Find out more about other pathologies starting with the letter “D”: Debility, Double-wave viral meningoencephalitis, Dementia with Lewy bodies, Depressive neurosis, Dermal sinus, Cerebral palsy, Jacksonian epilepsy, Diastematomyelia (diplomyelia), Discogenic myelopathy, Dystrophic myotonia Rossolimo-Steinert-Kurshman , Diabetic encephalopathy, Dyscirculatory encephalopathy, Diffuse axonal damage to the brain, Benign rolandic epilepsy.
Discirculatory encephalopathy: the danger of pathology and treatment methods
This pathology is a brain lesion that occurs due to constant progressive circulatory disorders of the central nervous system of various etiologies. It affects motor, emotional and cognitive function, and depending on the severity of the symptomatic picture is divided into three stages. To make and confirm the diagnosis, ultrasound, echo-EG, EEG, REG, duplex scanning of cerebral vessels, ophthalmoscopy, MRI are required. Therapy is selected individually and consists of neuroprotective, antiplatelet, antihypertensive, vascular and other drugs.
What is hidden under the mask of DEP?
Many patients with Alzheimer's disease (AD) are observed for a long time in the clinic with a diagnosis of DEP/CHI, without receiving adequate treatment. AD in our country is poorly diagnosed; patients are often observed with an erroneous diagnosis of chronic vascular lesions of the brain, even in cases of classic manifestations of the disease [Parfenov V.A. et al., 2014].
Absolutely all patients diagnosed with DEP require examination of cognitive functions, and in cases where the amnestic nature of cognitive disorders is detected, the neurodegenerative nature of the disease becomes probable (or a mixed nature: vascular disease + neurodegenerative process), therefore examination in a specialized center is required. As an example, we present 2 clinical cases.
Clinical case No. 1. DEP and BA
Patient N. , 69 years old , was brought to the clinic by relatives, with their complaints of progressive memory loss over three years. Three years ago, the husband began to notice the patient’s memory deterioration and speech impairment increasing over time (“she began to forget the names of some household items, had difficulty choosing the right words in a conversation”), and over the past two years she has not gone to the store because she has difficulty carried out financial calculations. A few weeks ago I couldn’t recognize my sister and niece, which was the reason for going to the doctor.
The patient’s condition at the place of residence was assessed as “discirculatory encephalopathy of the II degree. Cerebral atherosclerosis." However, no neuropsychological study was performed. Elevated blood pressure values (150-160/90-100 mm Hg) were recorded several times, but the patient did not seek medical help for this and did not take antihypertensive drugs.
A somatic examination revealed no significant pathology. The neurological status showed moderately pronounced reflexes of oral automatism and damage to the cranial nerves; no paresis or other neurological disorders were detected.
Brief Mental Status Rating Scale - 4 points, Frontal Dysfunction Battery - 2 points, Clock Drawing Test - 2 points, during the Symbolic Numerical Coding Test she was able to correctly indicate 2 digits in 1.5 minutes. Memorizing words is extremely difficult. When talking with the patient, attention is drawn to a decrease in speech fluency and pronounced elements of agnosia; when naming the objects being shown (the hammer), he says the following: “I don’t know for sure... but it’s probably intended for the household, I think.” Cannot correctly name the time of year or his age.
A CT scan of the brain revealed bilateral atrophy of the temporal lobes and hippocampi with an accent on the left. The results of duplex scanning revealed no stenosis or blockage of the carotid, vertebral or subclavian arteries. The patient was examined by a cardiologist who prescribed antihypertensive drugs. Antidementia drugs galantamine 12 mg/day and memantine 20 mg/day were prescribed. Repeated examinations after 3 and 6 months did not reveal significant changes in neuropsychological tests.
Thus, in our country there is a low level of diagnosis of AD; the majority of patients with AD are diagnosed with DEP or CCI, when cognitive impairment in most cases is caused precisely by a neurodegenerative process (AD) or its combination with cerebrovascular disease, and much less often have pure vascular genesis (vascular cognitive disorders).
