What's happening?
During the formation of the placenta, chorionic villi “invade” the uterine mucosa (endometrium). This is the same membrane that is shed during menstrual bleeding. However, there are cases when villi grow into the muscle layer, and sometimes throughout the entire thickness of the uterine wall. A dense attachment or accretion of the placenta occurs, differing in the depth of growth of the chorionic villi into the wall of the uterus.
Unfortunately, it is possible to recognize placenta accreta and tight attachment (and distinguish them from each other) only during childbirth, during the operation of manual separation of the placenta. If the placenta is tightly attached and accreted in the afterbirth period (III stage of labor), the placenta does not separate spontaneously.
Dense attachment or placenta accreta can be complete if the placenta is attached to its bed over the entire area, and partial if the placenta is attached only in one area. In the first case, spontaneous bleeding does not occur. In the second, when placental abruption begins, bleeding occurs, which can be very heavy.
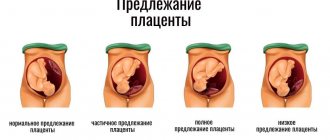
Location of the placenta: norm and pathology
On the side of the uterus, at the placenta attachment site, there is a thickening of the inner membrane. In it, depressions are formed that form the intervillous space. Some villi of the placenta grow together with the maternal tissues (they are called anchor), while the rest are immersed in maternal blood, filling the intervillous space. The anchor villi of the placenta are attached to the septa of the intervillous spaces; vessels that carry arterial maternal blood, saturated with oxygen and nutrients, pass through the thickness of the septa.
The placental villi secrete special substances - enzymes that “melt” small arterial vessels carrying maternal blood, as a result of which blood flows from them into the intervillous space. It is here that the exchange takes place between the blood of the fetus and the mother: with the help of complex mechanisms, oxygen and nutrients enter the blood of the fetus, and metabolic products of the fetus enter the blood of the mother. The fetus is connected to the placenta using the umbilical cord. One end of it is attached to the umbilical region of the fetus, the other to the placenta. Inside the umbilical cord there are two arteries and a vein, carrying blood from the fetus to the placenta and back, respectively. Blood rich in oxygen and nutrients flows through the umbilical cord vein to the fetus, and venous blood from the fetus, containing carbon dioxide and metabolic products, flows through the arteries.
Normally, the placenta is located closer to the fundus of the uterus along the anterior or, less commonly, posterior wall. This is due to more favorable conditions for the development of the fertilized egg in this area. The mechanism for choosing the place of attachment of the fertilized egg is not completely clear: there is an opinion that gravity plays a role in choosing the place - for example, if a woman sleeps on her right side, then the egg is attached to the right wall of the uterus. But this is just one theory. What can be said with certainty is that the fertilized egg does not attach to unfavorable places for this, for example, to the location of myomatous nodes or to places where the inner lining of the uterus is damaged as a result of previous curettages. Therefore, there are other options for the location of the placenta, in which the placenta is formed closer to the lower part of the uterus. There are low-lying placenta and placenta previa.
The placenta is said to be low when its lower edge is located at a distance of no more than 6 cm from the internal os of the cervix. This diagnosis is usually made during an ultrasound. Moreover, in the second trimester of pregnancy, the frequency of this pathology is approximately 10 times higher than in the third trimester. It's quite simple to explain. Conventionally, this phenomenon is called “migration” of the placenta. In fact, the following happens: the tissues of the lower part of the uterus, which are very elastic, undergo significant stretching and are pulled upward as the duration of pregnancy increases. As a result of this, the lower edge of the placenta seems to move upward, and as a result, the location of the placenta becomes normal.
Placenta previa is a more serious diagnosis. In Latin this condition is called placenta praevia. “Pre via” literally means before life. In other words, the term “placenta previa” means that the placenta is on the way to giving birth to new life.
Placenta previa can be complete or central, when the entire placenta is located in the lower part of the uterus and completely covers the internal os of the cervix. In addition, partial placenta previa occurs. This includes marginal and lateral presentation. A lateral placenta previa is said to occur when up to 2/3 of the uterine outlet is covered by placental tissue. With marginal placenta previa, no more than l/3 openings are closed.
