General signs of cutaneous vasculitis
The rash with cutaneous vasculitis is polymorphic, with elements of inflammation
. Despite the different symptoms, all these angiitis have similar features:
- an allergic rash with elements of inflammation, swelling, subsequently with hemorrhages into the skin and tissue necrosis;
- the elements of the rash are not the same in shape and size, their polymorphism is observed;
- rashes are symmetrical;
- the rash first appears or is most severe on the legs;
- tendency to acute inflammation and frequent relapses;
- combination of angiitis with vascular or allergic diseases.
Symptoms of the disease.
Allergic skin vasculitis (depending on the depth of the damaging process) is divided into:
- Superficial
- Deep
Symptoms of allergic skin vasculitis:
- Purpura – vascular spots in areas of hemorrhage
- Ulcers
- Vascular spots
- Papules are pink nodular lumps of skin
- Bubbles with a diameter greater than 5 mm
- Subcutaneous nodes
- Chronic urticaria
- Rash
All of the above symptoms are usually accompanied by general malaise, loss of appetite, itching and burning of the skin, fever and increased temperature.
Mechanism of development (pathogenesis) of cutaneous vasculitis
The disease is of an immunocomplex nature. This means that the walls of blood vessels are affected by aggregates (immune complexes) consisting of protective antibodies and various external harmful agents - antigens.
Strepto- and staphylococci, which exist for a long time in foci of infection (tonsillitis, caries), often act as antigens. Antigens can also be yeast fungi for candidiasis, tuberculous mycobacteria and other microbes that exist in the body for a long time. A large number of antibodies are produced to them, which form immune complexes.
Predispose to the development of cutaneous vasculitis:
- alcoholism and smoking;
- industrial intoxication;
- diabetes;
- obesity;
- hypothermia;
- hypertension;
- thromboangiitis obliterans and other peripheral vascular diseases;
- rheumatological diseases, such as lupus, rheumatoid arthritis or scleroderma.
What is vasculitis?
Vasculitis is a group of diseases characterized by the development of inflammation of the walls of blood vessels. This inflammation begins due to an impaired immune response. The cause may be a past infection or allergy. Inflammation can affect small, medium, and large vessels. Because of it, blood circulation and blood supply to individual organs are disrupted, which can cause complications. Without treatment of vasculitis, necrosis of the vessel walls (death of their tissue), bleeding, and ischemia (impaired blood flow) begin. Both children and adults can get vasculitis. The disease can be primary (when inflammation of the walls of blood vessels is the only manifestation without an apparent cause) or secondary. With secondary vasculitis, the walls of blood vessels become inflamed due to other diseases (infectious, oncological, rheumatic).
Symptoms of cutaneous vasculitis
Manifestations of the disease depend on how large the skin vessels are affected. Therefore, there are three types of cutaneous angiitis:
- hypodermal - deep, affecting arteries and veins with rather thick muscle walls (this is periarteritis nodosa and angiitis nodosa);
- dermal - superficial, affecting the smallest arteries, veins and capillaries (this is polymorphic dermal angiitis, chronic pigmentary purpura and others).
Cutaneous form of periarteritis nodosa
Usually there are a few formations ranging in size from 1 to 3 cm, periodically appearing along the vessels on the legs. The skin above them acquires a bluish-pinkish tint. Such nodes are painful, can turn into ulcers, and last from several weeks to months.
Angiitis nodosum, or erythema nodosum
Characteristic features are reddish nodules, slightly raised above the surface of the skin and painful. Most often they are located on the front surface of the legs. Such nodes gradually develop and disappear.
The nodes are usually painful and inflamed for several weeks. Then they gradually decrease in size and merge with the skin, leaving bluish spots, which then also disappear without a trace. This condition recurs quite often, so the patient may simultaneously have newly formed nodes on the legs at different stages of development, as well as those that are already disappearing.
Polymorphic dermal angiitis (Gougerot-Ruiter disease)
One of the variants of polymorphic dermal angiitis is hemorrhagic.