Clinical case No. 2. DEP and depression
Patient K., 63 years old , was seen by a neurologist with complaints of headaches, non-systemic dizziness, and sleep disturbances. The patient actively complained of loss of appetite (loss of body weight by 2-3 kg per month), fear of losing consciousness in a public place, fear of sudden death, and being alone at home for a long time. The patient avoided using the elevator. A thorough survey revealed complaints of bad mood, low self-esteem, irritability, fear of the future, blaming oneself for the inability to cope with what is happening, loss of interest in life, back pain, decreased concentration, due to which “nothing can be completed.” " The above symptoms were pronounced in the first half of the day, especially in the morning, and decreased somewhat in the evening.
The patient has been suffering from hypertension for a long time, periodically consulted various specialists on an outpatient basis (therapists, neurologists, cardiologists, otorhinolaryngologists), was treated with a diagnosis of stage II DEP with astheno-neurotic disorders and vestibulopathy; chronic vertebrobasilar insufficiency against the background of cervical osteochondrosis. Treatment included the prescription of betahistine, cinnarizine, afobazole, and he received diclofenac injections in courses; no lasting improvement was noted during the treatment. He was very concerned about his health and independently studied medical literature. An objective examination revealed no somatic pathology; blood pressure was 145/100 mm Hg. Art. A neuropsychological examination did not reveal any abnormalities: brief mental status assessment scale – 30 points, battery of tests for identifying frontal dysfunction – 18 points, clock drawing test – 10 points. No changes were noted in the neurological status. Tests for positional nystagmus and the Halmagi-Kerthoys test are negative. Duplex scanning of extra- and intracranial arteries without local changes in hemodynamics. MRI of the brain showed signs of moderate external replacement hydrocephalus.
Taking into account the peculiarities of the clinical picture, the absence of somatic and neurological disorders allowed us to assume that this patient had a depressive disorder. The patient was referred for consultation to a psychiatrist, who diagnosed a depressive episode of moderate severity with somatic symptoms. Supportive psychotherapy was conducted, aimed at explaining the mechanisms of existing disorders (psychoeducation), coping with neurosis-like symptoms and improving interpersonal interaction. It is recommended to take sertraline at an initial dose of 25 mg/day, followed by an increase to 100 mg/day during the 1st week and up to 150 mg/day at the end of the 1st month. During the treatment, the patient noted a significant improvement in well-being in the form of improved mood, increased daily activity, decreased intensity and decreased frequency of headaches. Observation of the patient for 3 months showed a lasting effect from the treatment.
Anxiety and depressive disorders can be a manifestation of both chronic CVD and psychogenic emotional disorders. Today, a significant proportion of patients suffering from psychogenic anxiety and depressive disorders are erroneously diagnosed with DEP/CHI without receiving adequate treatment. Effective drug and non-drug therapy for anxiety and depressive disorders helps most patients, both with and without chronic CVD.
Source: Parfenov V.A. Dyscirculatory encephalopathy and vascular cognitive disorders. – M.: IMA-PRESS, 2021. – 128 p.: 12 ill.
Causes
The main reason for its appearance is chronic cerebral ischemia caused by various vascular disorders:
- About 60% of cases of DEP are caused by atherosclerotic changes in the walls of cerebral vessels;
- Arterial hypertension ranks second in the list of causes. It can be observed in a number of pathologies: chronic glomerulonephritis, hypertension, polycystic kidney disease, Itsenko-Cushing's disease, pheochromocytoma, etc.
- Hypertension provokes encephalopathy due to the occurrence of vasospasm of the central nervous system, leading to depletion of blood flow;
- Pathology of the vertebral arteries can also cause the disease, as it is responsible for 30% of cerebral circulation. If the primary disease is instability of the cervical spine of a dysplastic nature, osteochondrosis, Kimerli's anomaly, developmental defects or previous spinal trauma, a symptomatic picture of circulatory disorders in the vertebrobasilar region is observed;
- DEP often occurs as a concomitant disease with diabetic microangiopathy. If, with diabetes, the patient is unable to adjust the blood glucose level to the upper limits of normal.
