Melanoma statistics
Melanoma is the leading type of cancer, ranking third in prevalence in men and second in women. At the same time, the number of victims increases every year, and the disease becomes “younger.”
In most cases, tumors occur on exposed skin, with about 70% of cases on the face.
Modern medicine has a wide range of cancer treatment options. Oncologists have chemotherapy, hormonal treatment, immunotherapy, which allows them to block specific immune checkpoints, and targeted drugs, which specifically affect cancer target cells. Recovery is possible, the main thing is timely diagnosis!
MelanomaUnit oncologists recommend regular preventive examinations and medical examinations for early diagnosis of melanoma and other skin cancers.
Prognosis and prevention
The prognosis directly depends on the stage at which the tumor was detected. When skin melanoma less than 1 mm thick is removed, the survival rate is more than 90%, and only a small number of patients subsequently experience relapses [2]. At the same time, with large cancer tumors and metastases in internal organs, more than half of the patients die within a few years.
To prevent melanoma, it is recommended to follow the following recommendations:
- Avoid sunlight during the middle of the day. This is a risk of burns and sunburn, which causes skin damage and increases the risk of developing melanoma. Ultraviolet radiation is most intense from 10 a.m. to 4 p.m.
- Use sunscreen. Choose a product with SPF of at least 30 even on cloudy days, and in summer in the sun - SPF 40-50. Apply the cream generously to your body and repeat every two hours, or more often if you swim or sweat heavily.
- Don't forget about clothes. Cover your skin with dark, thick fabric that covers your arms and legs, and wear wide-brimmed hats. Wear sunglasses.
- Avoid tanning lamps and tanning beds, they emit ultraviolet rays and may increase the risk of skin cancer.
- Examine your body. Check your skin regularly to see if new formations have appeared, moles, freckles, or birthmarks have changed.
- Remove moles that are often injured. At the site of the removed mole, only a barely noticeable scar remains. The greatest risk of developing melanoma is in nevi that are regularly touched by underwear, backpack harnesses or a blade during shaving or haircuts.
Sunscreen as a means of preventing melanoma
Sunscreens help prevent skin cancer.
Photo: zefart / Depositphotos Before going outside on a hot sunny day, it is recommended to apply sunscreen to exposed areas of the body to block ultraviolet rays. However, not all products are suitable for children aged 6 months and younger. Sunscreen has varying degrees of sun protection. Sun protection factor, SPF, shows how well UV rays are blocked. To prevent melanoma, it is recommended to use products with SPF 30 or higher.
It is important to remember that sunscreen wears off or loses its protective properties over time. It should be reapplied if the skin remains exposed to the sun for more than 2 hours, after swimming, when sweating heavily, or after drying with a towel [4].
Conclusion
Melanoma is one of the most dangerous types of cancer. At the same time, due to the fact that it is usually located on the surface of the skin, it is easy to identify and remove in time. This will prevent the tumor from spreading to the internal organs.
How does melanoma manifest?
Melanoma is one of the fastest growing types of cancer, which quickly “gives” metastases to the lymph nodes and internal organs.
At the initial stage of skin cancer, attention is drawn to the appearance of a new growth on the skin or a change in the color, size and shape of an existing mole.
The patient may also complain of itching, pain and burning sensation in the area of formation.
Targeted therapy
In approximately half of cases of melanoma with metastases, a mutation is detected in the BRAF gene. In this case, the drugs vemurafenib, dabrafenib and trametinib are effective. They belong to the group of protein kinase inhibitors. Thanks to them, the tumor may shrink, but, unfortunately, it will continue to grow in the future. Dabrafenib is most often prescribed together with trametinib. Side effects of this combination include fever, rash, fatigue, and abnormal liver tests. Other skin cancers may develop while taking vemurafenib (it can be treated by simply removing the melanoma), and in some cases, skin sensitivity to light, joint pain, fatigue, itching, and hair loss may occur.
ABCDE method in diagnosing melanoma
There are criteria (ABCDE), thanks to which patients can independently suspect a problem and consult a doctor:
- A (asymmetry) – asymmetry . The mole grows unevenly to the side. Normally, if you draw an imaginary line through the middle of the mole, the halves will be symmetrical.
- B (border irregularity) – uneven, jagged, fuzzy edge.
- C (color) – color. Suspicion of melanoma is caused by changes or heterogeneity in color, the appearance of inclusions.
- D (diameter) – diameter. Increase in size of a common mole.
- E (evolving) – variability of any characteristic: color, shape, size is a reason for immediate consultation with an experienced dermato-oncologist.
IMPORTANT : there is a type of melanoma that contains virtually no pigment and in the initial stages resembles more of a pimple or an ingrown hair, this disease is called non-pigmented melanoma .
