Testicular torsion in men is an acute pathological condition in which the spermatic cord and neurovascular bundle become twisted into a spiral. As a result, the blood supply is disrupted, which without a visit to the doctor can lead to serious consequences, including death of the gland and infertility. When the first signs of testicular torsion appear, immediate hospitalization is necessary!
Typically, this pathology is observed in young boys and teenagers 12-18 years old. It is extremely rare after reaching 30 years of age.
Testicular torsion: epidemiology, etiology and pathogenesis
Testicular torsion requires immediate medical attention. In its absence, ischemic changes occur in the organ, which can progress and irreversibly disrupt the functioning of the male reproductive gland. Necrosis (death) occurs.
Russian-speaking authors can give this condition other definitions: “torsion of the spermatic cord and testicle”, “volvulus of the spermatic cord”, “torsion of the spermatic cord”, “testicular inversion”.
Torsion is rare, occurring in approximately one in 4,000 representatives of the stronger sex. Usually these are children or adolescents 10–16 years old, occasionally adults and newborns. There is evidence that pathology can develop in the period before birth (that is, in the fetus). As a result, boys are born with only one testicle (monorchidism).
This pathology can occur if the testicle is not properly attached to the bottom of the scrotum.
The following conditions can lead to torsion:
- Abnormal testicular mobility. Its roots may lie in the underdevelopment of various testicular ligaments - the ligament that secures the testicle to the bottom of the scrotum, or the mesentery, which normally secures the testicle to the walls of the scrotum.
- Strong contractions of the levator testis muscle (during sudden movements, tension in the abdominal muscles, injuries, severe and prolonged coughing). One of the triggers is tight underwear.
In general, the testicle that is larger than the other is more susceptible to torsion. New growths or simply individual characteristics may be to blame for this. Torsion occurs along the vertical axis of the testicle from the outside to the inside and can vary in severity.
Sometimes the symptoms of torsion last a short time and disappear on their own - habitual or partial torsion. Of course, in such individuals the likelihood of complete torsion is very high. They are recommended to undergo surgical treatment, which in all cases leads to complete recovery from the symptoms of torsion.
How does removing a testicle affect future fertility?
One testicle is enough to ensure fertility and secrete the required amount of male sex hormones.
With a single testicle, normal amounts of sperm and testosterone are produced. There is some experimental evidence that suggests that fertility may be reduced, but in practice this effect is not observed clinically in men who have had testicular torsion.
What impact does my lifestyle have if I have lost a testicle or have a weak testicle?
Patients who have had a testicle removed or have a loose testicle should be especially careful with the remaining one. They should always wear protection when participating in sporting activities. They should seek medical attention immediately if they experience any discomfort or changes in the scrotum.
Symptoms of testicular torsion
The initial sign of torsion is sharp and severe pain that appears in the scrotum, groin area and lower abdomen. If we are talking about a small child, then nausea and vomiting are often observed.
Symptoms from the testicle include paler than usual skin of the scrotum or bluish skin of the scrotum and increased sensitivity. A testicle that has twisted is larger than the other, normal one, and hangs higher. When palpated, its density and pain are determined.
All local symptoms may appear very weakly, they are overshadowed by general symptoms (pain, fever, nausea).
With this pathology, the development of acute urinary retention cannot be ruled out.
Testicular torsion is painless in newborns. Its presence is determined by the increase in the size of half of the scrotum.
If medical care is not started in a timely manner, then after about a day with torsion, the pain weakens. But local signs of torsion (swelling, redness) rapidly increase. The body temperature increases even more, and the symptoms of intoxication intensify. Rarely (usually in newborns) collapse may occur.
The following types of this pathology are distinguished depending on the relationship to the testicular membrane (the so-called vaginal membrane):
- The extravaginal form of torsion is when the testicle rotates above the place where its tunica vaginalis is attached, and the rotation occurs along with it. It usually occurs in infants or the fetus and ends in congenital necrosis. This requires surgical removal of the testicle.
- Intravaginal form, when the testicle turns over inside the vaginal membrane, and that part of the spermatic cord that lies above the vagina is not changed. It usually occurs in boys aged 10–15 years due to the rapid growth of the gonads.
- Torsion of the testicle on the membrane of its epididymis, the latter remains normal, and only the vessels supplying the testicle are compressed. Occurs when there is significant separation of the epididymis and testicle.
Any form is fraught with cessation or a sharp decrease in blood flow to the testicle and its epididymis. Changes occur in the tissues of the male gland associated with oxygen starvation and lack of nutrients. The degree of change is determined by the degree of torsion and the duration of this condition. The length of the spermatic cord also plays an important role (the degree of destruction will be greater with a short cord). If medical assistance is not provided, then after 6-9 hours irreversible damage develops - testicular necrosis.
Complications of the pathology are testicular necrosis, testicular gangrene, scrotal abscess, scrotal gangrene, chronic inflammation of the epididymis.
What happens normally?
The blood supply to the testicle occurs through the spermatic cord, which comes from the abdomen through the inguinal canal, then enters the scrotum. The spermatic cord contains the vas deferens, through which sperm is released. Although the testicle has several sources of blood supply, all of which pass through the spermatic cord, disruption of this source of blood supply leads to complete ischemia of the testicle.
Testicles are organs located in the scrotum under the penis. Both testicles should be approximately the same size. Asymmetrical enlargement, especially if it occurs suddenly, is most likely pathological.
Also, the color of the skin on both sides of the scrotum should be the same. Any change in color, especially redness or darkening, suggests the presence of pathology. Normally, the testicles are painless; any pain or discomfort should force a person to see a doctor, even if there is no swelling or change in skin color.