Manual separation of the placenta
Indications for surgery:
- no signs of placental separation without bleeding 30 minutes after the birth of the baby;
- no signs of placental separation when bleeding begins, as soon as blood loss reaches 250 ml
The operation is performed under intravenous anesthesia. Simultaneously with the start of the operation, drip administration of glucose, crystalloid solutions, and uterine contractions is started. When firmly attached, the placenta is easily separated from the uterine wall.
After manual examination of the walls of the uterine cavity and confidence that it has completely emptied, oxytocin is injected intravenously, an ice pack is placed on the lower abdomen, and the condition of the uterus is periodically monitored by palpation through the anterior abdominal wall. In order to prevent postpartum infection, antibiotics are prescribed in all cases of surgical intervention in the afterbirth period. In case of pathological blood loss (500 ml or more), blood loss is compensated.
In case of accreta, the placenta (or part of it) cannot be separated from the uterus. In this situation, doctors are obliged to stop all attempts to separate the placenta and perform an urgent removal of the uterus.
Bleeding in the third stage of labor associated with abnormal placental attachment should be differentiated from bleeding caused by retention or strangulation of the separated placenta .
Conditions such as placenta previa and placenta accreta can lead to catastrophic consequences for both mother and fetus, especially during full-term pregnancy. Obstetric hemorrhage caused by placenta previa is one of the leading causes of maternal mortality [1–3].
The problem of diagnosing true placenta accreta and developing treatment methods for patients with this pathology seem extremely relevant, since, on the one hand, such a pathology is associated with a high risk for a woman’s life due to profuse bleeding during placenta separation, often leading to hysterectomy, on the other — its prevalence has increased significantly with the increase in the number of cesarean sections [4–7].
One of the main factors predisposing to placenta accreta is its localization in the lower parts of the uterus and the presence of a scar after cesarean section. The risk of infiltration of villi throughout the thickness of the myometrium increases with a history of several abdominal deliveries [8–10], and the situation may be complicated by involvement of the posterior wall of the bladder in the pathological process.
The purpose of this work is to present a combined approach for surgical delivery of 2 patients with placenta accreta in the area of the uterine scar after myomectomy, including the intraoperative use of two autonomous Zhukovsky balloon catheters (vaginal and uterine) [11], bilateral ligation of the uterine vessels, application of a supraplacental seromuscular hemostatic suture.
Clinical observation No. 1
Multigravida, primigravida N
., 43 years old, was admitted to the maternity hospital of the budgetary healthcare institution of the Omsk region “Regional Clinical Hospital” on November 8, 2016 with a diagnosis of 39 weeks of pregnancy. Head presentation. Scars on the uterus after a minor cesarean section and three myomectomies. Suspicion of placenta accreta. Isthmic-cervical insufficiency (ICI), corrected with an obstetric pessary. Gestational diabetes mellitus. Arterial hypertension is moderate. Complicated obstetric and gynecological history.
Anthropometric data of the woman: height 164 cm, body weight 71 kg.
There were 3 myomectomies in the anamnesis for large subserous uterine fibroids: in 2005 - laparotomy, enucleation of a 10 cm node in the left uterine angle, histological examination: cellular leiomyoma; in 2010 - laparotomy, enucleation of a 6 cm node in the left uterine angle, histological examination: leiomyoma; in 2012 - laparotomy, enucleation of a 6 cm node in the left uterine angle, histological examination: leiomyoma.
This was my fifth pregnancy, and my first birth was coming. Previous pregnancies: 1) 2004 - non-developing pregnancy at 6-7 weeks of pregnancy, vacuum aspiration of the ovum; 2) 2006 - termination of pregnancy for medical reasons (congenital malformations of the fetus), minor caesarean section at 20 weeks; 3) 2009 - non-developing pregnancy at 6-7 weeks, vacuum aspiration of the ovum; 4) 2012 - spontaneous abortion at 5-6 weeks of pregnancy.
The course and complications of this pregnancy.
She was registered at the antenatal clinic from the 11th week; threat of interruption - at 9 weeks, inpatient treatment. In order to correct ICI, an obstetric pessary was installed at 15-16 weeks. Dr. Arabin received progesterone (Utrozhestan 200 mg) until 36 weeks of pregnancy. At 17 weeks there was a threat of miscarriage and she received hospital treatment. An increase in blood pressure (BP) to 130/90 mm Hg was noted; the total weight gain during pregnancy was 10 kg.