This disease has several types:
- urticarial (resembles chronic urticaria);
- hemorrhagic (manifests as a hemorrhagic rash in the form of petechial skin hemorrhages, purpura, bruises - ecchymosis, blisters that open to form erosions and ulcerative defects);
- papulo-necrotic (inflamed nodes in the center undergo tissue disintegration - necrosis, so after their healing, retracted scars remain);
- pustular-ulcerative (reminiscent of gangrenous pyoderma - first, blisters appear on the skin, which then form a continuous inflamed surface, and eventually turn into an ulcer with a diameter of up to several centimeters; after healing, a deep scar remains);
- necrotic-ulcerative (foci of skin necrosis immediately form, turning into ulcers);
- polymorphic (purpura, nodules, blisters and other rashes are present at the same time).
Chronic pigmentary purpura
This disease has synonyms: progressive pigmentary purpura of Chambert or cutaneous hemosiderosis. It manifests itself as constantly recurrent multiple subcutaneous hemorrhages (petechiae), which then transform into brownish spots of iron deposits, that is, hemosiderosis.
Classification
Vasculitis is a large group of diseases, and two classifications are used for them. The first is by etiology - it takes into account the reasons for which the disease appears. The second is by localization, taking into account which vessels are affected.
By etiology
This classification takes into account the causes of vasculitis:
- primary. Inflammation of the walls of blood vessels is not associated with other diseases, is not their manifestation and develops as an independent disease. The exact causes of primary vasculitis have not been established, but it is known that hereditary predisposition plays an important role;
- secondary. The walls of blood vessels become inflamed due to other diseases, inflammation is one of their manifestations.
There are several types of secondary vasculitis based on the underlying disease or condition that caused inflammation of the vessel walls:
- hepatitis B and C viruses;
- syphilis;
- oncological diseases;
- reaction to taking medications.
By localization
Division by localization takes into account which vessels are affected by vasculitis and where they are located. This determines the clinical picture, treatment approaches, prognosis and possible complications. The walls of small, medium and large blood vessels can become inflamed; inflammation can affect blood vessels of different sizes or vessels of individual organs.
Vasculitis of large blood vessels
When the walls of large blood vessels become inflamed, there are several common symptoms. These are large deviations from the norm when blood pressure changes and anomalies in the propagation of pulse waves. With each such wave after the heart contracts, the pressure in the arteries increases. If the wave is asymmetrical or absent on the arms or legs, this may be a sign of vasculitis. The disease is also indicated by the development of ischemia (decreased blood flow in a particular area), intermittent claudication (pain that occurs when walking and goes away after rest). Each type of vasculitis of large blood vessels has its own additional symptoms.
Giant cell arteritis. Inflammation affects the thoracic aorta, as well as the large arteries running from it to the neck, and the extracranial section of the carotid artery. Polymyalgia rheumatica is often the cause of giant cell arteritis. Symptoms include: headaches, blurred vision, fever, weight loss, fatigue, and general malaise.
Takayasu arteritis. Inflammation of the walls of the aorta and its branches, the walls of the pulmonary arteries, most often develops in young women. The first signs of the disease are weakness, spastic pain in the limbs, periodic visual disturbances, hypertension, differences in pulse or blood pressure values on different legs or arms or on an arm and leg on the same side.
Vasculitis of medium-sized vessels
The general manifestation is symptoms of infarction of the tissues of the affected organs: their necrosis occurs due to insufficient blood supply. On the skin this is manifested by the formation of nodules, ulcers, and livedo reticularis (discoloration). With a muscle tissue infarction, severe pain appears. It is possible to develop multiple neuropathy (damage to several nerves), kidney damage (increased pressure in the renal arteries), and mesenteric ischemia, which disrupts blood flow in the intestinal vessels. The exact symptoms depend on where exactly the affected vessels are located.
Cutaneous vasculitis. It affects the vessels of the subcutaneous tissue, which is why ulcers, purpura (hemorrhages in or under the skin, look like scatterings of small red dots), petechiae (bright red rash) appear on the skin.
Polyarteritis nodosa. With this disease, the walls of the muscle arteries become inflamed, causing secondary tissue ischemia to develop. With nodular arteritis, damage to the skin, kidneys, peripheral nerves, gastrointestinal tract, and any other organs is possible. Lung damage is not typical. First, general symptoms appear: fatigue, fever. Other manifestations depend on which organ is affected.