Diagnosis of testicular torsion
If torsion is suspected, a careful examination of the patient and palpation of the organ suspected of pathology is carried out. Based on the clinical picture, a preliminary diagnosis can be made.
To confirm it, an ultrasound of the scrotal organs with Doppler and diaphanoscopy are performed.
Diagnosis of testicular torsion includes orchitis, epididymitis, trauma and some other abnormalities. Torsion is distinguished from orchitis by its more acute onset, and from epididymitis by the nature of the pain syndrome (the pain intensifies when the scrotum is raised, and with epididymitis it weakens). The cremasteric reflex practically disappears during torsion, in contrast to inflammatory processes of the testicle. Less often it is necessary to carry out a differential diagnosis of testicular torsion with its hydrocele, strangulated by an inguinal hernia.
With torsion, laboratory tests are of little value. The same cannot be said about instrumental studies. The most indicative is an ultrasound examination with Doppler ultrasound - it detects all blood supply disturbances in the organ. Dynamic testicular scintigraphy can also be performed. Unfortunately, it is not widely available. Endoscopic diagnosis is rarely practiced.
In difficult cases, when there is doubt about the diagnosis or in emergency situations, as well as when receiving ambiguous results from instrumental studies, they resort to diagnostic dissection of the scrotum and revision of the testicle.
Is it necessary to install a testicular prosthesis?
A testicular prosthesis is used to replace a lost testicle. There are hard, soft, polymer and silicone prostheses.
Most often, a prosthesis is installed when a person has already reached puberty. A smaller prosthesis in boys requires repeat surgery to change the prosthesis. This operation cannot be performed during removal of the dead testicle, but only several months later. The decision to install a prosthesis is purely personal and is made by the patient in consultation with a urologist.
Treatment of testicular torsion
When torsion occurs, irreversible changes occur within 6–8 hours, so immediate emergency medical care is required. In mild cases, closed detorsion (turning the testicle through the skin of the scrotum) helps. More severe cases require surgery. If too much time has passed and the tissue of the testicle has died, only its removal will help.
If treatment is carried out in a timely manner, the prognosis is good. Detorsion done in the first 6 hours after torsion leads to complete recovery in 90% of cases. If more than a day has passed, then, most likely, you will have to resort to orchiectomy.
Testicular detorsion closed
In the early stages of pathology development, conservative treatment - closed testicular detorsion - can help. This is the rotation of the testicle in the right direction, carried out without incisions, through the skin of the scrotum. It may be necessary to repeat the manipulation more than once. If the reversal is successful, the pain goes away or is greatly reduced. The testicle descends to the bottom of the scrotum and occupies an equal position with the other.
However, detorsion is not a panacea. Even if it led to success and eliminated the symptoms, it is necessary to fix the testicle to the bottom of the scrotum as soon as possible. Otherwise, a relapse is possible.
If it is impossible to quickly perform fixation after detorsion, drugs are prescribed to increase microcirculation, and novocaine blockades of the spermatic cord are performed.
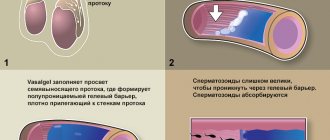
Completely conservative therapy for testicular torsion is dangerous due to the accumulation of sperm antibodies in the patient’s body (after all, the blood-testis barrier is broken during torsion), damage to the other testicle and infertility. Therefore, all patients after detorsion are prescribed heparin, aspirin, and occasionally steroids.
Open testicular detorsion
If it happens that detorsion fails, or testicular torsion exists for a long time, emergency surgical intervention is needed. After a skin incision, the condition of the testicle is inspected and open detorsion is performed, then the organ is fixed to the bottom of the scrotum. If the audit showed an unsatisfactory condition of the testicle due to a long lack of blood circulation, they resort to warming the organ with a warm isotonic solution, and a mixture of antispasmodic and analgesic, as well as a hemostatic drug, is poured into the spermatic cord.
If this does not help or signs of necrosis are clearly visible, the testicle is removed (orchiectomy).
Rehabilitation after treatment
Children, as a rule, spend no more than 2 days in a hospital setting. After discharge, the child must:
- dynamic observation by a urologist with ultrasound control;
- limit physical activity and strength training for 2 months;
- take medications prescribed by your doctor to prevent infection;
- exclude cycling, horses and other activities that can injure the scrotum for 2-3 months.
The sutures are removed a week after discharge, and a month later it will be necessary to undergo a follow-up examination using ultrasound and general clinical tests.
Symptoms of the disease
Intravaginal testicular torsion begins with sudden, unilateral scrotal pain followed by swelling of the scrotum and/or groin area. The pain may decrease when complete necrosis of the testicle occurs. Testicular torsion can occur during sports or physical activity, can be associated with injury, or can develop spontaneously.
About one third of patients also have gastrointestinal symptoms such as nausea and vomiting. In pediatric practice, nausea and vomiting have a positive predictive value greater than 96%. Duration of pain less than 6 hours, fever, vomiting, history of trauma or physical activity, absence of the cremasteric reflex, and abnormal testicular position are all features strongly suggestive of a diagnosis of testicular torsion.
Patients rarely report difficulty or painful urination. In some patients, scrotal trauma or other medical conditions, such as testicular hydatid torsion or epididymitis orchiepididymitis, may precede the onset of testicular torsion. Occasionally, patients may describe previous episodes of recurrent acute spontaneous scrotal pain. This history is primarily suggestive of a diagnosis of testicular torsion.