Also, the causes of dyscirculatory encephalopathy can be:
- Chronic or persistent hypotension;
- Arrhythmia;
- Hereditary angiopathy;
- Traumatic brain injuries;
- Systemic vasculitis.
Examination and treatment
Discirculatory encephalopathy
is a neurological disease with slow progression. It is characterized by a lack of blood supply to the blood vessels of the brain. As a result, its functions are disrupted in the area of the affected lesions. The disease occurs in both elderly and young patients. The sooner treatment is started, the higher the chances of full recovery.
Get diagnosed with disculatory encephalopathy at Clinic No. 1:
- MRI
- Consultation with an ophthalmologist
- EEG, REG
- Ultrasound of vessels
- Duplex scanning
For one-time payment for services - 20% discount
Call
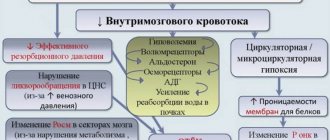
The mechanism of pathology development
The pathogenesis of dyscirculatory encephalopathy includes factors leading to deterioration of cerebral circulation, consequently to hypoxia and disruption of trophism of cells of the central nervous system. This leads to cell death and the appearance of areas of rarefaction of brain tissue, that is, leukoaraiosis or silent infarctions - multiple small lesions.
The subcortical structures and white matter of the deep parts of the brain are most susceptible to destruction during DEP. This is due to their location on the border of the carotid and vertebrobasilar basins. Chronic ischemia provokes the phenomenon of disconnection, that is, disruption of connections between the cerebral cortex and subcortical ganglia. Experts believe that this is the main pathogenetic mechanism. It causes a characteristic symptomatic picture:
- Violation of the emotional sphere;
- Cognitive disorders;
- Pathologies of motor functions.
A distinctive feature of DEP is the reversibility of functional disorders at the first stage of the disease with appropriate treatment and the persistent nature of neurological defects leading to disability at later stages.
General information
Encephalopathy occurs due to metabolic disorders in brain cells. Regardless of the cause, the pathology follows a single scenario. First, there is a decrease in the activity of neurons, then their gradual death. Foci of dystrophy are located throughout the brain, which causes a variety of symptoms.
The damage is irreversible, but with timely consultation with a specialist and quality treatment, the patient’s condition can improve. The remaining intact neurons partially take over the function of the dead cells, and brain function is significantly improved. If the disease was caught at an early stage, the patient retains complete clarity of mind.
Make an appointment
Classification of dyscirculatory encephalopathy
DEP is distinguished by etiology:
- Atherosclerotic;
- Hypertensive;
- Venous;
- Mixed.
According to the speed of development, it can be rapidly progressing or galloping and slowly developing, that is, the classic form.
The severity classification is as follows:
- The first stage is accompanied by subjective feelings of ill-being, mild cognitive impairment, and preservation of the neurological status;
- The second stage is characterized by obvious motor and cognitive disorders and increased emotional distress.
- The third stage is considered the most severe, at which mental disorders begin. It represents vascular dementia of varying severity.
Early symptoms
DEP begins unnoticeably and develops quite slowly. First of all, problems in the emotional sphere are noted. About 65% of patients suffer from depression, which, unlike depressive neurosis, occurs against the background of minor traumatic situations, while patients are not inclined to note depression and low mood. They are fixed on various somatic disorders, like patients with hypochondriacal neurosis. Complaints may include:
- Arthralgia;
- Back pain;
- Neuralgia;
- Noise in the head;
- Tinnitus;
- Pain of various localizations.
Their distinctive feature is that they do not fit into the clinical picture of supposed somatic pathologies. Depression in DEP is difficult to respond to psychocorrection and treatment with antidepressants.
The initial stage of DEP often manifests itself in increased emotional lability, which includes:
- Sudden mood swings;
- Cases of uncontrollable crying for minor reasons;
- Irritability;
- Attacks of aggressive behavior towards others.
In addition, sleep disturbances, fatigue, headaches, and absent-mindedness are noted. The symptomatic picture is similar to neurasthenia, but with dyscirculatory encephalopathy the symptoms are combined with cognitive impairment.