At the time of receipt, she did not make any complaints. General condition is satisfactory. Vision is clear. No headache. The skin is of normal color. The abdomen is enlarged due to the pregnant uterus; palpation is soft and painless. The area of postoperative scars on the uterus is painless upon palpation. The uterus is in normal tone. The position of the fetus is longitudinal, the head is presented above the entrance to the pelvis. The fetal heartbeat is muffled, rhythmic, up to 140 beats per minute. The waters are intact. There is no swelling. Physiological functions are normal. Vaginal examination: the vagina of a nulliparous woman, the cervix is in an obstetric pessary, located in the center, up to 2.0 cm long, moderately softened, the cervical canal allows the tip of the examining finger to pass through; the amniotic sac is intact; the head is presented above the entrance to the pelvis; the basin is capacious, the cape is not reachable.
Ultrasound examination was carried out using a SonoScape-8000Pro device. There is a living fetus in the uterine cavity, cephalic presentation, longitudinal position, first position, anterior view. The fetometric parameters of the fetus corresponded to 38.5 weeks of pregnancy. No congenital malformations were detected, fetal weight was 3362 g. The placenta was located on the posterior wall, 10 cm above the internal os. The thickness of the placenta was 43 mm, stage III of maturity, structure with calcifications. The amniotic fluid index is 11.2 cm. There is no hypertonicity. The wall of the uterus in the placentation zone is thickened due to the expanded vascular network.
At this stage, taking into account the scars on the uterus after a minor cesarean section and three myomectomies, in a 43-year-old primigravida with a particularly burdened obstetric and gynecological history, it was decided to deliver the pregnant woman by cesarean section as planned.
On the same day, the patient was examined by an anesthesiologist-resuscitator, and regional spinal anesthesia was recommended for a cesarean section. Given the high risk of bleeding, intraoperative reinfusion of autologous red blood cells using the Cell Saver device is recommended.
11/09/16 (10:50–12:10) under regional spinal anesthesia, a cesarean section was performed in the presence of a perfusionist. The anterior abdominal wall was opened in layers from the womb to the navel. Upon opening of the peritoneum, it was discovered that the size of the uterus corresponds to a full-term pregnancy; in the fundus of the uterus and along the left corner of the uterus there were cicatricial changes in the wall after myomectomy; no myomatous nodes were identified. The uterine cavity was opened with a transverse incision in the area of the lower segment according to Gusakov. Light amniotic fluid was released in the amount of 500 ml. At the 5th minute, a live full-term boy weighing 3076 g, height 51 cm, without visible malformations, with an Apgar score of 7 and 8 points was extracted.
In order to reduce blood loss, bilateral ligation of the uterine vessels was performed. There were no signs of placental separation. External methods of separating the placenta were without effect. It was decided to perform manual separation of the placenta. When examining the uterine cavity, the placenta was located along the posterior wall of the uterus with a transition to the fundus. When attempting to separate the placenta using sawing movements of the right hand, in the left uterine angle, in the area of the postoperative scar, placenta accreta was detected along its entire length (10×10 cm). Resection of the left uterine angle with placenta accreta was performed (Fig. 1).
Rice. 1. The placenta together with the resected portion of the uterine wall. a - placenta; b — resected section of the uterus with an ingrown placenta. The resected area of the uterus is sutured with separate eight-shaped sutures. The uterine cavity was inspected and blood clots were removed. To stop bleeding of the surgical wound area on the uterus, a local hemostatic agent, Hemoblock, was used. Method of application: externally, sterile gauze pads were moistened with the solution and applied to the bleeding, previously dried surface of the wound for 3 minutes.
A supraplacental seromuscular hemostatic suture is placed on the posterior wall of the uterus. The uterine cavity was dried with napkins. Separate vicryl sutures are placed at the corners of the wound on the uterus. A modified balloon uterine catheter was inserted through the hysterotomy incision using a guide wire through the cervical canal. The wound on the uterus is stitched with separate eight-shaped sutures. A modified balloon uterine catheter was filled with isotonic sodium chloride solution after suturing the wound on the uterus, then the vaginal module was brought intravaginally through a guide to the uterine balloon, filling it with 150 ml of isotonic sodium chloride solution. The duration of placement of the vaginal and uterine catheters was 14 hours. Intraoperative blood loss was 1500 ml, urine output was 100 ml. Blood reinfusion with Cell Saver 600 ml.