What other torsions are possible?
Epididymal torsion needs to be mentioned separately because... in younger boys it is more common than testicular torsion itself. It can occur in older age groups, but much less frequently. As with testicular torsion, there are no predisposing factors for this type of torsion, but it can occur at any time. Testicular appendages do not have a special function in men. They are located in the upper pole of the testicle. They have their own blood supply and can also become twisted, leading to a heart attack. Such patients have pain, but it is usually less severe than with testicular torsion and decreases within a few days. Often the diagnosis is made during surgery, because This condition is clinically very similar to testicular torsion.
In some cases, a urologist can make this diagnosis through physical examination or with the help of X-ray or nuclear magnetic resonance imaging. If the diagnosis is beyond doubt and testicular torsion is excluded, surgery can be avoided; pain and swelling disappear within a few days. If there is any doubt, it is necessary to exclude testicular torsion surgically.
For a long time, treatment tactics for testicular torsion were not urgent, because the very concept of “acute scrotal syndrome” did not oblige doctors to take emergency measures and implied conservative treatment of “nonspecific acute orchitis” [1,2]. Only a few patients underwent emergency intervention. A revision of these provisions occurred in domestic urology in the late 1970s and early 1980s. [3-5], abroad somewhat earlier - in the 50-60s. XX century [6,7].
An indication for emergency surgical intervention is any situation where testicular inversion cannot be excluded clinically and (or) there are characteristic changes recorded during ultrasound examination (US) and/or Doppler ultrasound (USDG) of the scrotal organs [8]. In the case of suspected torsion of a single testicle, the surgeon’s tactics should be as active as possible, even with negative results of additional research methods, because It has not been proven that instrumental methods or clinical assessment have greater accuracy [8]. According to V-B Shill et al., the experience of a specialist plays a large role in the success of diagnostics, both clinical and ultrasound [9].
The surgical intervention itself, from a surgical point of view, does not represent any significant complexity and is one of the simplest technically in operative urology. However, the tactical situation that arises both before the operation and after relief of the urgency of the condition poses a number of difficult questions for the urologist, among which the most pressing today are the reduction of preoperative ischemia of the organ, which is especially important if it is impossible to perform the operation immediately, as well as testicular fixation and prosthetics gonads.
These issues in testicular volvulus surgery are the most controversial and ambiguous according to the literature.
Despite the urgency of the condition, surgical intervention requires time for preoperative preparation. In conditions where this period cannot be reduced to a minimum for organizational, clinical or other reasons, it becomes important to find ways to reduce the negative impact of the temporary factor on the reproductive function of the gonad [10].
For this, a number of authors have proposed testicular hypothermia using a heating pad with ice [10,11,12]. AG Lewis uses this method in the emergency department before surgery [11]. An experiment on animals showed that hypothermia increases the survival rate of the gonad with a torsion period of 6 hours from 8-25% to 85-90% [12]. In a clinical study by M. Kallerhoff et al. it has been proven that a decrease in testicular temperature to 15°C increases the period of onset of necrobiotic changes in the gonad from two to six hours [10]. However, this method is not widely used in practical medicine.
The priority method for reducing testicular ischemia before surgery is closed manual detorsion [9]. However, opinions on the feasibility, indications for implementation and effectiveness of closed manual detorsion are extremely polar. The methodology for its implementation is described in detail in the literature [9,13,2]. According to V-B Shill et al., this manipulation is simple and effective [9]. Data on the effectiveness of closed manual detorsion are contradictory; there are both positive [14,15] and negative reviews [16]. However, all researchers agree that the effectiveness of the method is inversely proportional to the duration of torsion [9].
RH Jefferson et al. indicate that the effectiveness of the manual detorsion procedure is up to 80%, but note a large number of residual torsion - 28% [15]. AM de Vylder et al. note an increase in the frequency of preservation of the gonad up to 90% when using the technique in a complex of surgical measures to restore blood circulation to the testicle (blockade of the spermatic cord, warming the gonad) [14]. T. Snodgrass notes the effectiveness of the method in 32% of observations without residual torsion [16]. On the contrary, A.V. Bukhmin et al. indicate the extremely low efficiency of this technique (0.9%) [17].
There is a variety of data on the results of closed manual detorsion in practical work. I.Sh. Er-gashev completely abandoned attempts to perform it, believing that the direction of torsion is unpredictable in 26% of cases and such manipulation can only aggravate testicular ischemia [18]. At the same time, S.Yu. Komarova et al. It was also performed by 30.4% of patients, mainly within a day from the onset of the disease, obtaining an effective result. [19].
Due to the possibility of residual torsion, surgery has been proposed as a mandatory component for controlling detorsion [20]. In recent years, this position is not absolutely categorical; it is proposed to use Doppler ultrasound to control detorsion and, when visualizing testicular blood flow, to refrain from emergency surgical intervention [21,22].
Determining the indications for fixation of the testicle during inversion, as well as fixation of the contralateral organ, and the method of performing fixation is one of the most controversial issues in inversion surgery, on which a polarity of opinions remains to this day.
There is a consensus in determining the indications for testicular fixation [23]. The justification for testicular fixation is most often the presence of bilateral synchronous and asynchronous inversion and the identification of anatomical defects of the ligamentous apparatus of the scrotum [23]. However, one should also take into account the fact that the incidence of bilateral testicular volvulus is relatively low (6-7%) [17]. The anatomical defects are not symmetrical in all cases - at autopsies, an anomaly of the location of the testicle of the “bell tongue” type is found in 12% of cases, and in 66% it is bilateral [24]. Data on mesorchial torsion are also ambiguous - the frequency of its occurrence, according to various authors, is 25-100% [25,26].
