the pulse wave
Thus, CDA is the hemodynamically significant blood pressure, which is the average pressure in the aorta during one cardiac cycle. Therefore, systolic CDA is the pressure in the aorta during systole, and diastolic pressure is during diastole. An important indicator reflecting the morphofunctional state of the aorta and large arteries is the index of increased central pressure or AI, which is the quotient of the maximum pressure during systole divided by the value of the central pulse pressure.
Change in aortic pressure during one cardiac cycle
Studies that used central pulse wave analysis
The magnitude of AI and survival of patients with hypertension
Central pulse pressure and renal function
Closer attention to CDA and AI forced them to be considered as independent prognostic risk factors for the development of cardiovascular complications. It has become obvious that in the near future there will be special interest not only in the analysis of pulse wave velocity, but also in central pulse pressure and AI [9]. Today there are already several studies [4] on this issue (Table 1) and the independent prognostic value of these indicators has become clear (Table 2).
Moreover, it has already been proven that an increase in AI and the value of central pulse pressure has an extremely negative effect on the prognosis for the patient’s life and the risk of complications (Fig. 5, 6).
In The Strong Heart substudy, which followed 2409 patients with hypertension for an average of 4 years, it was convincingly shown that systolic blood pressure is an independent predictor of the risk of developing cardiovascular complications, while the level of systolic blood pressure at the brachial artery is not. This is probably due to the fact that the CDA indicator more accurately reflects the degree of left ventricular overload.
A number of clinical studies [6] assessed the effect of antihypertensive drugs on central pulse blood pressure (Fig. 7). Undoubtedly, the largest and most significant for the further intensification of research on the effect of AHT on central pulse pressure and IA was the ASCOT study (Anglo-Scandinavian Cardiac Outcomes Trial). The fundamental differences identified between the two AHT regimens – amlodipine + perindopril and atenolol + bendroflumethiazide – are of great importance in the development of new recommendations for the treatment of hypertension.
Of undeniable interest is the analysis of the reasons why the treatment regimen amlodipine + perindopril (Prestance) turned out to be significantly more effective in influencing almost all clinical events studied (endpoints) than atenolol + bendroflumethiazide.
Among the possible reasons for these differences, the most frequently mentioned are the following:
• atenolol was doomed in advance to the role of a “beating boy”, because, according to meta-analyses and randomized clinical trials, it is considered far from the best representative of an extremely heterogeneous class of β-blockers. This means that the best drugs in their classes (amlodipine and perindopril) were compared with an obviously “weaker” rival - atenolol;
• the negative impact of the combination of atenolol + bendroflumethiazide on endpoints was due to its negative effect on metabolic parameters.
Hemodynamic differences were also very important when using Prestance and the thiazide-containing combination. The Conduit Artery Functional Evaluation (CAFE) substudy was conducted as part of ASCOT [7]. The prerequisite for its implementation was the assumption that different antihypertensive drugs have different effects on CDA with the same degree of reduction in blood pressure in the brachial artery.
Decrease in systolic and pulse blood pressure in the brachial artery (B) and aorta (A) under the influence of various classes of drugs
The CAFE study (n = 2073; mean age 63 years; 80% men) has been conducted at 5 sites in the UK and Ireland since 2001 (design shown in Fig. 8). Patients were included in the study one year after randomization in ASCOT against the background of optimally selected ADT.
Evidence from studies demonstrating a relationship between central pressure (at the aorta or carotid artery) and the risk of cardiovascular complications (OÁRourke, 2004)
Study design CAFE
DCA graph in the CAFE study
CAFE: Lower CDA and equal peripheral value in amlodipine+perindopril therapy compared with atenolol+bendroflumethiazide
Brachial artery blood pressure was measured at each visit three times at 5-minute intervals using an Omron 705CP semi-automatic oscillometric device. The data from the last two measurements were averaged. After this, the pressure curve in the radial artery of the same upper limb was recorded for 10 seconds (applanation tonometer SPC-301, Millar Instruments). The obtained data were processed using software (SphygmoCorversion 7, AtCor): the average shape of the curve was calculated, which was mathematically transformed into a CDA graph [2]. In this case, the following CDA parameters were determined: time to the first (T1) and second (T2) systolic peaks of the wave; the pressure at the first peak/kink (P1) was taken as the ejection pressure, a further increase to the second peak (ΔP) meant the reflected pressure, their sum (maximum pressure during systole) was the systolic central pressure (Fig. 9). Reflected wave amplification index (AIx) was calculated as the ratio of ΔP to central pulse blood pressure: Alx = (ΔP/PP) × 100.
Among some (n = 114) patients, the velocity of propagation of the pulse wave in the carotid-femoral area was determined (Complior SP, Artech-Medical).