The postoperative period was uneventful; antibacterial and uterotonic therapy was carried out. The woman was discharged in satisfactory condition with the child on the 6th day.
Histological examination of an excised section of the uterine wall with the placenta reveals deep ingrowth of chorionic villi into the myometrium.
Clinical observation No. 2
Primigravida, primigravida M
., 32 years old, was admitted to the maternity hospital of the budgetary healthcare institution of the Omsk region “Regional Clinical Hospital” on November 15, 2016 with a diagnosis of 37 weeks of pregnancy. Head presentation. Scars on the uterus after myomectomy. Multiple large uterine fibroids. Isthmic-cervical insufficiency corrected with an obstetric pessary. Chronic pyelonephritis without exacerbation. Nephroptosis on the right.
Anthropometric data of the woman: height 162 cm, body weight 80 kg.
There is a history of two myomectomies for large subserous uterine fibroids: 2013 - laparotomy, enucleation of an 8 cm node in the right uterine angle, histological examination - cellular leiomyoma; 2021 (July) - laparotomy, enucleation of a 10 cm node in the left uterine angle, histological examination - leiomyoma.
The course and complications of this pregnancy: registered at the antenatal clinic from 10 weeks; for the purpose of correcting ICI, an obstetric pessary was installed at 17 weeks. Dr. Arabin received progesterone (utrozhestan 400 mg) until 36 weeks; the total weight gain during pregnancy was 8 kg.
At the time of receipt, she did not make any complaints. General condition is satisfactory. Vision is clear. No headache. The skin is of normal color. The abdomen is enlarged due to the pregnant uterus; upon palpation it is soft and painless. The area of the postoperative scar on the uterus is painless upon palpation. The uterus is in normal tone. The position of the fetus is longitudinal, the head is presented above the entrance to the pelvis. The fetal heartbeat is muffled, rhythmic, up to 150 beats per minute. The waters are intact. There is no swelling. Physiological functions are normal. Vaginal examination: the vagina of a nulliparous woman, the cervix - in an obstetric pessary, in the center, up to 1.5 cm long, moderately softened, the cervical canal allows the tip of the examining finger to pass through; the amniotic sac is intact; the head is presented above the entrance to the pelvis; the basin is capacious, the cape is not reachable.
Ultrasound examination was carried out using a SonoScape-8000Pro device. There is a living fetus in the uterine cavity, cephalic presentation, longitudinal position, first position, anterior view. Fetometric indicators of the fetus correspond to 37 weeks. No congenital malformations were found, the fetal weight was 2914. The placenta was located along the posterior wall with a transition to the bottom, 9 cm above the internal os. The thickness of the placenta was 37 mm, stage III of maturity. The amniotic fluid index is 21.7 cm. There is no hypertonicity. In the lower segment, along the posterior wall, a myomatous node measuring 69×64×63 mm is identified. In the fundus of the uterus, two myomatous nodes are identified in the placentation zone measuring 38×15×31 and 45×42×43 mm; with color Doppler mapping (CDC) they are avascular.
At this stage, taking into account the scars on the uterus after two myomectomies, including 07/05/16, multiple large uterine fibroids, it was decided to deliver the pregnant woman early by cesarean section as planned.
She was examined by an anesthesiologist-resuscitator, and regional spinal anesthesia was recommended for a cesarean section. Given the high risk of bleeding, intraoperative reinfusion of autologous red blood cells using the Cell Saver device is recommended.
On 11/18/16 (9:15–10:50) a cesarean section was performed under regional spinal anesthesia in the presence of a perfusionist. The anterior abdominal wall was opened in layers from the womb to the navel. After opening the peritoneum, the uterine cavity was opened with a transverse incision in the area of the lower segment according to Gusakov. Light amniotic fluid was released in the amount of 400 ml. At the 5th minute, a live full-term boy weighing 2743 g, height 49 cm, without visible malformations, with an Apgar score of 7 and 7 points was extracted.