Vasculitis of small vessels
When the walls of small vessels become inflamed, symptoms of tissue infarction develop in the affected area. Often these manifestations are similar to the symptoms of vasculitis of medium vessels.
Cryoglobulinemic vasculitis. It is systemic and affects mainly small vessels. Blood serum analysis reveals cryoglobulins. Symptoms are varied and are determined by the location of the inflammation. Damage to the kidneys and peripheral nervous system often develops, and vascular purpura appears. General manifestations are weakness, slight increase in temperature, fatigue. In 90% of cases, purpura appears, most often it forms on the skin of the legs. When the kidneys are damaged, peripheral edema and increased pressure in the renal artery develop. It is also possible to experience muscle and joint pain and enlarged lymph nodes.
Wegener's granulomatosis. The lesion can affect any organs, but most often it is the respiratory organs or kidneys. If the respiratory organs are affected, the first symptoms are cough and runny nose, after which swelling develops, increased pressure, and symptoms of damage to several organs at once appear.
Hemorrhagic vasculitis. More often children get it. There are four forms of the disease: cutaneous (cutaneous-articular), abdominal (with damage to the digestive organs), renal, mixed. Accordingly, characteristic symptoms are identified, including palpable purpura, abdominal or joint pain, renal syndrome, vomiting, and nausea.
Microscopic polyangiitis. A rare disease that most often affects the kidneys. In about a third of cases, additional purpura appears on the skin. Possible damage to the respiratory system with the rapid development of shortness of breath, hemoptysis, and anemia. If alveolar bleeding develops against this background, the patient needs emergency help. Abdominal pain, vomiting and nausea, and damage to the nervous system are also possible.
Vasculitides that can affect blood vessels of varying sizes
Behçet's disease. Inflammation develops on the walls of small or medium-sized vessels. Symptoms depend on location. The disease can affect the lungs, kidneys, stomach, and brain. A peculiarity is the frequent appearance of ulcers on the mucous membranes of the mouth, in the genital area, and other mucous membranes.
Cogan's syndrome. A rare disease in which blood vessels of different sizes become inflamed. The disease is often accompanied by fever, joint pain, neurological disorders, decreased vision, hearing loss (may be irreversible).
Systemic vasculitis
This group includes vasculitis associated with systemic diseases:
- systemic lupus erythematosus. The immune system begins to produce antibodies that damage healthy cells. Because of this, the walls of blood vessels become inflamed and lupus vasculitis develops;
- rheumatoid arthritis. This is a systemic inflammatory disease affecting small joints. May be accompanied by rheumatoid vasculitis;
- sarcoidosis The disease is accompanied by the formation of granulomas (nodules) in inflamed tissues. Foci of inflammation in sarcoidosis form in the lymph nodes, lungs, liver, spleen, skin, and bones. Sarcoidosis may be accompanied by sarcoid vasculitis.
Vasculitis of individual organs
Inflammation of blood vessels can affect only one, separate organ. Such diseases include:
- cutaneous vasculitis. Affects small and medium-sized vessels in the skin and subcutaneous tissue, manifested by the formation of ulcers, purpura, petechiae;
- cutaneous leukocytclastic angiitis. Inflammation of blood vessels in the skin is isolated and is not accompanied by systemic vasculitis or other associated conditions;
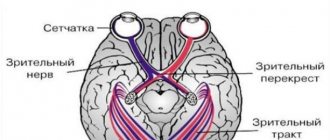
- primary angiitis of the central nervous system. It affects the vessels of the spinal cord, brain, and pia mater. There are no signs of systemic inflammation;
- isolated aortitis. A form of vasculitis with limited localization of inflammation of the vessel walls.
Diagnostics
Recognition of cutaneous vasculitis is based on the typical clinical picture. In some cases, a biopsy of the affected area of skin with its microscopic examination is prescribed. This confirms the damage to vessels of different diameters and surrounding tissues.