At the time of inclusion of patients in the study, blood pressure in the comparison groups did not differ and averaged 160/93 mmHg. Art.; 95% of study participants received combined AHT. By the time the study was completed (Fig. 10), blood pressure in the brachial artery decreased by 26/13.8 mmHg. Art. in the atenolol group and by 27.8/15.7 mm Hg. Art. in the amlodipine group (difference in systolic blood pressure – 0.7 mm Hg; p = 0.2; difference in diastolic blood pressure – 1.6 mm Hg; p < 0.0001; difference in pulse blood pressure – 0 .9 mm Hg; p = 0.06).
Treatment with the β-blocker atenolol led to a broadening of the CDA curve with a more pronounced late systolic peak. At the same time, in the amlodipine + perindopril group, CDA in systole was significantly lower than in the atenolol + bendroflumethiazide group (difference – 4.3 mm Hg; p < 0.0001), and these differences were visible from the very beginning of observation. The decrease in CDA in diastole and pulse CDA was also slightly more pronounced in the amlodipine + perindopril group: the difference was 1.4 (p < 0.001) and 3.0 mm Hg. Art. respectively (p < 0.0001).
The higher CDA in the atenolol + bendroflumethiazide group was not associated with an increase in ejection pressure (P1), since it was lower compared to the amlodipine + perindopril group (difference – 0.8 mm Hg; p < 0.01 ). However, the increase in systolic CDA (ΔP) in the atenolol + bendroflumethiazide group was significantly higher (difference – 3.8 mm Hg, or 6.5%; p < 0.0001; Fig. 11, Table 3). The heart rate during β-blocker therapy was 10.7 beats lower than in the amlodipine + perindopril group (p < 0.0001), which led to an increase in ejection pressure time (T1) and reflected pressure time (T2). There were no intergroup differences in the speed of pulse wave propagation (p = 0.3).
In a retrospective analysis of the relationship between CDA and clinical events, it was found that pulse CPA, ejection pressure and systolic CPA growth were significantly associated with the combined endpoint (all cardiovascular events and interventions + development of renal failure). Using multivariate analysis (Cox regression model), after adjusting for age and baseline risk factors, pulse CDA remained an independent predictor of clinical events (hazard ratio, 1.11 to 1.13). At the same time, in the amlodipine + perindopril group, the risk of achieving the primary endpoint decreased by 16% (p < 0.0001).
On this basis, it was concluded that antihypertensive drugs have different effects on CDA and central hemodynamics, despite similar changes in brachial artery blood pressure, and pulse CDA may serve as a major hemodynamic determinant of cardiovascular outcomes. Apparently, it is the relationship between the nature of AHT and changes in CDA that largely explains the differences in the incidence of cardiovascular complications between the atenolol + bendroflumethiazide and amlodipine + perindopril groups noted in the ASCOT study.
Among the possible reasons for the lower effect of the atenolol + bendroflumethiazide regimen on CDA, the authors of the CAFE study point to the prolongation of ejection time and the delay in peak ejection pressure when taking these drugs, which increases the likelihood of an increase in reflected pressure during systole. They also do not exclude that possible vasoconstriction when taking β-blockers leads to a more proximal shift of the areas generating reflected pressure, thereby increasing the increase in CDA.
The above hypotheses, in fact, boil down to another statement of the adverse (in this case hemodynamic) effects of the combination of atenolol + bendroflu-methiazide. With this approach, there is a certain underestimation of the powerful angioprotective potential of the amlodipine + perindopril combination [10]. The very mechanism of action of ACE inhibitors contains the ability to have a beneficial effect on vascular elasticity (Fig. 12).
CAFE was the second large study after REASON [8], which showed that AHT, including perindopril, leads to a significant decrease in pulse blood pressure, improvement in vascular stiffness and CDA.
CAFE: differences in blood pressure under different AHT regimens: amlodipine + perindopril versus atenolol + bendroflumethiazide
CAFE: IA in different treatment regimens CAFE
Mechanism of action of ACE inhibitors
Interestingly, in another ASCOT substudy, Conduit Artery Function Evaluation-Lipid-Lowering Arm (CAFE-LLA), the hypothesis that statins also have a beneficial effect on CDA and hemodynamics was not confirmed [11]. In this study, treatment with atorvastatin 10 mg/day in 891 patients with total cholesterol ≤ 250 mg/dL and hypertension was compared with placebo. The patients were observed for 3.5 years. As expected, atorvastatin reduced low-density lipoprotein cholesterol and total cholesterol levels by 32.4 and 35.1 ml/dL, respectively. However, there were no differences between atorvastatin and placebo in their effect on the function of the great arteries and central hemodynamic parameters (brachial artery blood pressure, blood pressure, heart rate, etc.).
Thus, the results of CAFE and a number of other studies allow us to draw at least two important conclusions:
In patients with hypertension, “new” combinations (Prestance) compared with “old” drugs (atenolol + bendroflumethiazide) have a more favorable effect not only on the risk of developing cardiovascular complications and indicators of metabolic control, but also on hemodynamics, as well as the elasticity of large arteries .
