The term “vasodilation” refers to the dilation of blood vessels that occurs when the smooth muscles of the arteries and large veins relax. Vasodilation occurs naturally in response to low oxygen levels or increased body temperature. The purpose of vasodilation is to increase blood flow and oxygen delivery to the parts of the body that need it.
In certain circumstances, vasodilation can have a beneficial effect on a person's health. For example, doctors sometimes induce vasodilation to treat high blood pressure and related cardiovascular disease. However, vasodilation can also contribute to certain diseases, such as hypotension (low blood pressure) and some chronic inflammatory conditions.
Vasodilation is caused by the following conditions
- pulmonary hypertension, increased blood pressure in the pulmonary circulation
- preeclampsia and eclampsia, which are complications of pregnancy
- heart failure
Your doctor may also stimulate vasodilation to improve the effect of drug or radiation therapy. Vasodilation increases the delivery of drugs or oxygen to the tissues targeted by this treatment.
Symptoms of weakened blood vessels
If similar symptoms are detected, you need to pay close attention to the condition of the blood vessels:
- Fainting and dizziness;
- Throbbing pain in the back of the head or temples, tinnitus;
- Cold and swollen feet;
- Intolerance to hot weather;
- Dependency on weather;
- Depression, insomnia, fatigue;
- Shortness of breath, tachycardia, constantly changing pressure;
- Hematomas even with a small impact;
- Changeable temperature;
- Nosebleeds;
- Spider veins and pinpoint hemorrhages on the skin;
- Tingling, pain and bruising on the eyeball.
Vascular stenosis
Atherosclerosis
Diabetes
Ulcer
4003 12 August
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Vascular stenosis: causes, symptoms, diagnosis and treatment methods.
Definition
Vascular stenosis (Greek στενός - “narrow, cramped”) is a partial or complete persistent narrowing of the lumen of blood vessels with limitation or complete cessation of blood flow.
Causes of vascular stenosis
Depending on which vessels are affected, a distinction is made between stenosis of arterial vessels (aorta, arteries, arterioles) and stenosis of venous vessels (superior vena cava, inferior vena cava, veins, venules).
Vascular stenosis can be either congenital or acquired.
The main cause of acquired stenosis of the aorta, arteries of the lower extremities, and coronary arteries of the heart is atherosclerosis, a systemic metabolic disease with predominant damage to the vascular wall. The degree of narrowing of the artery and its length may vary. When blood pressure increases, the sclerotic inner layer of the vessel (endothelium) is easily damaged, as a result, the blood clotting process is activated and a blood clot is formed.
Blockage of the vessel can lead to ischemia or necrosis of the tissue or organ.
Risk factors for the development of atherosclerosis include:
- male gender;
- elderly age;
- smoking;
- dyslipidemia (violation of the normal ratio of blood lipids);
- diabetes,
- arterial hypertension,
- increased blood homocysteine;
- elevated levels of C-reactive protein (CRP);
- increased blood viscosity and hypercoagulable states;
- chronic renal failure.
Another disease leading to arterial stenosis is obliterating endarteritis (spontaneous gangrene) - a chronic disease of peripheral blood vessels (mainly affecting the arteries of the feet and legs).
Mostly men under the age of 25-40 are affected. Those at risk include smokers, as well as people with frostbite on their feet. Diabetic angiopathy, characterized by damage to both small vessels and large and medium-sized arteries, develops in patients with diabetes mellitus. In diabetic macroangiopathy, when large blood vessels are affected, changes characteristic of obliterating atherosclerosis are found in the wall of the great vessels. With microangiopathies, when small blood vessels are affected, thickening of the walls of microvasculature vessels (arterioles, capillaries, venules) occurs, which leads to a narrowing of the lumen and deterioration of the blood supply to organs and tissues.
Coarctation of the aorta (congenital segmental narrowing of part of the aorta that obstructs blood flow) occurs as a result of improper fusion of the aortic arches in the embryonic period. The length of the narrowing is usually 1-2 cm. The ascending aorta and branches of the aortic arch expand, their diameter increases significantly, and the walls of the arteries participating in the collateral circulation become thinner. Two modes of blood circulation are formed in the systemic circle: up to the point of obstruction to blood flow there is arterial hypertension, and distal (or below) there is hypotension.
