Content:
- Causes of the disease
- How does alcoholic liver hepatitis occur?
- Classification varieties
- Symptoms
- Diagnostics
- Treatment
In addition to its intoxicating effect, alcohol has a pronounced toxic effect on the human body. Alcohol affects almost all organs. The brain is destroyed the most and fastest, but the liver gets a “double” blow. Its anatomical structural units - hepatocytes - not only suffer and undergo destruction, but are also forced to neutralize ethanol, decomposing it into safe compounds. Therefore, one of the most common and dangerous complications of drunkenness is alcoholic hepatitis. This disease leads to inflammatory changes in tissue. Subsequently, fatty degeneration develops. Its outcome is fibrosis, which gradually turns into cirrhosis - the replacement of cells with connective tissue, which becomes a causative factor in the complete loss of its main functions.
Features of women's lesions
More severe and rapid liver damage in women is explained by:
- A physiological feature of the composition of gastric juice in the female body is that women have significantly less production and content of the enzyme alcohol dehydrogenase than men, therefore, ethanol is not broken down in the stomach, enters the liver in massive quantities and represents a significant burden.
- A larger mass of adipose tissue in the body and a smaller mass of water, which leads to a lack of dilution of ethanol, increases its toxicity. Fats in the liver parenchyma enhance oxidative reactions, promote rapid inflammation and outcome in fibrosis.
- An imbalance of estrogen during menopause, which negatively affects alcohol intoxication.
All factors indicate a significant reduction in time of alcohol abuse for women compared with men for the same liver damage
Treatment of alcoholic hepatitis requires taking into account gender characteristics and their correction.
Causes of the disease
The disease is formed as a result of prolonged abuse of alcoholic beverages, especially surrogates. The speed of its development is determined by the doses taken, the strength and quality of the alcohol. The individual characteristics of the drinker’s body are of no small importance. Usually, after 5-7 years of regular drinking, serious complications appear. The pathology develops most quickly in persons with congenital deficiency of enzymes that neutralize ethanol and in weakened patients.
How does alcoholic liver hepatitis occur?
Once in the stomach, alcohol is absorbed into the blood vessels and carried by the bloodstream throughout the body, exerting its toxic effect. The only “filter” that protects all systems from its toxic influence is the liver. Alcohol catabolism occurs in hepatocytes.
There are 3 main pathways involved in its oxidation:
- With the participation of the enzyme alcohol dehydrogenase (ADH).
- Against the background of a microsomal ethanol oxidation reaction.
- With the help of catalase.
Option 1 is the most important. All three systems function thanks to hepatocytes. As a result of their effect on alcohol, acetaldehyde is formed - a poisonous alcohol catabolite. Hepatic dehydrogenases take part in its accelerated breakdown.
Chronic consumption of large doses of alcohol causes cell damage. They lose their protective properties, and poisons begin to quickly destroy all organs. An inflammatory process occurs in the liver.
Inflammation provokes:
- Increase in organ volume.
- Impaired performance.
- Edema.
- Soreness.
Against this background, the entire biochemical cell cycle in hepatocytes is disrupted, hypoxia occurs and their death occurs. The inflammatory reaction becomes diffuse.
Consequences and complications
Severe complications occur with liver cirrhosis. Among them it is worth highlighting:
- Variceal bleeding due to portal hypertension .
- Hepatic encephalopathy.
- Ascites.
- Infection. This is a common complication in severe hepatitis and cirrhosis . The most common causes are spontaneous bacterial peritonitis , bacteremia , respiratory infection, and urinary tract infections.
- Hepatorenal syndrome . This is the development of renal failure with severe impairment of liver function.
- Hepatocellular carcinoma.
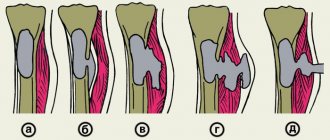
Classification varieties
Alcoholic hepatitis has many different course options. It is important for doctors to consider a number of main characteristics when choosing treatment tactics.
On this basis, they distinguish 2 main types along the flow:
- Persistent. This form is characterized by a stable character and reversible development, provided that a sober lifestyle is maintained.