The main difficulty is the differential diagnosis of cutaneous vasculitis and manifestations of tuberculosis. Among them are indurative erythema and papulonecrotic tuberculosis. Evidence in favor of the cutaneous tuberculosis process is:
- young age of patients;
- exacerbation of skin tuberculosis in winter;
- positive tuberculin tests;
- tuberculosis damage to other organs.
Prevention
The causes of primary vasculitis are unknown, so special prevention is not carried out. Prevention of secondary vasculitis is carried out in several directions and involves restoration and maintenance of normal health:
- reducing the risk of contracting hepatitis B virus, hepatitis C virus, and other infections;
- timely and correct treatment of any diseases and especially infectious ones;
- taking medications only as prescribed by a doctor;
- maintaining a healthy lifestyle: maintaining a normal weight, giving up bad habits, proper nutrition and sufficient physical activity;
- allergy control. If they exist, it is important to exclude allergic reactions to food and medicines.
Treatment
In cutaneous vasculitis, the definitive cause of the disease is unknown. Therefore, complex therapeutic measures are used, aimed at different stages of the pathogenesis (development) of the disease. Required:
- rehabilitation of infectious foci - treatment of tonsillitis, caries, otitis media, cholecystitis and other inflammatory processes;
- correction of metabolic disorders, normalization of blood sugar levels, weight loss;
- antihistamines;
- preparations of vitamins C, PP, group B;
- calcium preparations;
- non-steroidal anti-inflammatory drugs;
- antibiotics (with a clear connection between the exacerbation of the process and an infectious disease).
In severe cases, methods of extracorporeal detoxification (“blood purification”) are prescribed - hemosorption or plasmapheresis, as well as glucocorticoid hormones with their gradual withdrawal.
In the chronic course of the disease, a rheumatologist may prescribe special medications, for example, delagil.
External treatment:
- for spots, papular rashes, nodules, dressings with hormonal ointments, for example, fluorocort, are indicated;
- for necrosis and ulcers, Vishnevsky ointments, solcoseryl, iruksol, and methyluracil are used.
During an exacerbation of the process, bed rest is necessary. In severe cases, especially those requiring the use of glucocorticosteroids, hospitalization in the rheumatology department is necessary.
Causes
Inflammation of the walls of blood vessels begins due to autoimmune disorders, in which antibodies are produced against the cells of one’s own body. The exact causes of primary vasculitis have not been established. Secondary vasculitis develops against the background of infectious or oncological diseases, as a rare complication of vaccination, after overheating or hypothermia, or sunburn.
Other possible causes include allergies to medications. More than 150 drugs have been identified that can provoke the disease. These include some antibiotics, analgesics, radiopaque agents, serums, vaccines, as well as iodine preparations, B vitamins and other drugs. Allergies, autoimmune failure and the development of vasculitis do not always occur after taking them. The risk of such complications is determined by the individual reaction to the components of the drug. Therefore, it is important that all medications are selected by a doctor. You do not need to choose your own antibiotics or antihistamines.
Prognosis and prevention
Despite complex treatment, complete and final elimination of skin lesions does not occur; the patient may develop a relapse at any time. Skin vasculitis is not dangerous for the patient’s life. They are also not dangerous to others, are not contagious, and are not directly inherited. A child can only inherit disturbances in the functioning of the immune system, which can manifest themselves in a variety of diseases in the future.
To prevent relapse of the disease it is necessary:
- elimination of foci of chronic infection;
- refusal of prolonged stress on the legs;
- avoiding bruises and hypothermia;
- rational employment with the exclusion of harmful factors.
Practicing dermatologist V.V. tells everything about skin vasculitis. Makarchuk:
Leukocytoclastic vasculitis
Vasculitis is an inflammatory disease of blood vessels. The article focuses on leukocytoclastic vasculitis, which is most often encountered in the practice of a dermatologist. In particular, the modern view of pathogenesis and etiology, possible clinical manifestations (hemorrhagic rash, ulcers, etc.) and approaches to treatment are considered. It is known that therapy for vasculitis depends on etiological factors, as well as the severity of skin manifestations.