There are several successive stages in the development of melanoma:
- Stage O - characterized by damage to the upper layers of the epithelium, which responds well to treatment.
- Stage 1 - the pathological process penetrates into the deeper layers of the epithelium, but the size of the tumor does not exceed 2 cm.
- Stage 2 - the size of the tumor can increase up to 5 cm.
- Stage 3 - characterized by the appearance of the first metastases in sentinel and regional lymph nodes.
- Stage 4 is the terminal stage of the disease, which is characterized by multiple metastases to distant organs and tissues.
Symptoms
In most cases, melanoma develops from a mole (nevus). Early signs of a tumor include:
- horizontal increase in size of moles - growth in width over the surface of the skin;
- changes in the boundaries of the nevus - they become uneven, blurred, asymmetrical;
- change in the color of the mole, the appearance of heterogeneity (black, brown and other areas on one nevus), light spots in and around it.
These signs do not always indicate the development of skin melanoma. On the other hand, at a very early stage, the symptoms of the disease are easy to miss with the naked eye. Therefore, it is important to consult a doctor when the first signs or even suspicions appear. Timely treatment can save the patient's life.
Late symptoms:
- vertical growth - the formation rises above the surface of the skin;
- peeling, itching, pain, bleeding of the surface of the nevus;
- enlargement of regional and distant lymph nodes.
Sometimes people, especially those who are characterized by increased anxiety, begin to suspect melanoma, mistaking it for ordinary moles. There is another extreme - patients ignore the initial signs of melanoma, considering them a newly appeared or injured nevus, age-related pigmentation. It is important to distinguish a mole from a malignant formation.
Moles usually have a smooth surface and even, symmetrical edges. Their color varies from light brown to dark brown, it is uniform, without light or dark inclusions. The normal size of a mole is considered to be up to 6 mm in diameter (you can use a pencil eraser as a guide). Moles extremely rarely change their size, and they are not characterized by unpleasant or painful sensations.
What types of melanoma are there?
There are several classifications of melanoma, the most common of which is the TNM system:
- Tumor
- LymphNode – lymph node
- Metastasis – metastases
T-category
This is the volume or thickness of the tumor, which is measured using the Breslow system. Also in this category the rate of development of metastases is taken into account.
N-category
Determines the presence of a tumor in the lymph nodes that are susceptible to metastasis in the first place.
M-category
This category determines the spread of the pathological process to internal organs.
Complications and consequences of the disease
Pigmentless melanoma can be complicated by screenings of daughter tumors, metastases, and internal organs. This leads to a deterioration in their performance:
- metastases in the lungs impair blood oxygen saturation;
- brain metastases cause seizures, personality changes, and impaired movement and/or sensation in the limbs. Daughter tumors in the brain stem lead to disturbances in breathing, heartbeat, and maintaining normal blood pressure levels;
- metastases in the bones cause severe pain, bone destruction, difficulty in movements - up to their complete impossibility;
- metastases to the liver lead to indigestion, yellowing and itching of the skin, and deterioration of brain function;
- metastases to the skin cause pain.
When neoplasia is detected by the body's immune system, intoxication develops. It manifests itself as weakness, loss of appetite, drowsiness, and nausea. A person stops eating normally, and the body does not receive the nutrients it needs for life and to fight the tumor.
Over time, cancer cachexia develops - exhaustion. It is manifested by weight loss, constant weakness, and lack of appetite. Cachexia further worsens a person’s condition, disrupting metabolism and the functioning of all his internal organs.
Stages of melanoma
| Stages of melanoma | Characteristics of the stage |
| Melanoma 0 | Present only in the upper layer of the skin - the epidermis (in situ). This melanoma is non-invasive; it does not penetrate into the deeper layers of the skin and does not spread to other parts of the body. |
| Melanoma I | There are two subcategories here - A and B. The thickness of the tumor at an early stage does not exceed 1 mm. The neoplasm has no peeling or ulcers and does not bleed. The rate of cell division is quite low. Melanoma does not affect organs or lymph nodes. At this stage, surgery is recommended, i.e., surgical removal of the malignant neoplasm. |
| Melanoma II | There are three subcategories here - A, B and C. At this stage, the tumor penetrates deeper. The thickness of melanoma can reach 2.00 mm and sometimes 4.00 mm. The surface of the melanoma itself takes on a hypertrophied appearance. There is peeling, the presence of ulcers, and sometimes bleeding. Lymph nodes and other organs are not affected. |
| Melanoma III | There are also three subcategories here - A, B and C. At this stage, the tumor affects the lymph nodes. They can be increased, but not always. The malignant neoplasm thickens and penetrates even deeper into the tissue. Expressions can also either appear or not. At this stage, radiation and operable (surgical) methods are accepted as treatment. |
| Melanoma IV | This stage is the last stage of skin cancer. The malignant neoplasm is already metastasizing, affecting internal organs such as the liver, lungs, and brain. Penetrates to distant lymph nodes and affects individual areas of the skin. At this stage, long-term and complex treatment is necessary. It is also possible to resort to surgical methods, removing individual skin lesions affected by the tumor or cutting out metastases from internal organs. |
Diagnosis of melanoma
The prognosis for recovery largely depends on the timeliness of diagnosis and the prescription of adequate treatment.