Moreover, in 90% of patients, cognitive impairment occurs at the initial stage of the disease. These include:
- Decreased concentration;
- Memory impairment;
- Reduced speed of thinking;
- Difficulties in planning activities;
- Fatigue with mental effort;
- Problems with speech reproduction of information while maintaining memory.
Movement disturbances, such as dizziness and unsteadiness when walking, may also occur. DEP must be differentiated from vestibular ataxia, since nausea and vomiting may be present, but only during walking.
Symptoms
Stage 1
Characterized by a gradual onset and chronic course. Emotional disturbances are often the most noticeable in the beginning. In 65% of cases, depressive symptoms reminiscent of hypochondriacal neurosis are detected. Complaints of depression and decreased mood are usually absent; unpleasant somatic sensations come to the fore: headache, noise and ringing in the head, pain in the back and joints.
Differences from neurotic depression are the absence of a provoking traumatic situation, the low effectiveness of psychotherapy and antidepressants. In adults, the symptom that determines the picture of the disease is sometimes emotional lability: attacks of aggression or causeless crying, sudden changes in mood, increased irritability. The clinic is complemented by absent-mindedness, deterioration of sleep and fatigue.
In 90% of patients, cognitive impairment occurs at the initial stage. The ability to concentrate and plan actions decreases. Memory deteriorates, thinking slows down. In the motor sphere, dizziness and slight instability when walking are sometimes detected, which are the first signs of vestibulopathy.
Stages 2 and 3
When moving from grade 1 to grade 2, motor and cognitive dysfunction worsens. Due to amnesia, decreased attention and intelligence, usual mental work becomes unbearable. A decrease in criticism and the ability to navigate in place and time arise and gradually worsen. At stage 3, behavior and personality suffer. Due to dementia, patients lose their ability to work, and in severe cases, their ability to self-care.
Apathy prevails. People are not interested in anything, do nothing or do something unproductive, and show indifference to the world around them. Movement disorders become more pronounced and noticeable from the outside. A shuffling gait is formed in small steps without lifting the foot off the floor. Patients with vestibulo-atactic syndrome have progressive balance disorders.
Signs of transition to stage 3 are severe speech problems, paresis, trembling of the limbs, urinary incontinence and pseudobulbar syndrome. Some patients develop symptomatic epilepsy. Due to unsteady gait, people fall, resulting in fractures. Women especially often suffer from injuries, which is due to the prevalence of osteoporosis during menopause.
Clinical picture at stage II-III
In subsequent stages, the clinical picture grows and intensifies: memory deteriorates significantly, attentiveness and intelligence decrease, and difficulties are noted when performing habitual mental work. Patients are unable to adequately assess their own condition and tend to overestimate their performance and intelligence. Over time, the ability to develop a program of action, generalization, and orientation in time and space is lost. At the third stage, disturbances in praxis and thinking are noticeable. Personality and behavior disorder occurs. Dementia is noted, in which patients lose the ability to work, and in more severe cases, self-care skills.
The emotional stage is dominated by apathy, loss of interest in previous hobbies, and lack of motivation. At the third stage, patients do nothing or are engaged in unproductive activities. They are indifferent to themselves and their surroundings.
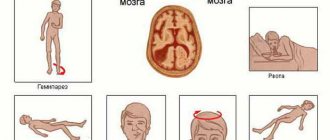
If at the first stage motor disorders are weakly expressed, then at later stages these disorders are visible to others. Typical manifestations are:
- Slow gait in small steps;
- Shuffling;
- Falls when walking or turning, which are often accompanied by fractures, especially if the patient suffers from osteoporosis;
- Difficulty starting or stopping in time.
Clinical manifestations, especially the characteristic “skier’s gait,” are similar to the symptoms of Parkinson’s disease, but are not accompanied by abnormalities in the arms, so experts call such signs of DEP “vascular parkinsonism” or “lower body parkinsonism.” Also, the last stage is accompanied by:
- Urinary incontinence;
- Pseudobulbar syndrome;
- Paresis;
- Tremor;
- Severe aphasia;
- Symptoms of oral automatism.
Epileptic seizures may occur.