Table 1. Classification of skin vasculitis
Rice. 1. Hemorrhagic rash due to vasculitis
Rice. 2. Ulcers due to vasculitis
Rice. 3. Livedo vasculitis
Table 2. Treatment methods for skin vasculitis
Rice. 4. General approach to the treatment of leukocytoclastic vasculitis
Recently, there has been an increase in the number of patients visiting doctors of various specialties (therapists, dermatologists, vascular surgeons, etc.) regarding hemorrhagic rashes in the lower and upper extremities. As a rule, such patients are diagnosed with skin vasculitis.
Vasculitis is an inflammatory disease of blood vessels. It may be primary, secondary, or a manifestation of a systemic disease.
The consequence of inflammation of the blood vessels of the dermis and subcutaneous fat is skin vasculitis. Currently, this pathology is not identified as an independent nosological unit. Isolated cutaneous vasculitis should be considered if systemic pathology is not established. However, signs of a systemic pathological process can be detected after the appearance of skin rashes.
The above makes it difficult to create a unified classification of skin vasculitis. One of the possible options for such a classification is presented in Table. 1.
To refer to the manifestations of vasculitis on the skin, the term “purpura” is often used (from the Latin purpura
). This is due to the characteristic coloring of skin rashes due to vascular inflammation. In medicine, purpura is understood as small-spotted capillary hemorrhages in and under the skin or mucous membranes of a reddish-violet color that do not fade when pressed. The release of red blood cells from the bloodstream occurs as a result of a violation of the integrity of the vascular wall. In dermatological practice, leukocytoclastic vasculitis is more often encountered.
Definition
Hypersensitivity angiitis (vasculitis) was first mentioned in the work of P. Zeek et al. in 1948 [1]. Skin rashes in the form of purpura and necrotizing vasculitis were noted during the use of the serum. Subsequently, along with the term “hypersensitive vasculitis”, the terms “drug vasculitis” or “allergic vasculitis” were used - in connection with the primary or secondary nature of the pathological process, the manifestations of which were limited primarily to the skin, as well as in connection with isolated skin vasculitis.
In modern literature, when discussing issues related to isolated skin vasculitis, leukocytoclastic vasculitis is mainly mentioned. This concept was introduced on the basis of a consensus adopted at a conference in Chapel Hill (USA) in 1994 - isolated leukocytoclastic angiitis of the skin, without manifestations of systemic vasculitis and glomerulonephritis - and is used in the context of allergic vasculitis [2].
Histologically, this type of vasculitis is characterized by inflammation of small vessels, in which the inflammatory infiltrate is represented by neutrophils. After degranulation, neutrophils die and, undergoing decay, form an infiltrate. This process is called “leukocytoclasia.” It should be noted that not all small vessel vasculitides are accompanied by the destruction of neutrophils. Lymphocytic and granulomatous vasculitic infiltrates have also been described.
Leukocytoclastic vasculitis can affect small vessels not only of the skin, but also of other organs. At the same time, leukocytoclasia can occur with vasculitis and other diseases in which neutrophils are the key cells of the inflammatory process.
Thus, the term “leukocytoclastic vasculitis” does not provide insight into the etiology and pathogenetic mechanisms of the disease.
Clinical manifestations
Leukocytoclastic vasculitis of the skin is characterized by the appearance of purpura, predominantly in the distal parts of the lower extremities (Fig. 1). The rashes are represented by petechiae with a diameter of about 3 mm. Petechial rash can also be localized on the forearms and hands, and less commonly on the upper torso. In bedridden patients, manifestations of leukocytoclastic vasculitis are localized, as a rule, on the back or side surface of the body.
In addition to petechiae, leukocytoclastic vasculitis may be accompanied by blisters, erythematous plaques, bullous hemorrhagic rashes and ulcerations (Fig. 2). Less common are livedo reticularis (Fig. 3), deep ulcers and nodules. Their appearance is regarded as involvement of the middle arteries in the pathological process.
The acute onset of the disease with the simultaneous appearance of petechial rashes on the skin is often associated with taking a number of medications or the development of infection. Recurrent petechial rashes on the skin can be observed with Henoch-Schönlein purpura and connective tissue diseases. The chronic course of leukocytoclastic vasculitis is often observed in patients with malignant neoplasms, cryoglobulinemia and systemic vasculitis of small vessels.
