The first Danilovsky multidisciplinary medical center on Avtozavodskaya provides treatment for all types of hepatitis. At the clinic you can undergo laboratory diagnostics, have an ultrasound of the liver and receive personal therapy from doctors of the highest category.
Hepatitis D has several development options:
- co-infection (the disease occurs together with hepatitis B);
– superinfection (superimposed on the hepatitis B virus).
Key Facts
- Hepatitis D virus is a virus that requires the presence of hepatitis B virus to replicate. Hepatitis D virus infection occurs either simultaneously with hepatitis B virus infection (coinfection) or after hepatitis B virus infection (superinfection).
- Globally, nearly 5% of all people with chronic hepatitis B are infected with the hepatitis D virus; The hepatitis D virus is transmitted through the blood or other body fluids of infected people.
- There are several pockets of high prevalence of hepatitis D, including in Mongolia, the Republic of Moldova and several countries in West and Central Africa.
- Groups at high risk of co-infection with hepatitis B and D viruses include indigenous peoples, hemodialysis patients and people who inject drugs.
- Since the 1980s, there has been a decline in the overall incidence of hepatitis D worldwide. This trend is mainly due to the success of the global hepatitis B vaccination program.
- Coinfection with hepatitis D and hepatitis B viruses is considered the most severe form of chronic viral hepatitis due to the more rapid progression of fatal liver failure or hepatocellular carcinoma.
- To date, treatment success rates for this form of infection are generally low.
- Hepatitis D infection can be prevented through hepatitis B immunization.
Hepatitis D is an inflammatory liver disease caused by the hepatitis D virus, which requires the presence of the hepatitis B virus to replicate. Without hepatitis B, infection with hepatitis D is impossible.
Co-infection with hepatitis D and B viruses is considered the most severe form of chronic viral hepatitis due to the more rapid progression of fatal liver failure or hepatocellular carcinoma. The only way to prevent hepatitis D is vaccination against hepatitis B.
Viral hepatitis - symptoms and treatment
It is advisable to consider the detailed pathogenesis of each type of viral hepatitis in separate articles. It is enough to understand the options for normal functioning of the liver and the general mechanisms of its pathology.
The formation and metabolism of bilirubin is normal
Bilirubin is a product of the transformation of hemoglobin (Hb), a kind of “waste” that must be removed from the body. It is formed mainly from Hb, which is released from red blood cells (lifespan 120 days). The destruction of hemoglobin and the formation of bilirubin occurs in the cells of the phagocytic mononuclear cell system:
- Vysokovich-Kupffer cells, which capture and process old non-functional liver blood cells;
- splenic phagocytes - cells of the immune system that protect the body by absorbing harmful foreign particles or dying cells.
A brief scheme for the formation of bilirubin looks like this:
Red blood cells (in the spleen) - Hemoglobin (in the spleen) - Verdoglobin (a product of the enzymatic oxidation of the non-protein part of hemoglobin, formed in the cells of the macrophage system) - Biliverdin (an intermediate product of the breakdown of hemoglobin).
Stages of formation and excretion of bilirubin:
- First phase: formation of free (indirect) bilirubin in the spleen and hepatocytes (liver tissue cells).
- The second phase: its entry into the blood and transfer by albumins (simple water-soluble proteins) into hepatocytes.
- Third phase: binding of free bilirubin with glucuronic acid in hepatocytes (formation of bound, or direct, bilirubin).
- Fourth phase: release of direct bilirubin by hepatocytes as part of bile into the bile capillary.
- Fifth phase: entry of bilirubin-diglucoronide (direct bilirubin) into the duodenum in the form of bile.
Bilirubin diglucoronide can undergo two transformations:
- In the large intestine, it is converted into stercobilinogen, a substance created by colonic bacteria. Stercobilinogen is yellow in color and is further excreted in the feces in the form of stercobilin (provides the normal brown color of stool).