Studies have been published that completely deny the need for testicular fixation [1]. There is an opinion about the need to fix the testicle only if it is the only one [27].
The wider dissemination of indications for fixation in practice is associated with the publication of study results showing the absence of a negative effect from the operation [28].
KM Broberick et al. when analyzing data from 121 respondents from European clinics, it was noted that fixation of the contralateral testicle is performed by 93-96% of pediatric urologists [29]. L. Harper et al. presented data on fixation of the contralateral testicle in 16 of 28 pediatric urology departments in France after extravaginal torsion and in all cases after intravaginal torsion [8]. C. Bolln et al., having conducted a survey of employees of pediatric surgery clinics in Great Britain and Ireland, received positive opinions about testicular fixation, both on the interested and contralateral sides in 95% of cases [30].
The need for bilateral fixation is included in the basic principles of surgical treatment of testicular volvulus, formulated in the fundamental study of I. Pearce in 2002. The author also pointed out that there is no need for prophylactic fixation of the testicle if surgical intervention is not performed for testicular torsion [31].
Over the past years, there has been a consensus among authors about the need for bilateral fixation in all cases, either simultaneously with the primary operation or delayed [8,23,30,32-38]. However, this opinion remains controversial and continues to be discussed.
When testicular torsion occurs in newborns, the issue of fixation becomes even more acute, because at this age, the frequency of bilateral volvulus is significantly higher [33]. This position is also confirmed by the fact that inspection often reveals signs of ischemia of the contralateral testicle in the absence of obvious testicular volvulus [23,39-41]. Taking into account the above data, N. Biplah et al. believe that fixation of the contralateral testicle is the same urgent surgical measure as the elimination of volvulus [33].
An indirect justification for the need to fix the gonad during torsion is the description of cases of testicular torsion in members of the same family [42]. It is also advisable to perform fixation in patients of older age groups [43].
The methods for performing orchiopexy are varied, but come down to four main methods.
Method I: application of fixing sutures made of non-absorbable suture material. The most commonly used fixation is a 4/0 nonabsorbable suture with three sutures to secure the testis [44].
Method II: eversion of the tunica vaginalis of the testicle using the “dartos pouch” technique with or without fixation with sutures. The most widely used technique in practice was proposed by TS Morse. The essence of the technique is as follows: the edges of the tunica vaginalis are sutured to the tunica albuginea with six 4/0 sutures using non-absorbable suture material, creating a window in the tunica measuring 1.5*2.0 cm, which is sufficient for adhesion of the testicular capsule and its fixation in the tunica
[45]. The TS Morse technique also avoids suture fixation with potential damage to the tunica albuginea and disruption of the blood-testis barrier compared to the Jaboulay technique [46].
The Jaboulay-Winkelman method of testicular fixation, which provides fixation due to the adhesion of the testicle to the everted tunica vaginalis, has found its application. AM de Vylder considered it the operation of choice [47], but in other studies this technique was found to be inappropriate [31].
An alternative to the above methods is the Shoemaker operation, which is widely used in cryptorchidism surgery. The use of this operation to prevent testicular volvulus was reported by JF Redman et al. [48]. At the same time, according to the opinions of a number of authors, its use is advisable only when the testicle is torsion in the inguinal canal, when, simultaneously with detorsion, the testicle is brought down into the scrotum [31,46].
III method: use of special cauterizing or coagulating devices. J. Chimenge proposed a fixation technique using a Lancet laser scalpel, according to which superficial deserosis of the tunica albuginea is carried out without damaging the parenchyma at the sites of sutures [49].
IV method: chemical sclerotherapy, for which talc and tetracycline are most often used. At the same time, LE Robrigues et al. noted that this technique is less effective than when using mechanical fixation of the testicle with suture material [50].
It must be emphasized that there is a possibility of recurrence of torsion when using any of the proposed methods. TS Morse analyzed 22 cases of recurrent torsion after testicular fixation and found that non-absorbable suture material was used in three cases, and absorbable in 19 cases [51]. He also described cases of recurrent torsion after using the “dartos pouch” technique, but, according to the data presented, they are observed much less frequently [52]. C. Bollin et al. noted recurrence of torsion with a very high frequency - 16 cases per 95 fixations, but did not indicate the method of fixation [30]. Some researchers note reliable fixation only when using the “dartos pouch” method with fixation with non-absorbable sutures [50,53]. S. Blaut et al. report the possibility of torsion recurrence regardless of the fixation method [34].
Any method of testicular fixation has advantages and disadvantages, which are discussed in the literature [31]. Most often they are associated with the use of suture material and directly correlate with the reliability of fixation [33,51]. According to TS Morse, the use of absorbable material leads to the formation of ligature granulomas and, as a consequence, to inflammation and fibrosis in the scrotal cavity, while the “dartos pouch” technique provides sufficient adhesion for fixation of the testicle [51]. There is another opinion, according to which the “dartos pouch” technique causes an excessive adhesive process in the scrotal cavity [24]. Some publications indicate cases of testicular necrosis after fixation, which is likely due to technical errors during the operation [8].
There is also no consensus on the timing of testicular fixation. If, with regard to fixation of the “suffering” gonad, the prevailing opinion is that it is necessary to fix it simultaneously with detorsion or in the near future after it, then the issue of the timing of fixation of the contralateral testicle is actively discussed [30,31,34]. So, G.N. Rumyantseva et al. suggest performing testicular fixation on the contralateral side 1-2 weeks after the acute episode [44]. A number of authors perform the operation delayed after 2-3 months [29].