Pathogenesis
The occurrence of leukocytoclastic vasculitis is associated with a combination of factors: damaged skin (especially against the background of a secondary infection), drugs, immune complexes, inflammatory cells and vascular endothelium. It should be noted that the uniqueness of the skin's vascular system is due to its ability to respond to both exogenous and endogenous stimuli. In this case, migration of leukocytes, changes in permeability and signs of inflammation are observed mainly in post-capillary venules [3]. Endothelial cells at this level produce a specific set of procoagulants and anticoagulants, and also express HLA class II molecules. This may explain the ability of endothelial cells to act as antigen-presenting agents, to express Toll-like receptors responsible for recognizing pathogenic microorganisms, CD32 molecules involved in the type 3 hypersensitivity reaction, and histamine H1 receptors, the stimulation of which leads to vasodilation.
Thus, leukocytoclastic vasculitis is the result of a vascular reaction to various stimuli, from pathogenic microorganisms to circulating immune complexes, which develops with the participation of endothelial receptors at the level of postcapillary venules.
We have to admit that the pathogenesis of leukocytoclastic vasculitis remains not fully understood. Its development, as with many other autoimmune diseases, is the result of a complex interaction of genetic and environmental factors. However, most authors believe that this disease initiates the deposition of immune complexes in the walls of blood vessels. This assumption is confirmed by the results of experimental studies involving both animals and humans. It was found that the pathogenesis of leukocytoclastic vasculitis is similar to the mechanism of development of the Arthus reaction [4]. When there are a large number of antigens, circulating antigen-antibody immune complexes are deposited in the walls of blood vessels.
Complement components C3a and C5a are also involved in the development of inflammation in leukocytoclastic vasculitis. They promote the production and activation of chemotactic factors, which in turn stimulate the migration of neutrophils and basophils to the site of inflammation. Activated neutrophils release adhesion molecules, cytokines, collagenase and elastase, as well as free radicals, which leads to damage to the vascular wall. With small vessel vasculitis, other types of immune reactions are also observed - Gell and Coombs reactions.
Etiological factors
Identification of the root cause of the pathology is directly related to the choice of therapeutic tactics.
In particular, at the initial stage of diagnosing cutaneous vasculitis, it is necessary to determine whether the vascular damage is isolated, primary, idiopathic, or secondary, systemic, involving other organs and systems. Most often, leukocytoclastic vasculitis accompanies autoimmune and infectious diseases, as well as malignant neoplasms, and is a reaction to drugs.
It should be noted that the causes of the development of leukocytoclastic vasculitis in children and adults differ. Thus, in childhood, Henoch-Schönlein purpura (systemic hemorrhagic vasculitis) is more common. It develops predominantly against the background of bacterial and viral infections of the respiratory and gastrointestinal tract. The etiological factors of Henoch-Schönlein purpura are considered to be beta-hemolytic streptococcus group A, Haemophilus influenzae, chlamydia, mycoplasma, Legionella, Yersinia, Epstein-Barr, Coxsackie viruses, hepatitis B and C, adenovirus, cytomegalovirus, parvovirus B19, salmonella, Helicobacter
pylori
,
Clostridium difficile
.
Alcohol, certain medications, foods, hypothermia, and insect bites can be triggers [5].
Forecast
In most cases, when systemic disease is excluded, isolated leukocytoclastic vasculitis is characterized by a relatively favorable prognosis. In approximately 50% of cases, complete remission occurs within six months to one year. However, the disease can take on a chronic, relapsing course from several months to several years.
The prognostic criterion for chronicity is the presence of arthralgia, cryoglobulinemia and the absence of fever [6].
Therapy
The choice of therapy depends on the etiology of the disease and the severity of clinical manifestations (Fig. 4, Table 2) [7].
If leukocytoclastic vasculitis is secondary, for example developed due to infection or medication, the main and often sufficient component of the therapeutic strategy is considered to be elimination of the provoking factor.
If vasculitis is a manifestation of a systemic pathological process (for example, with granulomatosis accompanied by polyangiitis, Churg-Strauss syndrome), the treatment regimen is determined by the severity of damage to internal organs and, as a rule, includes the administration of systemic glucocorticosteroids and other drugs with an immunosuppressive effect. In recent years, biological therapy (rituximab) has been increasingly used for systemic vasculitis. In addition, the use of cytokine therapy (interleukins 5 and 6) is promising [8–10].