From the standpoint of evidence-based medicine, AHT, including perindopril, has the greatest positive effect on pulse wave velocity, CDA and IA in patients with hypertension.
Adjust individually
The question of whether it is possible to adjust indicators separately is also of concern to many. “Basically, all the drugs that we use to correct high blood pressure act on both upper and lower pressure. However, among the classes of antihypertensive drugs, we have the opportunity to select drugs with a predominant effect on systolic or diastolic pressure. Therefore, it is possible to implement a personalized approach to the patient based on his needs,” notes Maria Benevskaya.
For example, she says, medications that have a vasodilating effect will be more likely to cause a decrease in diastolic (lower) blood pressure. And drugs that reduce the force of heart contractions will reduce systolic (upper) blood pressure to a greater extent.
Mechanism of increased blood pressure
Blood pressure is regulated by a complex system of stimulation or inhibition of blood flow in the vessels. An increase in pressure occurs with an increase in the volume of cardiac blood output per minute and the resistance of the vascular bed. This physiological process is controlled by the hypothalamus and the vasomotor center located in the brain stem.
Three main reasons can lead to an increase in blood pressure:
- narrowing of the arterioles of the systemic circulation;
- a shift of blood masses towards the heart due to narrowing of the veins - this leads to an expansion of the heart cavity, an increase in tension in the heart muscles and an increase in the volume of blood ejection;
- increased cardiac activity based on a signal from the sympathetic nervous system.
Blood pressure in teenagers
Deviations in blood pressure are increasingly common in children and adolescents. There are often cases when a teenager aged 14-18 years is already diagnosed with hypertension.
The children's body is characterized by lower blood pressure parameters, in contrast to adults. As a rule, the younger the child is, the more elastic the vascular walls of the arteries are, resulting in lower blood pressure.
Blood pressure in teenagers and children depends on how old they are:
- If the child is less than 15 days old – 59-90/40-50.
- At the age of 15-30 days – 80-110/40-70.
- From 2 months to a year 95-116/50-76.
- At the age of 2-3 years - 105-110/50-80.
- At 6-9 years old – 110-120/59-79.
- For a teenager 10-12 years old – 110-130/75-85.
- For a teenager aged 13, 14 and 15 years – 115-130/75-90, for children aged 16-18 years – 110-120/70-80.
Based on statistics, we can say that 12-14% of adolescents aged 14-18 years have slightly elevated blood pressure. As a rule, in a third of children this is due to impaired renal function. Risk factors in this situation are:
- Stressful condition, depression.
- Rapid physical development.
- Excess weight.
- Excess sodium accumulated in the body of a teenager.
Modern medical research has revealed a correlation between high blood pressure and adolescent diseases such as scoliosis and poor posture. As a result of such pathological conditions, venous outflow is disrupted and neurocirculatory dystonia develops.
These teenagers often experience headaches, which usually get worse at the end of the day or during mental stress. Painful sensations in the heart area often occur, which are pressing or aching in nature.
You may notice short temper in children, changeable mood, memory impairment, and unreasonable fatigue.
It is worth noting that with all this, there is also that third of children who feel great with high blood pressure and do not experience any discomfort. And such indicators are detected during preventive medical examinations.
If a teenager has low blood pressure, the following actions should be taken:
- Herbal medicine - regular green tea, rosemary, tansy.
- Hardening is cold foot baths or a contrast shower, when cold and hot water alternate.
- Optimal physical activity.
In cases of high blood pressure, you should also pay attention to your physical condition and introduce a special diet - reduce the consumption of baked goods, sweets and smoked meats. Not only human health, but also his life depends on normal blood pressure.
Therefore, it is necessary to know your optimal pressure and measure it regularly
Not only a person’s health, but also his life depends on normal blood pressure. Therefore, it is necessary to know your optimal pressure and measure it regularly.
If there is a tendency for low or high blood pressure, you need to consult a doctor who will determine the causes of this pathological condition and draw up an adequate treatment regimen. The popular video in this article will tell you in detail about all types of pressure.
https://youtube.com/watch?v=PXnzCmkJtOY
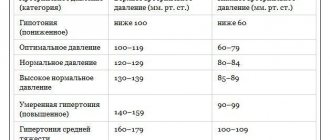
Abnormal blood pressure
Readings above 120/80 are considered abnormal. The table shows the severity levels of high blood pressure.
Stages of High Blood Pressure in Adults
These ranges are for adults with no short-term serious illness.
People with diabetes or chronic kidney disease should stay within 130/80.
Although the elevated blood pressure seen in prehypertension is less than that seen in high blood pressure, prehypertension can progress to hypertension and should be taken seriously. Over time, persistent high blood pressure weakens and damages blood vessels, which can lead to complications.