Testicular endoprosthetics is a new direction both in testicular volvulus surgery and in pediatric and adolescent reconstructive andrology in general. The need for testicular replacement is beyond doubt because implantation is considered an important procedure for restoring an aesthetically acceptable scrotum and preventing the child from experiencing the psychological consequences of having an “empty” scrotum [9]. The role of this operation as the final stage of patient rehabilitation is great[19].
The priority of research in this direction belongs to adult urologists. The first publications on testicular prosthetics related to adults were published in the 30s of the 20th century [54,55]. Prosthetics were performed for various reasons, but testicular inversion was not the leading one among them. Already in the 1980s, significant foreign experience in performing such operations had been accumulated. The leadership in this direction belongs to SMD Marshal [45]. The author collected data on 2533 cases of testicular replacement, of which 527 cases were for testicular inversion in children and adolescents. According to his data, testicular inversion was the reason for prosthetics in 17% of cases; testicular hypoplasia and anorchism were presented - in 35%, testicular tumors - in 23%, orchiectomy for prostate cancer - in 16%, epididymitis and orchitis - in (8%), trauma - in 1%. J. Adshead et al. presented a slightly smaller study size - 424 patients [56]. In the domestic literature, the greatest experience in testicular replacement in children and adolescents belongs to A.B. Okulov (224 patients under the age of 18 years) [13]. It should be noted that the number of publications on testicular prosthetics is not large, both in domestic and foreign literature.
By now, testicular replacement has firmly taken its place in reconstructive genital surgery; the feasibility of its implementation for psychological and cosmetic reasons has been proven and is no longer subject to debate. Meanwhile, this problem leaves many unresolved questions, such as the optimal age for prosthetics, selection of implant sizes, types of implants, prosthetic techniques, complications during prosthetics, satisfaction with the result. All these questions require further research.
The issue of timing of prosthetics is still being discussed. A. Brandon considers it possible to perform testicular prosthetic surgery simultaneously with its removal, but only in the absence of inflammatory changes in the membranes of the organ [57]. Other authors suggest delaying prosthetics, after 3-6 months, when the inflammatory process in the testicular membranes stops and a scar on the scrotum has formed, which is important when using the inguinal approach[13].
There is an opinion about the advisability of prosthetics in two stages, when an implant of the smallest possible size is installed soon after removal of the own testicle, and subsequently prosthetics is performed with an implant corresponding to the own second testicle [58]. The technique, on the one hand, makes it possible to place a second implant in a “prepared” scrotum of sufficient volume without tension on the integument and disruption of its trophism, and on the other hand, it has negative aspects - it is traumatic, the need for repeated intervention and the isolation of a smaller implant from the adhesions in the cavity with the risk of damage to the membranes [ 19]. A number of authors prefer to implant a prosthesis corresponding to the size of their own testicle in adolescence, while determining the size of the implant using ultrasound data [59].
At the same time PJ. Turek believes that it is necessary to be critical of the size of the testicle according to ultrasound data and implant a slightly larger prosthesis, because the own testicle is located in membranes that increase its volume, and the implantation of a testicular prosthesis is carried out almost under the skin of the scrotum [58].
Most authors indicate the advisability of implanting a testicular prosthesis at the age of 13-17 years [19,59,60], A.B. Okulov, performing operations in the age range from 7 to 18 years, also considers the optimal age to be 13-17 years [13]. Yu.Yu. Madykin et al. Testicular prosthesis is implanted in patients starting from the age of 17; this is probably due to the fact that the author operates mainly on adult patients [59]. S.Yu. Komarova et al. Testicular prosthetics are performed at any age, but subsequently the implant is replaced with one that corresponds to the adult age norm. The authors also point out the need to take into account, when choosing the size of an implant, in addition to the size of one’s own testicle, the general proportions of the genital organs, primarily the size of the penis [19].
There are currently two main types of implants:
1. Liquid implants placed in the scrotum by puncture. The composition, common in practice, was proposed by A.B. Okulov and is tridecaethylene glycol dimethacrylate in combination with water in ratios of 13-24%: 64-86.8% [13]. G.A. Makarov et al. It was proposed to use sterile polyacrylamide hydrogel (PAAG) of 6th degree density as an implant-filler [60]. Silicone rubber, proposed by N.A., was used. Plate [61]. PJ Turek et al. a prosthetic method was used using a reservoir filled with saline solution [58].
Previously, methods were proposed using paraffin (Volpyan I.G., 1947), foam sponge (Sayfutdinov R.A., 1968), AKR-10 plastic (Mukhtarov A.M., Murvanidze D.D., 1988) - all today they have only historical significance [60].
2. Silicone implants having a certain shape. The most widely used implants in clinical practice are the following (Russia, Mytishchi), ZAO MIT (Russia, Zheleznodorozhny), LLC PKO Kauchuk (Russia, Rostov-on-Don), Mertor/Coloplast (USA), Eurosilicone 26cc ( USA). Currently, the vast majority of prosthetic operations are performed with silicone implants [19,59,62].
Of the existing methods for installing silicone implants, two stand out in principle: implantation through the inguinal [56,62] and scrotal approaches [59]. In the first case, access is carried out along the inguinal fold, the formation of a tunnel into the scrotum, if the atrophied testicle remains there - orchofuniculectomy with high ligation of the spermatic cord and implantation of the prosthesis into the prepared cavity [62]. In the second case, access is made to the scrotal cavity directly through its integument [59].