- In the small intestine it is converted into urobilinogen, a colorless product of the reduction of bilirubin, formed under the action of small intestinal bacteria. It is excreted through the kidneys with urine in the form of urobilin, and also enters the portal vein system into the liver with subsequent destruction.
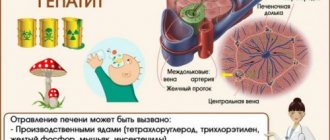
Pathology of bilirubin metabolism in viral hepatitis
Damage to hepatocytes leads to a weakening of the uptake of free bilirubin and disruption of the process of addition of glucuronic acid to it (phase 3). As a result, the content of free bilirubin in the blood increases. Impaired transport of conjugated bilirubin into the bile capillary (phase 4) leads to an increase in conjugated bilirubin in the blood. At the same time, intrahepatic cholestasis is observed, i.e., the level of both free and bound bilirubin in the blood increases, and there is more of the latter (the skin turns yellow).
Bound bilirubin (the urine becomes dark in color) and bile acids penetrate from the blood into the urine, which reduce the surface tension of the urine and cause it to foam easily. Little bound bilirubin enters the intestines - the stool becomes discolored. Due to intrahepatic cholestasis and impaired bile secretion, little bile enters the intestine. Since bile is necessary for the digestion of fatty foods and the absorption of fat-soluble vitamins, due to its lack, a lot of fat remains in the stool (steatorrhea), and the absorption of vitamin K is impaired. Due to the low level of vitamin K, the synthesis of prothrombin in the liver decreases, as a result, blood clotting worsens .
General pathogenetic mechanisms in the liver during hepatitis
Cytolysis syndrome (cytolytic syndrome) is a set of signs indicating a disruption of the liver due to a violation of the integrity of liver cells and the release of liver enzymes into the blood. The degree of increase in the activity of aminotransferases (enzymes that reflect the functionality of the human liver) indicates the severity of the cytolytic syndrome, but does not directly indicate the depth of the dysfunction of the organ.
There is an empirical de Ritis coefficient - AsAT/AlAT. It reflects the ratio of the activity of serum AST (aspartate aminotransferase) and ALT (alanine aminotransferase). The de Ritis coefficient approximately indicates the predominant damage to one or another parenchymal organ. For hepatitis, its value is less than 1.33. In a healthy person it is in the range of 0.91-1.75.
Cholestasis syndrome is characterized by a violation of the outflow of bile. It lingers in the intrahepatic bile ducts, causing the liver tissue to swell and swell. There is an accumulation of bilirubin, cholesterol, β-lipoproteins and alkaline phosphatase in the blood. Also characteristic is the appearance of cholemia, a pathological syndrome characterized by the accumulation of bile acids in the blood. Normally, the acid content in the blood is 5-25 mmol/liter. If their number increases, cholemia develops, which is accompanied by itching, scratching, damage to the central nervous system (CNS) and staining of the skin through bile (80% bile acids + bilirubin).
Mesenchymal-inflammatory syndrome - damage to the liver parenchyma, connective tissue stroma, reticuloendothelium. Clinically expressed by enlarged liver and spleen, increased body temperature, acute phase parameters, as well as the level of autoantibodies, thymol test, β and γ proteins.
Immunosuppressive syndrome (secondary immunodeficiency) is a temporary or permanent depression of the immune system that develops under the influence of certain chemical and physical influences on the body, as well as due to certain infectious processes.
Biliary dyskinesia syndrome is a violation of their motility. It may occur due to changes in the innervation of the biliary tract due to the relative predominance of the tone of the vagus or sympathetic nerve.
Hepatic cell failure is a pathological process in which massive death of liver cells occurs. This condition is characterized by a decrease in albumin (manifested by edema syndrome) and a decrease in prothrombin (manifested by lethargy, fatigue, nausea, vomiting, hemorrhagic rash) [2][3][5][7][9].