- Progressive. This process is characterized by a rapid increase in symptoms, cell destruction and organ damage (fine-focal necrosis with transition to cirrhotic changes).
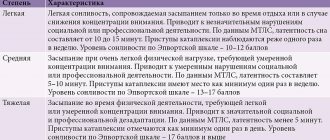
Stages of the disease:
- Easy.
- Average.
- Heavy.
The disease has phases:
- Acute – more pronounced and fast-flowing.
- Chronic, characterized by a sluggish course with periodic exacerbations.
Risk factors
For the occurrence of hepatitis in the liver against the background of alcohol abuse, the following are important:
- malnutrition (deficiency of fruits and vegetables, meat products);
- treatment with hepatotoxic drugs and herbs (for example, St. John's wort should be taken according to its name);
- infection by viruses with a predominant effect on liver cells;
- lack of immunity;
- genetic predisposition in the form of inhibition of the synthesis of the necessary set of enzymes.
The clinical course of alcoholic hepatitis is associated with a combination of all of these factors. Depending on the duration and symptomatic complex of the lesion, it is customary to distinguish between acute and chronic forms.
Symptoms
The symptoms of alcoholic hepatitis depend on the stage and severity of the process.
According to clinical manifestations, the following forms are distinguished:
- Latent.
- Jaundice.
- Cholestatic.
- Fulminant.
Latent manifests itself:
- Unpleasant sensations in the right hypochondrium.
- Periodic nausea, decreased appetite.
- An increase in the content of transaminases in a biochemical blood test.
Jaundice (the most common) is characterized by:
- Constant weakness.
- Loss of appetite.
- Pain in the liver area.
- Loss of body weight.
- Dyspeptic disorders, diarrhea, often nausea and vomiting.
- Yellowness of the skin and sclera.
- Prolonged low-grade fever.
- Liver pain on palpation.
In the advanced stage, an enlarged spleen, fluid in the abdominal cavity, redness of the palms, and telangiectasia (a network of dilated small vessels on the skin) appear. These signs indicate the beginning of the cirrhotic process.
The cholestatic variant is characterized by:
- Severe skin itching.
- Discolored stool.
- Obvious jaundice.
- Dark colored urine.
This type of pathology is less common and has a protracted course.
The fulminant form occurs with the following symptoms:
- Heavy current.
- Rapid onset of liver failure.
- Hemorrhagic syndrome.
- Rapid development of coma.
Chronic alcoholic hepatitis occurs with moderate complaints and minor changes in laboratory tests.
Diagnostics
At a diagnostic appointment, the specialist carefully examines and interviews the client and/or his relatives.
The doctor pays attention to the presence of external signs of alcoholism and complications:
- Puffy face.
- Degradation.
- Trembling in hands.
- Muscle atrophy.
- The presence of Dupuytren's contracture is a fibrous degeneration of the tendons of the hand.
- Damage to the heart and nervous system.
All these signs indirectly indicate the presence of pathological malfunctions in the liver. When identifying a disease, doctors often encounter difficulties. Especially when it comes to the initial stages of the disease. In this case, the specialist is alarmed by deviations in the biochemical composition of the blood.
- Patients are diagnosed with:
- Leukocytosis is an increased content of leukocytes, indicating an acute course of a painful disorder.
- Leukopenia is a decrease in the level of white blood cells, characteristic of toxic damage to the red bone marrow.
- Anemia caused by vitamin B12 deficiency.
- Acceleration of ESR.
- High levels of hepatic transferases - ALT and AST.
In addition to examination, questioning and palpation, the narcologist prescribes ultrasound and MRI.
Ultrasound examination reveals:
- Increased organ size.
- Heterogeneity of structure.
- Increased echogenicity.
Magnetic resonance imaging reveals:
- Stagnation of blood in the portal vein system.
- An extensive network of collateral circulation (due to increased pressure in the hepatic vessels).
- Damage to the pancreas.
Treatment
Healing alcoholic hepatitis requires an integrated approach.
The doctor needs:
- Eliminate the main cause of the disease – alcohol abuse. The patient must undergo basic therapy for alcoholism, drug treatment for its consequences, psychotherapy and coding. A regime of absolute sobriety is the most necessary condition for recovery.