The uterus was brought out into the wound, the following was found (Fig. 2):
Rice. 2. Subserous uterine fibroids, hernial protrusion in the scar on the uterus after myomectomy. a - retrocervical interstitial-subserous myomatous node; b — hernial protrusion; c — interstitial-subserous myomatous node in the fundus. along the posterior wall in the lower segment - an interstitial-subserous myomatous node with a diameter of 9 cm, in the fundus - an interstitial-subserous myomatous node with a diameter of 6 cm. On the posterior wall in the area of the placental site in the area of the old scar after myomectomy - a hernial protrusion with a diameter of 4 cm (placental hernia), pronounced varicose veins of the uterine appendages. In order to reduce blood loss, bilateral ligation of the uterine vessels was performed in case of unseparated placenta.
The placenta is removed by pulling the umbilical cord, the placenta is located along the posterior wall. The bed of the hernial protrusion was examined: an area of ingrowth of placental tissue was discovered; no bleeding. A transverse incision was made in the uterus, and myomectomy of the retrocervical node was performed. The bed is sutured with figure-of-eight sutures, the wound is sutured with a double-row vicryl suture. To stop bleeding in the area of the surgical wound on the uterus, a local hemostatic agent, Hemoblock, was used (Fig. 3).
Rice. 3. Use of a hemoblock after myomectomy with hernial protrusion. a - hernial protrusion; b — local hemostatic Hemoblock. Acute herniotomy was performed. Scar tissue with areas of placenta accreta was excised and removed (Fig. 4).
Rice. 4. Excision of the site of placenta accreta. The bed is sutured with figure-of-eight sutures, the wound is sutured with a double-row vicryl suture. Myomectomy of interstitial-subserous myomatous nodes in the fundus of the uterus was performed similarly.
The uterine cavity was inspected and blood clots were removed. To stop bleeding of the surgical wound area on the uterus, a local hemostatic agent, Hemoblock, was used. A supraplacental seromuscular hemostatic suture is placed on the posterior wall. The uterine cavity was dried with napkins. Separate vicryl sutures are placed at the corners of the wound on the uterus. For controlled uterine tamponade, a modified balloon uterine catheter was installed through the hysterotomy incision with a guidewire inserted through the cervical canal. The wound on the uterus is stitched with separate eight-shaped sutures. A modified balloon uterine catheter was filled with isotonic sodium chloride solution after suturing the wound on the uterus, then the vaginal module was brought intravaginally through a guide to the uterine balloon, filling it with 120 ml of isotonic sodium chloride solution. The duration of placement of the vaginal and uterine catheters was 14 hours. Intraoperative blood loss was 1100 ml, urine output was 150 ml. Blood reinfusion with the Cell Saver device - 500 ml.
The postoperative period was uneventful; antibacterial and uterotonic therapy was carried out. The mother was discharged in satisfactory condition with the baby on the 6th day.
Histological conclusion: the excised section of the uterine wall with the placenta is a deep ingrowth of chorionic villi into the myometrium.
Thus, the above examples show that the use of a combined approach for surgical delivery of patients with placenta accreta in the area of the uterine scar after myomectomy, including the intraoperative use of two autonomous Zhukovsky balloon catheters (vaginal and uterine), bilateral ligation of the uterine vessels, application of supraplacental seromuscular hemostatic suture, allows you to perform organ-preserving operations and preserve the reproductive function of patients.
The authors declare no conflict of interest.