Territorial distribution
A study conducted in collaboration with WHO and published in 2021 in the Journal of Hepatology1 estimates that hepatitis D virus affects nearly 5% of people with chronic hepatitis B worldwide and approximately one in five cases of liver disease and cancer. liver disease in those infected with hepatitis B is associated with coinfection with hepatitis D. The study identified several geographic areas of high prevalence of hepatitis D, including Mongolia, the Republic of Moldova, and several countries in West and Central Africa.
Symptoms
Acute hepatitis: Co-infection with hepatitis B and D viruses can lead to moderate to severe hepatitis and in some cases fulminant hepatitis, but complete recovery usually follows and chronic hepatitis D is rare (in less than 5% of cases). cases of acute hepatitis).
Superinfection: a person who already has chronic hepatitis B can become infected with the hepatitis D virus. Superinfection with hepatitis D against the background of chronic hepatitis B leads to the accelerated development of more severe forms of the disease in 70-90% of patients, regardless of age. Patients superinfected with hepatitis D develop cirrhosis nearly 10 years faster than patients infected with hepatitis B alone. Patients with cirrhosis due to hepatitis D virus are at increased risk of developing hepatocellular carcinoma. The reason why hepatitis D virus causes more severe disease and accelerated fibrosis compared with hepatitis B monoinfection remains unknown.
HDV structure
HDV belongs to the genus Deltavirus, is a satellite virus and is a spherical particle with a size of about 36 nm, inside of which there is a nucleocapsid with a diameter of 19 nm. The surface shell of HDV is represented by HBsAg and includes proteins encoded by Pre-S1, Pre-S2 and S-zones of HBV DNA. Moreover, unlike HBV, the ratio of these proteins is presented as 1:5:95.
The HDV nucleocapsid consists of 70 molecules of delta antigen (HDAg), which has two forms: long (LHDAg) - 214 amino acids (27 kDa) and short (SHDAg) - 195 amino acids (24 kDa). The L-form of HDAg differs from the S-form only by the presence of an additional 19 amino acid residues at the C-terminus of the molecule. While SHDAg is required for viral replication, LHDAg, on the contrary, has the ability to suppress HDV replication, but plays a key role in the mechanism of virus assembly and secretion.
HDV RNA is a single-stranded minus strand of 1,700 nucleotide bases and is the smallest RNA virus that infects humans. The HDV genome has 6 open reading frames, of which only 1 is involved in transcription and is responsible for the synthesis of HDAg.
The replication mechanism of the RNA virus is unique in its own way and occurs through the so-called “double repeating cycle”. During the replication process, 3 forms of viral RNA are present in the cell: genomic (negative polarity), antigenomic RNA (positive polarity) and messenger RNA, which contains an open reading frame for the synthesis of HDAg. The virus has the unique ability to use RNA-dependent human RNA polymerases to transcribe its own RNA without producing intermediate forms of DNA.
Who is at risk?
Carriers of chronic hepatitis B are at risk of contracting hepatitis D.
Individuals who are not immune to hepatitis B (i.e., have not had the disease or have not been vaccinated against hepatitis B) are at risk for contracting hepatitis B, which in turn is a risk factor for contracting hepatitis D.
Groups at highest risk of co-infection with hepatitis B and D viruses include indigenous peoples, people living with HIV, and people who inject drugs.
Patients on hemodialysis, men who have sex with men, and sex workers also appear to be at increased risk of co-infection.
Migration from countries with a high prevalence of hepatitis D to areas with a lower prevalence of hepatitis D may have a negative impact on the epidemiology of hepatitis D in the host country.
Prevention
Prevention measures used to prevent liver tissue damage are aimed at correcting a person’s lifestyle, eliminating risk factors for re-infection, and improving the patient’s quality of health and life.