Venous stenosis most often occurs as a result of direct damage to the vascular wall during catheter insertion and is then aggravated by the constant presence of a foreign body and mechanical irritation. Inflammation and activation of the blood coagulation system are observed in the vessel wall. These changes lead to proliferation (multiplication) of smooth muscle cells, thickening of the vein wall, and the formation of microthrombi.
Thus, risk factors for the development of central venous stenosis are: the use of a central venous catheter, infections associated with the installation of a catheter, and concomitant diseases.
Systemic vasculitis, tumor diseases and other causes of vascular stenosis are detected much less frequently.
Classification of the disease
According to the type of blood vessels:
- arterial stenosis;
- venous stenosis
Due to the occurrence:
- congenital;
- acquired.
By localization:
- Stenosis of the arteries of the lower extremities.
- Stenosis of the carotid (carotid) and cerebral arteries.
- Stenoses of the arteries of internal organs:
- renal arteries,
- mesenteric arteries etc.
- Aortic stenosis.
- Stenosis of coronary vessels.
By caliber of damage:
- stenosis of large vessels (aorta and its branches);
- stenosis of medium-diameter vessels;
- stenosis of small vessels (arterioles and capillaries).
Symptoms of vascular stenosis
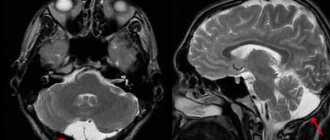
Damage to the blood vessels of the brain is one of the main causes of mortality and disability in the population. 2/3 of ischemic strokes are associated with narrowing and deformation of the carotid arteries.
The risk of developing ischemic stroke is directly related to the degree of narrowing of the artery lumen.
Occlusion (closure) of the internal carotid artery leads to the development of stroke in 40% of cases.
Damages to the blood vessels of the brain can occur in several forms:
- The asymptomatic form is characterized by the absence of focal and cerebral neurological symptoms (impaired consciousness, headache, vomiting, slow pulse).
- Discirculatory encephalopathy is characterized by a predominance of general cerebral symptoms; focal neurological symptoms are absent or appear in a very mild form.
- Transient ischemic attacks manifest themselves in the form of transient disorders of cerebral circulation of the ischemic type and are accompanied by the appearance of focal neurological symptoms that resolve within 24 hours.
- The consequences of a minor stroke are an acute ischemic cerebrovascular accident with the development of neurological symptoms, which almost completely regress within a month as a result of conservative therapy.
- The consequences of a completed stroke are an acute ischemic disorder of cerebral circulation, accompanied by the development of persistent focal neurological and cerebral symptoms.
- Ischemic stroke is damage to brain tissue with disruption of its functions due to obstruction or cessation of blood flow.
Atheroslerotic lesion of the coronary arteries of the heart is manifested by angina pain, but can sometimes be perceived by the patient as discomfort, a feeling of heaviness, compression, tightness, distension, burning or lack of air.
Most often, the pain is localized behind the sternum or along the left edge of the sternum; it can radiate (give) to the neck, lower jaw, teeth, interscapular space, and less often to the elbow or wrist joints, mastoid processes. Pain with angina pectoris usually lasts from 1 to 15 minutes. Occurs during significant physical or emotional stress. After taking nitroglycerin or stopping the exercise, the pain stops. As angina progresses, an attack may occur with minimal exertion and then at rest.
The main symptom of renal artery stenosis is a persistent increase in blood pressure, which is difficult to respond to drug therapy. Approximately 90% of cases of renal artery stenosis are caused by atherosclerosis; in 10% of cases, stenosis occurs due to fibromuscular dysplasia, a group of diseases that affect the walls of the arterial vessel.
With renal artery stenosis, the blood supply to the kidney tissue is reduced, hormonal factors (renin-angiotensin-aldosterone system) that regulate blood volume and blood pressure are activated, and the development of chronic kidney disease is accelerated.