The technical implementation of the methods is described in detail in the literature, both of them have both positive and negative sides (Table 1).
Table 1. Comparison of testicular replacement techniques [45]
| Criterion | Inguinal access | Scrotal access |
| Removal of the spermatic cord to the internal inguinal ring | Possible and technically easy to implement | Impossible |
| Difficulties of hemostasis in the scrotal cavity | Possible | Virtually none |
| Traumaticity | Big | Smaller |
| Tightness of the scrotal cavity | Hermetically sealed | No tightness |
| Risk of implant infection | Minimum | Available |
| Push effect | Available | Virtually absent |
| Trophic disorders of the scrotum | Possible | Not likely |
| Cosmetics | A scar remains in the groin area | The scar on the scrotum is almost invisible |
The paucity of publications on testicular prosthetics leaves the issue of complications of prosthetics insufficiently covered, however, it is directly related to implantation techniques. Thus, the risk of implant rejection and infection of the surgical site is significantly higher when using the scrotal approach, because in this case, there is incomplete sealing of the seams and contact of the prosthesis with the external environment [59]. Some authors have presented cases of silicone implant destruction [63].
Table 2 presents complications of testicular replacement according to various authors.
Table 2. Complications of testicular replacement
| Author | Access | Rejection, % | Infection, % | Hematoma, % | Suppuration, % | Implant shrinkage, % | Pain syndrome, % | Total,% |
| SMD Marshal 1986 | inguinal | 2,20% | 1,00% | 1,30% | 0,50% | — | 1,20% | 6,20% |
| scrotal | 3,50% | 1% | 1% | 0,50% | — | 1% | 7,00% | |
| L. Incrocci, 1999 | inguinal | — | — | — | 3,30% | — | 3,30% | 28,20% |
| AP Doherty, 2000 | inguinal | — | — | — | — | 3,10% | — | 6,60% |
| Yu.Yu. Madykin, 2012 | scrotal | 5,80% | 11,40% | — | 5,80% | 3,20% | 2% | 3,10% |
An important aspect of testicular replacement is the realistic outcome expected by the patient and satisfaction with the result of the operation. According to foreign authors, it does not occur in all cases [56,45]. According to survey data, the percentage of patients satisfied with the results of the operation is 65-70% of cases, in 20% of cases relative satisfaction is noted [62]. Dissatisfaction with the results is associated with complications and, to a greater extent, with inflated expectations from prosthetics. About half of the patients refuse reimplantation of the prosthesis after its rejection, preferring to have a cosmetic defect of the scrotum rather than undergo a second operation for fear of failure [59].
Thus, the problems of surgical tactics for testicular torsion remain relevant and controversial to this day. There is no uniform protocol for the management of patients after relief of an urgent condition until the final stage of rehabilitation. The data available in the literature are insufficient to evaluate and compare the effectiveness of existing methods. Further research is required in this area of treatment and rehabilitation of pediatric patients with testicular torsion.
LITERATURE
1. Bairov A.G., Aleksandrov S.V., Kashin A.S., Zaitseva N.A., Polyakov P.N. Experience in treating patients with acute diseases of the scrotal organs. Collection of materials from the IV All-Russian Conference with international participation “Emergency Pediatric Surgery and Traumatology” 2021, February 14-15, Moscow. Moscow: 2021. 377 p.
2. Yudin Ya.B., Sakhovsky A.F. Acute testicular diseases in children. Novokuznetsk: 1979. 16 p.
3. Soloviev A.E. Diagnosis and treatment of acute testicular diseases in childhood: Doctor of Medical Sciences thesis. Moscow: 1983. 39 p.
4. Soloviev A.E. Treatment of acute testicular diseases in childhood. Clinical Surgery 1988;(6):30-34.
5. Soloviev A.E. Pathogenesis of testicular atrophy due to torsion of the spermatic cord in childhood. Bulletin of surgery named after. Grekova. 1982;128(6):99-102.
6. Favorito LA, Cavalcante AG, Costa WS. Anatomic aspects of epididymis and tunica vaginalis in patients with testicular torsion. Int Braz J Urol 2004; (30):420-424. doi: https://dx.doi.org/10.1590/S1677-55382004000500014.
7. Prando D. Torsion of spermatic cord: the man gray - scale and Doppler sonographic signs. Abdom Imaging 2009; 34 (5): 648 – 661. doi: 10.1007/s00261-008-9449-8.
8. Harper L, Gatibelsa ME, Michel JL, Bouty A, Sauvat F. The return of the solitary testis. J Pediatr Urol 2011; 7 (5): 534-537. doi: https://dx.doi.org/10.1016/j.jpurol.2010.08.003.
9. Schill W-B., Comhair F., Hargreave E. Clinical andrology. [Transl. from English]. Moscow: GEOTAR-Media; 2011.800 p.
10. Kallerhoff M, Gross AJ, Botefur IC. The influence of temperature on changes in pH, lactate and morphology during testicular ischemia. BJU 1996;(78): 440 – 445. doi: 10.1046/j.1464-410X.1996.00138.x.
11. Lewis AG, Bukowski TP, Jarvis PD, Wacksman J, Sheldon CA. Evaluation of acute scrotum in the emergency department. J Pediatr Surg 1995;(30):277-282. doi: https://dx.doi.org/10.1016/0022-3468(95)90574-X.