This is interesting: Routes of transmission, symptoms, treatment and prevention of hepatitis E
Principles of prevention:
- limiting unprotected sexual intercourse for both women and men;
- use of contraception;
- fight against drug addiction;
- safe performance of invasive manipulations is achieved through the use of disposable materials (needles, syringes) not only in a medical institution, but also in other organizations (tattoo studio, cosmetology parlor);
- use of personal hygiene products;
- improving methods for testing transfused blood samples;
- vaccination against HBV also provides protection against hepatitis D (immunization is especially important in children);
- vitamin therapy;
- improvement of social and living conditions.
Screening and diagnosis
Diagnosis of hepatitis D is carried out by detecting a high concentration of antibodies to the hepatitis D virus of the class immunoglobulin G (IgG) and immunoglobulin M (IgM); To confirm the diagnosis, a test is carried out for the presence of hepatitis D virus RNA in the blood serum.
However, diagnostic tools for hepatitis D are poorly available, and hepatitis D virus RNA tests, which are used to monitor response to antiviral therapy, are not standardized.
If it is not possible to perform a quantitative test for hepatitis D virus RNA, it is advisable to conduct a quantitative test for HBsAg to monitor the response to therapy. A decrease in HBsAg titer often indicates disappearance of this surface antigen and clearance of the hepatitis D virus, although disappearance of surface antigen is rare in patients undergoing treatment.
Treatment
Current guidelines generally recommend pegylated interferon alfa for at least 48 weeks, regardless of response to treatment. The overall rate of sustained virological response is low, but this treatment is an independent factor associated with a lower likelihood of disease progression.
Current guidelines generally recommend pegylated interferon alfa for at least 48 weeks, regardless of response to treatment. With this treatment, the overall rate of sustained virological response is low, but its administration is an independent factor associated with a lower likelihood of disease progression. However, interferon treatment is associated with significant side effects and is contraindicated in patients with decompensated cirrhosis, active psychiatric diseases and autoimmune diseases.
More efforts are required to reduce the global burden of chronic hepatitis B and develop safe, effective and affordable hepatitis D drugs; this would ensure widespread access to treatment for those who urgently need it.
Therapy for chronic hepatitis delta
The main goal of antiviral therapy is to increase the duration and improve the quality of life of patients. Treatment objectives are:
- suppression of replication of HBV, HDV viruses;
- clearance of HBeAg, HBsAg antigens or their seroconversion;
- normalization of ALT activity levels;
- reduction of inflammation and fibrosis;
- reducing the risk of developing liver cirrhosis and its decompensation, hepatocellular carcinoma;
- reduction of extrahepatic manifestations;
- prevention of HBV recurrence in the graft.
In the treatment of chronic hepatitis D, interferon preparations (interferon-α and pegylated interferons-α (PEG IFN-α)) are used.
Nucleoside analogues (lamivudine, telbivudine, adefovir (not registered in the Russian Federation) and entecavir) are ineffective in suppressing HDV replication (due to the absence of the virus’s main target of action, reverse transcriptase). However, nucleoside analog therapy should be considered in patients with active HBV replication (HBV DNA greater than 2000 IU/mL).
Interferon-α has been used to treat chronic hepatitis D since the mid-1980s. The dose and duration of interferon administration were studied on a large number of observations. Small randomized controlled trials using 3–9 million IU of interferon-α for 3–24 months have shown that biochemical and virological responses are achieved in 70% of patients with chronic hepatitis D by the end of therapy.
It was found that higher doses of interferon-α (9 million IU 3 times a week) for 12 months suppress HDV replication, help normalize ALT levels and improve the histological structure of the liver in patients with chronic hepatitis D.
However, more than half of patients experience a relapse of the disease after treatment. SVR—the absence of HDV RNA 6 months after completion of antiviral therapy is observed on average in 25–28% of patients.