The chronic relapsing course of leukocytoclastic vasculitis requires the use of effective and safe drugs, with a relatively small number of unwanted side reactions. Bed rest is recommended for patients. In this case, the lower limbs should be raised.
Non-steroidal anti-inflammatory, analgesic and antihistamine drugs are prescribed as symptomatic therapy to eliminate burning and/or itching. However, these drugs do not affect the course of the disease and do not prevent the development of relapses.
If the rashes become rough, ulcerate, or nodular elements appear against their background, the disease recurs, and expansion of drug therapy is required. Thus, for leukocytoclastic vasculitis, Henoch-Schönlein purpura, and urticarial vasculitis, colchicine and dapsone are effective in some patients [11–13]. If they are ineffective, low doses of systemic glucocorticosteroids are prescribed, in particular 10–20 mg/day of prednisolone. Increasing the dose of glucocorticosteroids to 0.5–1.0 mg/kg/day is recommended in the presence of cystic elements, necrosis and a tendency to ulceration [14]. After achieving a positive clinical effect, drugs should be discontinued slowly, with a gradual reduction in the therapeutic dose.
In chronic leukocytoclastic vasculitis, the use of azathioprine is advisable [14].
Relatively recently, the effectiveness of the biological drug rituximab, which is a monoclonal antibody against CD20-positive cells, has been proven in patients with cutaneous vasculitis. This drug is especially effective for primary leukocytoclastic vasculitis, occurring in combination with cryoglobulinemia, as well as for secondary vasculitis that develops against the background of hepatitis C and Sjögren's syndrome [15].
Conclusion
Numerous attempts to define and create a classification of diseases characterized by isolated inflammation of the blood vessels of the skin are still being made.
Currently, leukocytoclastic vasculitis refers to a heterogeneous group of inflammatory lesions of the walls of small vessels of the skin, which develop under the influence of etiopathogenetic and trigger factors. In most cases, they are a consequence of pathology of other organs and systems.
In order to determine the nomenclature of these diseases and develop new pathogenetically based treatment methods, it is necessary to continue studying the mechanisms of their development.
Diet for vasculitis
The diet for vasculitis is designed to eliminate food allergies, normalize weight, and provide the daily requirement for calories, vitamins, minerals, etc. When forming a diet, they take into account the causes that provoked vasculitis and which organs were affected due to inflammation of the walls of blood vessels and poor circulation. For example, if the stomach or intestines are damaged, a special nutrition plan is needed.
General recommendations involve organizing a healthy diet: excluding foods that cause an allergic reaction, eating enough fresh vegetables and fruits, dairy products, cereals, excluding fatty, spicy, fried foods. In each individual case, you can contact a nutritionist for help in creating a diet.
Forecast
Depends on the form, localization of vasculitis, severity of the disease. In some cases, primary vasculitis goes away without treatment and leaves no consequences at all. In others, the disease develops rapidly and is life-threatening. It is important to consult a general practitioner or rheumatologist in time, immediately after the first symptoms appear. The main danger with most forms of vasculitis is possible complications:
- severe cardiovascular diseases, heart attacks with polyarteritis nodosa;
- development of infections and pulmonary hemorrhages with microscopic polyarteritis;
- infections, renal, respiratory failure, cardiovascular accidents with Wegener's granulomatosis;
- partial or complete loss of vision with giant cell arteritis (but overall the prognosis is favorable);
- strokes, heart attacks with Takayasu arteritis.
To improve the prognosis, it is important to strictly follow the recommendations of the attending physician, try to prolong the remission of the disease, and eliminate factors that provoke relapses.
Valeria Korol – general practitioner, rheumatologist, Member of the expert council of MedPortal “How to avoid recurrent vasculitis?
— Avoid factors that can provoke an exacerbation of the disease:
- Infections
- Stress
- Exposure to direct sunlight
- Unmotivated medication use
- To give up smoking
- Normalization of body weight
- Valeria Korol
- general practitioner, rheumatologist"