*e-mail; ORCID: https://orcid.org/0000-0002-0357-7097
Sources
- Petersen DS., Kreuter N., Heepe L., Büsse S., Wellbrock AHJ., Witte K., Gorb SN. Holding tight to feathers — structural specializations and attachment properties of the avian ectoparasite Crataerina pallida (Diptera, Hippoboscidae). // J Exp Biol - 2021 - Vol221 - NPt 13 - p.; PMID:29712747
- Mori H., Kobara H., Nishiyama N., Masaki T. Novel concept of endoscopic device delivery station system for rapid and tight attachment of polyglycolic acid sheet. // World J Gastroenterol - 2018 - Vol24 - N2 - p.211-215; PMID:29375206
- Voigt D., Tsipenyuk A., Varenberg M. How tight are beetle hugs? Attachment in matting leaf beetles. // R Soc Open Sci - 2021 - Vol4 - N9 - p.171108; PMID:28989792
- Adams GC., Stoops MA., Skomro RP. Sleep tight: exploring the relationship between sleep and attachment style across the life span. // Sleep Med Rev - 2014 - Vol18 - N6 - p.495-507; PMID:24721278
- Fau M., Kowalczyk A., Olejnik P., Nowicka AM. Tight and uniform layer of covalently bound aminoethylophenyl groups perpendicular to gold surface for attachment of biomolecules. // Anal Chem - 2011 - Vol83 - N24 - p.9281-8; PMID:22047188
True placenta accreta. Conservative therapy
1. Ailamazyan E.K., Repina M.A., Kuzminykh T.U. Another look at the problem of obstetric bleeding // Journal. obstetrics and wives bol. – 2008. – No. 3. – P. 3–11. 2. Angstmann T., Gard G., Harrington T. et al. Surgical management of placenta accreta: a cohort series and suggested approach // Am. J. Obstet. Gynecol. – 2010. – Vol. 202. – P. 38–39. 3. Arulkumaran S., Ng CS, Ingemarsson I. et al. Medical treatment of placenta accreta with methotrexate // Acta Obstet. Gynecol .Scand. – 1986. – Vol. 65, No. 3. – P. 285–286. 4. Chan BCP, Lam HSW, Yuen JHF et al. Conservative management of placenta previa with accreta // Hong Kong Med. J. - 2008. - Vol. 14 – P. 479–484. 5. Clement D., Kayem G., Cabrol D. Conservative treatment of placenta percreta: a safe alternative // Eur. J. Obstet. Gynecol. Reprod. Biol. – 2004. – Vol. 114. – P. 108–109. 6. Flood KM, Said S, Geary M et al. Changing trends in peripartum hysterectomy over the last 4 decades // Am. J. Obstet. Gynecol. – 2009. – Vol. 200. – P. 632.el—632.e6. 7. Henrich W., Surbek D., Kainer F. et al. Diagnosis and treatment of peripartum bleeding // J. Perinat. Med. – 2008. – Vol. 36, No. 6. – P. 467–478. 8. Kayem G., Davy C., Goffinet F. et al. Conservative versus extirpative management in cases of placenta accreta // Obstet. and Gynecol. – 2004. – Vol. 104. – P. 531–536. 9. Kent A. Management of placenta accreta // Rev. Obstet. Gynecol. – 2009. – Vol. 2, No. 2. – P. 127–128. 10. Kotsuji F., Nishijima K., Kurokawa T. et al. Usefulness of the transverse uterine fundal incision for placenta previa // Abstracts of the XXII European congress of perinatal medicine. – Granada, 2010. – P. 618. 11. Lam H., Pun TC, Lam PW Successful conservative management of placenta previa accreta during caesarean section // Int. J. Gynecol. Obstet. – 2004. – Vol. 86. – P. 31–32. 12. Mussalli GM, Shah J, Berck DJ et al. Placenta accreta and methotrexate therapy: three case reports // J. Perinatol. – 2000. – Vol. 20. – P. 331–334. 13. Ophir E., Singer-Jordan J., Odeh M. et al. Abnormal placental invasion – a novel approach to treatment case report and review // Obstet. Gynecol. Surv. – 2009. – Vol. 64, No. 12. – P. 811–822. 14. Palacios Jaraquemada JM, Pesaresi M, Nassif JC et al. Anterior placenta percreta: surgical approach, hemostasis and uterine repair // Acta Obstet. Gynecol. Scand. – 2004. – Vol. 83. – P. 738–744. 15. Palacios Jaraquemada JM, Bruno CH MRI in 300 cases of placenta accereta: surgical correlation of new findings // Acta Obstet. Gynecol. Scand. – 2005. – Vol. 84. – P. 719–727. 16. Son G., Kwon J., Cho H. et al. A case of placenta increta presenting as delayed postabortal intraperitoneal bleeding in the first trimester // J. Korean Med. Sci. – 2007. – Vol. 22. – P. 932–935. 17. Sumigama S., Itakura A., Ota T. et al. Placenta previa increta/percreta in Japan: a retrospective study of ultrasound findings, management and clinical course // J. Obstet. Gynecol. Res. – 2007. – Vol. 33, No. 5. – P. 606–611. 18. Thia EWH, Tan L.