12. Miller DC, Peron SE, Keck RW, Kropp KA. Effect of hypothermia on tedticular ischemia. J Urol 1990;(143): 1046 -1048.
13. Okulov A.B. Surgical tactics for diseases of the reproductive system in children: abstract. Dissertation of Doctor of Medical Sciences. Moscow; 2001.77 p.
14. de Vylder AM, Breeuwsma AJ, van Driel MF Torsion of the spermatic cord after orchiopexy. J Pediatr Urol 2006; 2(5): 497-499. doi: https://dx.doi.org/10.1016/j.jpurol.2005.09.011.
15. Jefferson RH, Perez LM, Joseph DB. Critical analysis of the clinical presentation of acute scrotum; a 9-year experience at a single institution. J Urol 1998; (158): 1198-1200.
18. Snodgrass T. Warren. Pediatric Urology. Evidence for Optimal Patient Management. New York: Springer; 2013.286 rub.
17. Bukhmin A.V., Nikitin I.V. Acute scrotum in children. Proceedings of the VIII International Congress of Urologists. Kharkiv. 2000. pp. 305-314
18. Ergashev I.Sh., Khakomov T.P. Diagnosis and treatment tactics for swollen scrotum syndrome in children. Pediatric Surgery 2010;(3):23-26. doi: 0.12955/emhpj.v8i1.528.
19. Komarova S.Yu., Gaidysheva E.V., Timoshinov M.Yu., Ekimov M.N., Smirnova S.E. Testicular replacement in children. Collection of materials from the VI School of Pediatric Urology and Andrology. 2021 April 6-7 Moscow. Moscow: publishing house; 2021. pp. 23-24.
20. Pulatov A.T., Karaseva O.V., Medvedev I.V. On conservative correction of testicular torsion in children. Pediatric Surgery 2004; (2):6-10.
21. Garel L, Dudois J, Azzie G. Preoperative manual detorsion of the spermatic cord with Doppler ultrasound monitoring in patients with intravaginal acute testicular torsion. Pe-diatr Radiol 2000;30 (1):41 – 44. doi: 10.100 7/s002470050012.
22. Kiesling Jr VJ, Schroeder DE, Pauljev P, Hull J. Spermatic cord block and manual reduction: primary theatment for spermatic cord torsion. J Urol 1984;(132):921 – 923.
23. Kaye JD, Shapiro EY, Levitt SB. Parenchymal echo texture predicts testicular salvage after torsion: potential impact on the need for emergent exploration. J Urol 2008;(180):1733-1736. doi: https://dx.doi.org/10.1016/j.juro.2008.03.104.
24. Caesar RE, Kaplan GW. The incidence of the cremasteric reflex in normal boys. J Urol 1994; (152): 779 – 780. doi: https://dx.doi.org/10.1016/S0090-4295(94)80020-0.
25. Anderson J, Williamson R. Testicular torsion in Bristol: a 25-year revive. Br J Surg 1988;(75):988-992. doi: 10.1002/bjs.1800751015.
26. Ransler CW, Allen TD. Torsion of the spermatic cord. Urol Clin North Am 1982;(9): 245-250.
27. Mishriki SF, Winkle DC, Frank JD. Fixation of a single test: some facts and figures. Br J Urol 1992; 69 (3): 311-313. doi: 10.1111/j.1464-410X.1992.tb15535.x.
28. Hadziselimovic F, Snyder H, Duckett J. Testicular histology in children with unilateral testicular torsion. J Urol 1986; (136): 208 - 210.
29. Broberick KM, Martin BG, Herndon CD, Joseph DB, Kitchens DM. The current state of surgical practice for neonatal torsion: a survey of pediatric urologists. J Pediatr Urol 2013; (10): 339-342. doi: https://dx.doi.org/10.1016/j.jpurol.2012.12.010.
30. Bolln C, Driver CP, Youngson G. Operative management of testicular torsion: Current practice within the UK and Ireland. J Pediatr Urol 2006; 2 (3): 190 – 193. doi: https://dx.doi.org/10.1016/j.jpurol.2005.07.006.
31. Pearce I. Suspected testicular torsion: a survey of clinical practice in North West England. J Royal Soc. Med 2002; (95): 247 - 249.
32. Ahmed H, Al-Salem. Intrauterine testicular torsion: a surgical emergency. J Pediatr Surg 2007; 42 (11): 1887 - 1891.
3. Biplah N, Feilim LM. Neonatal testicular torsion: a systematic literature review. Pediatr Surg Int 2011; (27): 1037 – 1040. doi: 10.1007/s00383-011-2945-x.
34. Blaut S, Steinbach F, Tittel B, Durig E. Torsion of the Spermatic Cord after Prophylactic Orchidopexy. Akteelle Urol 2008; (39): 147-149. DOI: 10.1055/s-2007-980146
35. Brandt MT, Sheldon CA, Wacksman J, Matthews P. Prenatal testicular torsion: principles of management. J Urol 1992;(147):670-672. DOI: https://dx.doi.org/10.1016/0022-3468(92)90827-T
36. Kashif M, Riazulhag M, Hussain N. Perinatal testicular torsion: some facts and figures. Med Forum 2009;20 (1): 28 – 31. DOI: https://dx.doi.org/10.5489/cuaj.803
37. Olguner M, Akgur FM, Aktug T, Derebek E. Bilateral asynchronous perinatal testicular torsion: a case report. J Pediatr Surg 2000;(35): 1348 – 1349. DOI: https://dx.doi.org/10.1053/jpsu.2000.9330