- Choose a suitable diet for the patient.
- Prescribe medication.
For mild forms of inflammatory changes in the liver, it is quite enough to simply give up alcohol. The pathogenic process in most cases will reverse.
In more severe situations, pharmacotherapy is required, consisting of:
- Infusion-drop therapy with accelerated neutralization of toxins and facilitating the work of liver cells.
- Introduction of amino acids that reduce pathological protein catabolism and destruction of protein reserves, improving brain function.
- Prescription of hepatoprotectors, especially those based on essential phospholipids. They effectively reduce fatty degeneration of tissues and have a pronounced antioxidant effect. By causing organ regeneration, they promote more effective healing.
- Taking cytoprotectors.
- Vitamin therapy. A sick body needs pyridoxine, thiamine, cyanocobalamin and riboflavin.
In the most severe cases, patients are given hormonal therapy with glucorticosteroids, plasma substitutes and interferons are prescribed to prevent the formation of fibrosis.
Dietary food should contain a sufficient amount of vitamins and unsaturated fatty acids.
The prognosis of alcoholic hepatitis depends on the clinical form of the pathology and the patient’s behavior. With the help of modern drugs, it is possible to cure or stop the pathological process even in serious stages of the disease. But if a person continues to drink alcohol, then sooner or later he will develop cirrhosis. There is a high probability of developing hepatocellular carcinoma (malignant degeneration). In both cases, the prognosis for life is unfavorable.
Diet
Diet 5th table
- Efficacy: therapeutic effect after 14 days
- Duration: from 3 months or more
- Cost of products: 1200 - 1350 rubles per week
Diet for hepatitis
- Efficacy: therapeutic effect after a week
- Terms: 6 months or more
- Cost of products: 1400-1450 rubles per week
Diet for liver cirrhosis
- Efficacy: therapeutic effect after 3-4 months
- Terms: lifelong
- Cost of products: 1600-1800 rubles. in Week
For all liver diseases, diet Table No. 5 . In the stage of cirrhosis, when the patient has insufficient protein-forming function of the liver, it is necessary to monitor the intake of protein in the body and maintain it in the amount of 1.2-1.5 g per kg of weight. The main thing is that the patient has a normal energy value of food (at least 2000 kcal) and a sufficient amount of vitamins (group B and folic acid). Patients should be given multiple meals with light snacks during the day and at night.
- Increase the content of foods that provide essential nutrients.
- In case of decompensated cirrhosis with encephalopathy , protein intake should be limited, and in case of ascites , unsalted food is recommended.
- Use nutritional mixtures (orally) for energy malnutrition.
- Use of whole protein mixtures.
- For hepatic encephalopathy - mixtures based on branched chain amino acids (so-called BCAA amino acids).
- For ascites - concentrated and high-calorie mixtures.
- For anorexia, they switch to enteral tube feeding.
- For hyperammonemia, Hepasol A is a special agent for parenteral nutrition.
Literature:
- Scheme of differential diagnosis of alcoholic and viral hepatitis [Text]: (Methodological recommendations) / Ministry of Health of the USSR; [Comp. Lebedev S.P., Mukhin A.S., Potekaeva M.A. and etc.]. — Moscow: b. i., 1979. - 8 p.
- Alcoholic liver disease: method. recommendations / Military medical. acad. them. CM. Kirov
- 2004 (State Unitary Enterprise of the Republic of Kazakhstan Republic, type. P.F. Anokhin).
- Differentiated approach to the management of patients with alcoholic hepatitis: abstract of thesis. ... Candidate of Medical Sciences: 01/14/28 / Komkova Inna Igorevna; [Place of protection: First Moscow. state honey. univ. them. THEM. Sechenov]. - Moscow, 2013. - 24 p.
The text was checked by expert doctors: Head of the socio-psychological service of the Alkoklinik MC, psychologist Yu.P. Baranova, L.A. Serova, a psychiatrist-narcologist.
CAN'T FIND THE ANSWER?
Consult a specialist
Or call: +7 (495) 798-30-80
Call! We work around the clock!