-K., Devendra K. et al. Lessons learned from two women with morbidly adherent placentas and a review of literature // Ann. Acad. Med. Singapore. – 2007. – Vol. 36. – P. 298–303. 19. Timmermans S., van Hof AC, Duvekot JJ Conservative management of abnormally invasive placentation // Obstet. Gynecol. Surv. – 2007. – Vol. 62, No. 8. – P. 529–539. 20. Tong SYP, Tay KH, Kwek YCK Conservative management of placenta accreta: review of three cases // Singapore Med. J. – 2008. – Vol.49, No. 6. – P. e156–e159. 21. Vazquez JA, Rivera GV, Higareda SH et al. Obstetric hysterectomy. Incidence, indications and complications // Ginecol. Obstet. Mex. – 2008. – Vol.76, No. 3. – P. 156–160. 22. Yamasmit W., Chaithonqwongwatthana S. Risk factors for cesarean hysterectomy in tertiary center in Thailand: A case-control study // J. Obstet. Gynecol. Res. – 2009. – Vol. 35, No. 1. – P. 60–65. 23. Yi K.W., Oh M.-J., Seo T.-S. et al. Prophylactic hypogastric artery ballooning in a patient with complete placenta previa and increta // J. Korean Med. Sci. – 2010. – Vol. 25. – P. 651–655.
Symptoms and possible complications of placenta previa
The main complications and the only manifestations of placenta previa are spotting. Depending on the type of presentation, bleeding may occur for the first time during various periods of pregnancy or childbirth. Thus, with central (complete) placenta previa, bleeding often begins early - in the second trimester of pregnancy; with lateral and marginal variants - in the third trimester or directly during childbirth. The severity of bleeding also depends on the type of presentation. With complete presentation, bleeding is usually more profuse than with incomplete presentation.
Most often, bleeding appears during pregnancy 28-32 weeks, when the preparatory activity of the lower segment of the uterus is most pronounced. But every fifth pregnant woman diagnosed with placenta previa notes the appearance of bleeding in the early stages (16-28 weeks of pregnancy).
What is the cause of bleeding during placenta previa? During pregnancy, the size of the uterus constantly increases. Before pregnancy, they are comparable to the size of a matchbox, and by the end of pregnancy, the weight of the uterus reaches 1000 g, and its dimensions correspond to the size of the fetus along with the placenta, amniotic fluid and membranes. This increase is achieved mainly due to an increase in the volume of each fiber that forms the wall of the uterus. But the maximum change in size occurs in the lower segment of the uterus, which stretches more as the due date approaches. Therefore, if the placenta is located in this area, then the process of “migration” proceeds very quickly, the low-elastic tissue of the placenta does not have time to adapt to the rapidly changing size of the underlying uterine wall, and placental abruption occurs over a larger or smaller extent. At the site of detachment, damage to blood vessels occurs and, accordingly, bleeding.
With placenta previa, there is often a threat of miscarriage: increased uterine tone, pain in the lower abdomen and lumbar region. Often, with this location of the placenta, pregnant women suffer from hypotension - a persistently reduced blood pressure. A decrease in pressure, in turn, reduces performance, causes weakness, a feeling of weakness, and increases the likelihood of fainting and headaches.
In the presence of bleeding, anemia is often detected - a decrease in the level of hemoglobin in the blood. Anemia can aggravate the symptoms of hypotension, and oxygen deficiency caused by decreased hemoglobin levels adversely affects fetal development. Growth retardation and fetal growth restriction syndrome (FGR) may occur. In addition, it has been proven that children born to mothers who suffered from anemia during pregnancy always have a reduced hemoglobin level in the first year of life. And this, in turn, reduces the baby’s body’s defenses and leads to frequent infectious diseases.
Due to the fact that the placenta is located in the lower segment of the uterus, the fetus often takes an incorrect position - transverse or oblique. Often there is also a breech presentation of the fetus, when its buttocks or legs are facing the exit from the uterus, and not the head, as usual. All this makes it difficult or even impossible to give birth to a child naturally, without surgery.