Stenosing damage to the vessels supplying blood to the abdominal organs (mesenteric arteries) is more often observed in middle-aged and elderly people and manifests itself as chronic abdominal ischemia syndrome, so the main complaint of patients is pain, which appears after 20-25 minutes. after eating, lasts 1-2 hours and usually subsides on its own. The pain can be localized in the epigastric region, directly under the xiphoid process, and radiate to the right hypochondrium or spread from the periumbilical region throughout the abdomen. Some patients note a feeling of constant heaviness in the abdomen, and vomiting is rarely observed.
Other symptoms of chronic abdominal ischemia are intestinal dysfunction, expressed by disturbances in its motor, secretory, absorption functions, and progressive weight loss.
Obliterating atherosclerosis of the aorta and main arteries of the lower extremities is more common in men over 40 years of age and deprives them of their ability to work. The process can be localized in large vessels (aorta, iliac arteries) or medium-sized arteries (femoral, popliteal).
Small atherosclerotic lesions of the arteries of the lower extremities may not be clinically manifest. With continued vasoconstriction, intermittent claudication occurs, which is manifested by discomfort or pain in the muscles of the lower limb during physical activity. Damage to the terminal aorta and iliac arteries can cause pain in the buttocks, thigh, and calf. Impaired patency of the femoral-popliteal segment is characterized by pain in the calf. Occlusion of the arteries of the leg usually causes pain in the calf, foot, absence or decrease in skin sensitivity in them.
With obliterating endarteritis, trophic disorders are observed (cracks, dry skin, brittle nails, ulcers), intermittent claudication, leg pain, necrosis and gangrene of the limb.
In the generalized form of obliterating endarteritis or atherosclerosis, not only the vessels of the extremities are affected, but the visceral branches of the abdominal aorta, branches of the aortic arch, cerebral and coronary arteries.
The clinical picture of diabetic macroangiopathy consists of the clinical picture of microangiopathy and atherosclerosis of the great vessels, but is characterized by a more severe and progressive course, often ending in gangrene.
The clinical picture of diabetic microangiopathy of the lower extremities is similar to that of obliterating endarteritis.
With coarctation of the aorta, symptoms depend on the severity of the disease. In the case of significant narrowing of the aorta, the parents of the newborn pay attention to the pale skin, sweating, and difficulty breathing of the child. In older children and adults, the symptoms are usually mild: high blood pressure, headache, cold extremities, nosebleeds.
Stenosis of the central veins is clinically manifested by swelling of the extremities, pain in them and trophic changes (cyanosis, thinning of the skin, cracks, ulcers, etc.).
Diagnosis of vascular stenosis
Diagnosis of the disease is based on the analysis of patient complaints, medical history data, clinical picture, data from laboratory and instrumental research methods.
To clarify the cause of vascular stenosis, the following may be recommended:
- clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes);
How to strengthen blood vessels?
Most doctors suggest that patients not only take medications, but also change their lifestyle. It is worth giving up bad habits (smoking and alcohol), changing your physical activity regime (try not to sit still, but also not overloading yourself with exercise), resting, avoiding nervous shock and sticking to proper nutrition.
Medicines are the main way to correct the condition of blood vessels. With proper treatment, you can achieve good results in strengthening the walls of blood vessels or reduce the risk of problems with them in the future.
What causes vasodilation
- Exercise
: Vasodilation allows extra oxygen and nutrients to be delivered to muscles during exercise. - Alcohol
: Alcohol is a natural vasodilator. Some people report alcohol-induced vasodilation as warmth or redness in their facial skin. - Inflammation
: This is the body's way of repairing damage. Vasodilation promotes inflammation by delivering oxygen and nutrients to damaged tissue. - Naturally occurring chemicals
: The release of certain chemicals in the body can cause blood vessels to dilate. Examples include nitric oxide and carbon dioxide, as well as hormones such as histamine, acetylcholine, and prostaglandins. - Vasodilators
: These are drugs that dilate blood vessels. Doctors sometimes use these drugs to treat hypertension and related conditions.
Vasoconstriction is the opposite of vasodilation. During vasoconstriction, the heart must work harder to force blood through the narrowed veins and arteries. This may lead to increased blood pressure.
Factors that may affect vasodilatation
There are several factors that can affect the diameter of blood vessels.