38. Pinto KJ, Noe HN, Jerkins GR. Management f neonatal testicular torsion. J Urol 1997; (158): 1196 - 1197.
39. John CM, Kooper G, Mathew DE, Ahmed S, Kenny SE. Neonatal testicular torsion - a lost cause? Acta Paediatr 2008;97(4):502-504. DOI: 10.1111/j.1651-2227.2008.00701.x
40. Stone KT, Kass EJ, Cacciarelli AA, Gibson DP. Management of suspected antenatal torsion: what is the best strategy? J Urol 1995; (153): 782 - 784. DOI: https://dx.doi.org/10.1016/S0022-5347(01)67720-6
41. Yerkes EB, Robertson FM, Gitlin J. Management of perinatal torsion: today, tomorrow or never? Urol 2005;174: 1579-1582. DOI:https://dx.doi.org/10.1097/01.ju.0000179542.05953.11
42. Okeke LI, Ikuerovo OS. Familial torsion of the testis. Int Urol Nephrol 2006;38:641-642. DOI: 10.1007/s11255-006-0049-7
43. Brandon A, Adam J Ball, Desai A. Delayed presentation of acute scrotum: a rare age for torsion. Intern EmergMed 2010;( 5):553-554. DOI: 10.1007/s11739-010-0378-5
44. Rumyantseva G.N., Kartashev V.N., Avrasin A.L., Chimenge Zh. Treatment tactics for testicular volvulus in children. 3rd Congress “Modern technologies in pediatrics and pediatric surgery”. 2004 October 20-23, Moscow. M.: 2004. 556 p.
45. Marshal SMD. Potential problems with testicular prostheses. Urology 1986;28(5):388-390.
46. Lent V, Stephani A. Eversion of the tunica vaginalis for prophylaxis of testicular torsion recurrences. J Urol 1993;(150):1417-1421. DOI: https://dx.doi.org/10.1016/ S0022-5347(01)67276-8
47. de Vylder AM, Breeuwsma AJ, van Driel MF. Torsion of the sprrmatic cord after orchiopexy. J Pediatr Urol 2006; 2(5): 497-499. DOI:https://dx.doi.org/10.1016/j.jpurol.2005.09.011
48. Redman JF, Barthold JS. A technique for atraumatic scrotal pouch orchiopexy in the management of testicular torsion. J Urol 1995; 154 (5): 1511 - 1512. DOI: https://dx.doi.org/10.1016/S0022-5347(01)66918-0 49. Chimenge J. Application of modern technologies in the diagnosis and treatment of acute diseases of the scrotal organs: diss. . ... Doctor of Medical Sciences. Tver: 2003.17 p.
50. Robrigues LE, Kaplan GW. An experimental study of methods to produce in-trascrotal testicular fixation. J Urol 1988; (139): 565 - 567. DOI: 10.1007/BF00326694
51. Morse TS, Hollabaugh RS. The “window” orchiopexy for prevention of testicular torsion. J Pediatr Surg. 1977; (12): 237.DOI: https://dx.doi.org/10.1016/ S0022-3468(77)80014-6
52. Thurston A, Whitaker R. Torsion of testis after previous testicular surge. Br J Surg 1983;(70):217-230. DOI: 10.1002/bjs. 1800700410
53. Bellindger MF, Abromowitz H, Brantley S, Marschall G. Orchidopexy: an experimental study of the effect of surgical technique on testicular histology. J Urol 1989; (142): 553-555.
54. Girsdansky J, Nerwman HF. Use of a vitallium testicular implant. Surg 1939; (1):21DOI: https://dx.doi.org/10.1016/S0002-9610(41)90676-1
55. Venable C, Stuck W. Testicular implants. Ann Surg 1937;(105):917.
56. Adshead J, Khoubehi B, Wood J, Rustin G. Testicular implants and patient satisfaction: a guestion-based study of men after orchidectomy for testicular cancer. BJUInt 2001;(88):559 - 562 DOI:10.1046/j.1464-4096.2001.02392.x
57. Knight PJ, Vassy LE. The diagnosis and treatment of the acute scrotum in children and abolescents. Ann Surg 1984; (200): 664-673.
58. Turek PJ. Master and The Testicular Prosthesis Group. Safety and effectiveness of a new saline filled testicular prosthesis. J Urol 2004;(172):1427- 1430. DOI: https://dx.doi.org/10.1097/01.ju.0000139718.09510.a4
59. Madykin Yu.Yu., Zolotukhin O.V., Firsov O.V. About some features of testicular prosthetics. Materials of the 8th Congress "Men's Health". 2012 April 26-28, Yerevan. Yerevan: ed.; 2012. pp. 73-74.
60. Makarov G.A., Chepurnoy G.I. Method of testicular replacement for monorchism and anorchism [Internet]. https://www.findpatent.ru/patent/223/2231300.html (Date of visit 05.10.17)
61. Plate N.A. Synthetic polymers for medical purposes. Tashkent: Fan; 1984. pp. 30-31.
62. Lawrentschuk N, Webb R David. Inserting testicular prostheses: a new surgical technology for difficult cases. BJU Int 2005;(95):1111-1114. DOI: 10.1111/j.1464-410X.2005.05476.x
63. Doherty AP, Mannion BM, Moss JJ, Ockrim JL, Christmas TJ. Spread of silicone to inguinal lymph nodes from a leaking testicular prosthesis: a cause for chronic fatigue? BJU Int 2000; (86): 1090. DOI: 10.1046/j.1464-410x.2000.00961.x
| Attached file | Size |
| 2.18 MB |
‹ A modern view of the physiological effects of testosterone in men Up Comparison of urination parameters in different body positions ›