Treatment
Therapy is carried out comprehensively, procedures are selected individually for each patient. Patients at stage 2 of DEP often forget about appointments, so to achieve results they cannot do without the help of loved ones. Responsible adherence to recommendations can show good results and improvements in the patient’s condition within a few months.
1. Non-drug therapy
Physiotherapy can be quite effective in treating encephalopathy. Based on the causes of the syndrome and general health, patients are prescribed the following procedures: UHF and laser therapy, electrosleep and galvanic currents. Sometimes non-traditional approaches are used, such as acupuncture.
The following will also help improve the patient’s condition:
- regular long stay in the fresh air;
- getting rid of stressful situations;
- the presence of simple physical activity agreed upon with the doctor (however, serious physical activity and heavy lifting must be avoided);
- daily therapeutic exercises;
- giving up alcohol and smoking;
- if your weight exceeds the norm, it is recommended to lose weight.
2. Treatment with medications
The doctor individually selects appropriate medications depending on the form and symptoms of the disease. Dyscirculatory encephalopathy in people with hypertension requires the use of medications to normalize blood pressure. If a patient has vascular atherosclerosis, the doctor prescribes therapy that helps clean the blood channels and get rid of cholesterol plaques. The treatment complex for stage 2 dyscirculatory encephalopathy may include the necessary vitamins, sedatives, antidepressants and nootropics.
3. Diet therapy
If you follow a proper diet, you can also get good results. The patient should exclude from the diet foods that lead to nervous tension and decreased vascular functionality: fried, fatty, spicy foods, alcohol and energy drinks, processed foods and dishes with preservatives, dyes, chemical additives, coffee and soda. When creating a meal plan, it is recommended to choose fresh fruits and vegetables, garlic and onions, white meat and fish, as well as other light dishes that do not overload the body.
Methods for diagnosing DEP
It is very important to make a diagnosis as early as possible in order to promptly begin vascular therapy to compensate for neurological disorders. Therefore, all patients at risk for discirculatory encephalopathy must be regularly examined by a neurologist. The risk group includes:
- People suffering from atherosclerosis;
- Diabetics;
- Hypertensive patients;
- Aged people.
To identify cognitive impairment, special tests are required. Tasks may include the need to remember and repeat a list of words named by the doctor, draw a dial with a given time, or repeat certain words.
In addition, consultation with an ophthalmologist and ophthalmoscopy, determination of visual fields, will be required. The following hardware diagnostic methods are shown:
- Echo-EG;
- EEG;
- REG;
- ECG and daily ECG monitoring;
- Doppler ultrasound of head and neck vessels;
- MRA of cerebral vessels;
- Duplex scanning;
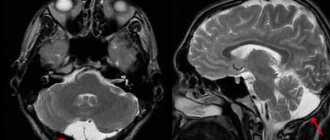
- MRI of the brain.
MRI of the brain will help distinguish DEP from other pathologies: Alzheimer's disease, Creutzfeldt-Jakob disease, disseminated encephalomyelitis. Magnetic resonance imaging makes it possible to visualize foci of silent infarctions, while areas of leukoaraiosis and cerebral atrophy also occur in other neurodegenerative pathologies.
To detect etiological factors, consultation with a cardiologist and nephrologist, blood pressure monitoring, a coagulogram, determination of lipoproteins and cholesterol in the blood, and a blood sugar test are required.
Diagnostics
A neurologist is involved in the diagnosis and treatment of encephalopathy. Patient examination includes:
- survey: collection of complaints and anamnesis; it is mandatory to clarify information about previous diseases, injuries, risk factors, the time of the first violations, the rate of development, etc.;
- neurological examination: assessment of reflexes, sensitivity, muscle strength, motor function;
- electroencephalography (EEG): assessment of electrical impulses arising during brain function; allows you to identify signs of epilepsy, inflammation, the presence of tumors, etc.;
- Doppler ultrasound of the vessels of the brain and neck: assesses the quality of blood flow in large vessels, identifies areas of narrowing, assesses the volume of incoming blood;
- rheoencephalography: complements ultrasound, allows you to assess the tone and elasticity of blood vessels, detect blood clots;
- angiography: X-ray examination of blood vessels by introducing a contrast agent into them;
- CT and MRI: allow you to detect foci of sclerosis, tumors, inflammatory foci, consequences of stroke and other structural changes;
- blood tests (general, biochemical): make it possible to evaluate the functioning of the kidneys, liver, pancreas, and identify toxins that can affect the condition of the brain.