Temperature
The human body contains nerve cells called thermoreceptors
, which detect temperature changes in the environment. When the environment becomes too warm, thermoreceptors trigger vasodilation. This directs blood flow to the skin, where excess body heat can escape.
Weight
Obese people are more likely to experience changes in vascular reactivity. This can happen when blood vessels do not narrow and dilate as they should. In particular, obese people have blood vessels that are more resistant to vasodilation. This increases the risk of hypertension and related cardiovascular diseases such as heart attack and stroke.
Age
Blood vessels contain receptors called baroreceptors
, which constantly monitor blood pressure and cause vasoconstriction and dilation. As we age, baroreceptors become less sensitive. This may reduce their ability to maintain a constant blood pressure level. Blood vessels also become stiffer and less elastic as we age. This makes them less able to contract and expand as needed.
Height above sea level
Air at high altitudes contains less oxygen. Therefore, a person at high altitude will experience vasodilation as their body tries to maintain oxygen supply to its cells and tissues.
Although vasodilation lowers blood pressure in large blood vessels, it can increase blood pressure in capillaries because small vessels do not dilate in response to increased blood flow.
Increased blood pressure in the capillaries of the brain can cause fluid to leak into the surrounding brain tissue. This leads to local swelling. Medical professionals call this condition altitude sickness. People at high altitudes may also experience constriction of blood vessels in the lungs. This can cause fluid to accumulate in the lungs, which is called high-altitude pulmonary edema. These conditions can be life-threatening if the person does not receive treatment.
Chronic inflammatory conditions
Vasodilation also plays an important role in inflammation. Inflammation is a process that helps protect the body from harmful pathogens and repair damage caused by injury or disease. Vasodilation promotes inflammation by increasing blood flow to damaged cells and tissues in the body. This ensures effective delivery of the immune cells needed for protection and repair. However, chronic inflammation can cause damage to healthy cells and tissue, leading to DNA damage, tissue death, and scarring. Some conditions that can cause inflammation and associated vasodilation include:
- infections
- severe allergic reactions
- chronic inflammatory conditions such as rheumatoid arthritis, inflammatory bowel disease, lupus, and Sjögren's syndrome
Diagnosis of varicose veins:
- Examination and history taking;
- Duplex scanning of veins;
- Ultrasonography;
- Phlebography of the veins of the extremities;
- Phlebomanometry.
After examining the patient, the doctor determines the need for one or another type of vascular diagnostics. When the disease is diagnosed, the patient is offered the following treatment methods for varicose veins:
- Removal of affected veins (phlebectomy)
- Laser photocoagulation;
- Sclerotherapy (with the help of a special substance, damaged veins seem to stick together and disappear);
- Radiofrequency coagulation of veins.
Treatment
Based on the characteristics of the disease, one or another method of treating the aneurysm is selected. In cases where there is no threat to life and health, the patient is recommended only regular observation in combination with the prevention of vascular diseases: first of all, in such cases it is recommended to adhere to a strict diet, lead an active lifestyle with moderate physical activity and completely stop smoking.
If the risk of complications is high, dilated, thinned arteries are treated surgically. The indications for the operation are determined by the doctor. In some cases, open surgery is performed to remove the aneurysm and replace the removed portion of the vessel with an endoprosthesis. Endovascular surgery offers modern and safe ways of surgical treatment. To treat aneurysms, an intravascular type of intervention is used - stenting. The essence of the method is to install a stent graft. A special design excludes the dilated section of the vessel from the general blood flow and prevents further growth of the aneurysm and its rupture. The advantage of stenting is that the intervention is performed without incisions under local anesthesia. Find out about the cost of the operation to install a stent by clicking on the link.
Causes
The causes of vasodilation are hypertension, severe injuries, the last stages of syphilis, atherosclerosis. Moreover, atherosclerosis is the most common of them. The deposition of cholesterol with the formation of plaques in the walls of the arteries causes the causes of vascular atherosclerosis. Because of this, the elasticity of the blood vessels decreases, the walls become weakened. Under the influence of blood pressure, they stratify and aneurysms form. They not only interfere with the normal blood supply to organs: rupture of an aneurysm is extremely dangerous due to the threat of hemorrhage.