PEG-IFN-α was introduced into the treatment of CGD in 2006. The study of the effectiveness of PEG-IFN-α (HIDIT-1 - The Hep-Net International Delta Hepatitis Interventional Trial) included 90 patients from Germany, Turkey and Greece who were divided into three groups: group 1 received therapy with 180 mcg PEG-IFN-2α in combination with Adefovir (10 mg/day), group 2 - 180 mcg PEG-IFN-2α weekly and placebo, group 3 - Adefovir only (10 mg/day) for 48 weeks.
Among patients receiving PEG-IFN2α, there was a significant decrease in serum HDV RNA compared with patients on Adefovir monotherapy. In addition, HDV RNA was not detected after completion of therapy in the group of patients receiving PEG-IFN-2α (27%). The combination of PEG-IFN-2α with Adefovir resulted in a reduction in serum HBsAg of only 1.1 log10 after 48 weeks of therapy and did not result in an increase in SVR compared with patients receiving PEG-IFN-2α alone.
In summary, the HIDIT-1 trial demonstrated significant antiviral efficacy of PEG-IFN-2α against HDV in more than 40% of patients, with 25% achieving SVR at 48 weeks of treatment. Adefovir had no effect on reducing HDV RNA levels; its use is only necessary for patients with significant HBV replication.
PEG-IFN-2α + nucleoside analogue combination therapy is superior to reverse transcriptase inhibitor (RTI) monotherapy in reducing serum HBsAg levels in HDV-infected patients with active HBV replication.
In June 2009, the second study evaluating the effectiveness of PEG-IFN-2α in combination with IOT (HIDIT II) was launched and is scheduled to end in May 2021. Patients with chronic hepatitis D (70 people) will receive PEG-IFN-2α (180 mcg) in combination with Tenofovir (245 mg), and the comparison group was PEG-IFN-2α (180 mcg) in combination with placebo.
A new direction in the treatment of chronic hepatitis D is the development of drugs that inhibit the binding of HDV and HBV. Thus, Mirkludex B is the first developed inhibitor of HDV and HBV binding. Today it is the only representative of a new class of molecules with activity against HDV and HBV.
The proposed mechanism of action of this drug is its ability to firmly bind to specific (however, still not fully studied) receptors for HBV located on the surface of hepatocytes, which does not allow viral particles to penetrate into the cell and, as a result, prevents the spread of infection. This mechanism of action makes it possible to solve two of the most important medical problems: to ensure long-term eradication of HBV and to prevent the development of hepatitis D.
By the end of 2011, preclinical studies of the safety of the drug under development were carried out, as well as an assessment of its antiviral effectiveness in in vitro and in vivo models. In an in vivo model with transplanted hepatocytes sensitive to HBV infection, the use of the drug completely prevented the development of hepatitis B. At the beginning of 2012, a phase Ia clinical trial was completed, which showed the safety and good tolerability of the drug. Phase Ib-IIa clinical trials are planned in patients with chronic hepatitis B and chronic hepatitis D.
In addition, a second group of drugs is currently being studied that affects the processes of post-translational modification of HDV antigens, in particular the processes of prenylation, i.e. modification of the cysteine residue at the C-terminus of the L-HDVAg molecule, which enhances the lipophilic properties and ensures a stable connection of the HDV nucleocapsid with the virus envelope (HBsAg). There is no doubt that this direction is promising for future antiviral therapy of chronic hepatitis D.
Delta infection and liver transplantation
Liver transplantation is the only treatment option for patients with end-stage liver disease, hepatocellular carcinoma in the absence of extrahepatic metastases, and for patients with fulminant hepatitis due to HDV/HBV co-infection or HDV superinfection.
Patients chronically infected with HBV and HDV have a lower risk of post-transplant HBsAg recurrence and better survival than patients infected with HBV alone.
Multivariate analysis showed that independent predictors of a lower risk of recurrent HBV infection after transplantation were HDV infection, absence of active HBV replication (negative detection of HBV DNA and HBeAg in the blood serum before transplantation), acute liver failure and long-term administration of anti-HBV immunoglobulin (HBIg).