If necessary, other tests and examinations may be prescribed, as well as specialist consultations to accurately determine the cause of encephalopathy.
Make an appointment
Therapy
The therapeutic approach to the treatment of encephalopathy should have an etiopathogenetic direction and be comprehensive. It is necessary to compensate for the primary disease, enhance microcirculation and cerebral circulation, and also protect the cells of the central nervous system from ischemia and hypoxia.
Etiotropic treatment of DEP includes the selection of hypoglycemic and antihypertensive drugs, which should be prescribed individually. An anti-sclerotic diet is also indicated. If cholesterol levels do not decrease even with dietary correction, appropriate medications are prescribed, such as gemfibrozil, lovastatin, probucol.
The basis of pathogenetic therapy is drugs that improve cerebral hemodynamics. It is important that they do not lead to the effect of stealing. These are calcium channel blockers such as flunarizine, nifedipine, nimodipine, as well as α2-adrenergic receptor antagonists, such as nicergoline or pyrobedil, and phosphodiesterase inhibitors: ginkgo biloba, pentoxifylline. Since DEP is often accompanied by increased platelet production, the patient needs lifelong use of antiplatelet agents, which include ticlopidine or acetylsalicylic acid. If the patient has contraindications, such as gastrointestinal bleeding or stomach ulcers, dipyridamole may be prescribed.
It is very important to take drugs with a neuroprotective effect, which allow neurons to function under conditions of chronic hypoxia. These include:
- Piracetam;
- GABA derivatives: gamma-aminobutyric acid, aminophenylbutyric acid, N-nicotinoyl-gamma-aminobutyric acid;
- Membrane stabilizing drugs: choline alfoscerate;
- Cofactors;
- Medicines of animal origin: porcine cerebral hydrolysate, hemodialysate from the blood of dairy calves, cortexin;
- Vitamin and mineral complexes.
If discirculatory encephalopathy is caused by a narrowing of the lumen of the internal carotid artery reaching seventy percent, it usually progresses very quickly and is accompanied by small strokes or episodes of PNMK. In such a situation, surgical intervention is indicated. It could be:
- Carotid endarterectomy for stenosis;
- Extra-intracranial anastomosis with complete occlusion;
- Reconstruction of the vertebral artery in case of damage.
The use of "Semax 0.1%" for dyscirculatory encephalopathy:
- ensures the survival of neurons and forms new interneuronal connections even under conditions of chronic hypoxia during DE;
- supports the functionality of nervous tissue;
- increases mental and physical performance;
- restores cognitive functions;
- improves memory and concentration;
- normalizes the work of vegetative centers;
- improves memory and concentration;
"Semax 0.1%" fights not only the symptoms, but also the causes of the disease, successfully defeating them.
Doctor's forecasts
With effective and timely therapy, the development of DEP at the first or second stage in most cases slows down. Occasionally, rapid development of the disease is observed, in which case each stage takes about two years. When dyscirculatory encephalopathy is combined with degenerative changes in the central nervous system, the prognosis is most often unfavorable. Hypertensive crises, ischemic or hemorrhagic strokes, TIA and other cerebrovascular accidents, and uncontrolled hypoglycemia that accompany the disease have a negative impact on the recovery process.
Prevention
Encephalopathy is a complex disease. There is no clear method to prevent its occurrence and eliminate all risk factors. Doctors recommend adhering to the following rules:
- provide yourself with a full daily routine with alternating work and rest, a full night’s sleep;
- minimize stress;
- eat properly and balanced, avoid overeating and excess body weight;
- ensure sufficient supply of vitamins and microelements;
- quit smoking, drugs, alcohol;
- exercise in moderation (not professionally);
- promptly identify and treat chronic diseases: hypertension, diabetes, atherosclerosis;
- consult a doctor at the first signs of trouble.