On the contrary, the presence of hepatocellular carcinoma or recurrence of hepatocellular carcinoma after liver transplantation, as well as concomitant HIV infection, are the main factors for reinfection with HBV and HDV.
However, patients with delta infection remain at risk for re-infection with both HBV and HDV. In a European multicenter study, the risk of recurrent HBV infection within three years in patients receiving long-term HBIg was 70% and 17%, respectively, in HBV- and HDV-infected patients.
The survival rates of patients after liver transplantation for HBV cirrhosis and HDV cirrhosis reached 48 and 85%, respectively. In a cohort of 76 patients with HDV cirrhosis receiving long-term HBIg, the 5-year survival rate after liver transplantation reached 88%, and re-detection of HBsAg was observed in 10% of patients.
The European Liver Transplant Registry showed that 5-year survival was 89% in patients with HDV cirrhosis and 86% in patients without hepatocellular carcinoma, and 10-year survival was 78 and 73%, respectively.
Patient survival depends on preventing reinfection with HBV and HDV after liver transplantation or slowing the progression of the disease in the presence of relapse. The use of potent antiviral drugs against HBV further reduces the risk of HBV/HDV reinfection.
Significant progress in the treatment of chronic hepatitis B came with the introduction of highly effective and well-tolerated anti-HBV nucleoside analogues, such as Lamivudine and Adefovir, which, in combination with HBIg, reduced the risk of re-infection by 10% in the first 2 years after transplantation. The combination of HBIg with Lamivudine is the “gold standard” for preventing recurrent infection.
Today, the use of low doses of HBIg in combination with a potent nucleoside analogue (Entecavir) is the most cost-effective prevention of reinfection. In patients with delta infection, this strategy is justified in the presence of initially active HBV replication. In addition, given the rapid development of drug resistance of HBV to Lamivudine, it is preferable to use drugs with a high genetic barrier that are highly effective against HBV (Entecavir, Tenofovir, or a combination thereof).
In order to control the possible risk of reinfection with HBV and HDV, the emergence of HBV drug resistance in liver recipients, HBsAg and HBV DNA should be determined every 3 months, HDV RNA - every 6 months.
WHO activities
In May 2021, the World Health Assembly adopted the first Global Health Sector Strategy on Viral Hepatitis 2016–2021. The strategy emphasizes the critical role of universal health coverage and aligns its objectives with those of the 2030 Sustainable Development Goals. The strategy's overarching goal is to eliminate viral hepatitis as a public health problem and is reflected in global targets to reduce the number of new cases of viral hepatitis infection by 90% and reduce deaths from viral hepatitis by 65% by 2030. The strategy sets out the measures that countries and the WHO Secretariat must take to achieve these goals.
WHO has not published specific recommendations for hepatitis D; Effective means of preventing hepatitis D infection include prevention of hepatitis B transmission through vaccination, including timely administration of the first dose of vaccine immediately after birth, additional preventive antiviral therapy for pregnant women with appropriate indications, ensuring blood safety, maintaining injection safety when providing medical care, as well as health care services. reducing harm associated with injecting drug use, such as providing sterile needles and syringes. WHO is supporting Member States to scale up these evidence-based interventions.
In addition, to support countries in meeting the global hepatitis targets of the 2030 Agenda for Sustainable Development, WHO is working in the following areas:
- raising awareness, facilitating partnerships and mobilizing resources;
- developing evidence-based policy and collecting data to inform action;
- improving health equity in the hepatitis response;
- prevention of transmission of infection;
- expanding coverage of screening, care and treatment services.
In 2021, WHO is celebrating World Hepatitis Day under the theme “The fight against hepatitis can't wait” to highlight the urgency of eliminating hepatitis in order to achieve the goals by 2030. Key messages relate to the latest estimates of the burden of viral hepatitis and mortality from viral hepatitis at the global and regional levels, as well as the need to ensure certification of the elimination of hepatitis as a public health threat by 2030.