Early accurate diagnosis of melanoma is carried out using an accurate modern examination - dermatoscopy .
The tumor can be diagnosed with high accuracy using special studies: dermatoscopy, drawing up a “mole map” using the Fotofinder system.
At the moment, no single cause of melanoma has been established, but doctors identify a number of predisposing factors :
- excessive inhalation or active exposure of the skin to the sun's rays
- heredity
- a certain phototype - freckles, light skin and eye color
- a large number of moles (nevi) on the body.
If you are at risk, it is recommended not to overuse ultraviolet rays (tanning, solarium). In people with dark hair and dark skin tone, melanomas may form on the surfaces of the palms and soles. Many clinical studies have proven that 50-75% of melanomas are formed from moles already on the body. Accidental damage can cause it to transform into a malignant tumor. Therefore, it is recommended to take special care to protect nevi from external trauma, rubbing, and to visit an oncologist at the first warning signs, which include:
- horizontal or vertical unnatural growth;
- identified asymmetry of the edges;
- growths on a mole;
- mole falling off;
- color changes;
- discomfort in the area of the nevus;
- the appearance of foreign formations on the mole, bleeding.
- sunburn, intense tanning both naturally and in a solarium
- congenital nevi
- genetic predisposition , that is, cases of cancer, especially skin cancer, in close relatives
- diseases of the endocrine system, especially damage to the thyroid gland
- trauma to the skin , birthmarks and moles
- increased sensitivity to ultraviolet radiation
- age factor – with age increases the risk of skin cancer
- Skin phenotypes 1 and 2 are people with fair skin, blond or red hair, blue or gray eyes and freckles.
Melanoma cancer cells spread throughout the body through the lymphatic system, and one of the earliest sites of spread for metastasis is nearby lymph nodes. Examination of the lymph nodes helps answer the question of whether melanoma has metastasized to other parts of the body.
Professor Chaim Gutman, doctor of the highest category
For more information about the causes and risk factors for melanoma, see the article “Risk Factors for Melanoma”
Melanoma most often affects young people, especially those with fair skin and hair.
The content of the article
To recognize melanoma, it is worth looking at skin changes based on the ABCDE principle. Testing is best done in the fall to check for current and new changes. Melanoma is a malignant tumor that metastasizes, so its early detection is very important.
Melanoma consists of melanocytes - pigment cells of the skin that produce the pigment - melanin. The dye causes the skin to darken when exposed to ultraviolet rays, such as the sun or lamps used in tanning beds.
Melanoma on the skin
Melanomas most often appear on the skin, but they can also occur around the mouth, nose, nails, or eyeball.
Melanoma, which initially appears on the surface of the skin, eventually penetrates deeper than 1 mm into the skin and spreads beyond the dermis into the blood vessels. Then through them it reaches other organs in a very short time. Cancer develops in up to three months, so postponing a visit to a dermatologist even for a day can cost you your life.
Melanoma is characterized by aggressive growth and the ability to form early and numerous metastases, which are very difficult to treat pharmacologically. Metastatic melanoma is the deadliest form of the disease, which occurs when cancer spreads beyond the surface of the skin to other organs such as the lymph nodes, lungs, brain and other areas of the body.
Meanwhile, removal of local melanoma, when the disease is not yet widespread in the body, can cure up to 97% of patients. That is why it is extremely important to quickly and correctly recognize this type of oncology.
Melanoma staging
Staging of melanoma or, in other words, determining the stage of tumor development is based on its thickness, size, rate of spread of metastases, presentation of the tumor (how often and severely symptoms manifest itself), damage to the lymph nodes, as well as other organs.
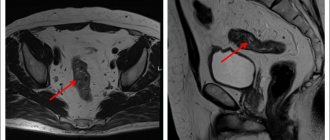
To determine the stage, it is necessary to conduct a comprehensive examination. It is carried out as follows:
- Examination by a dermato-oncologist
- Dermatoscopy
- Biopsy of the pathological formation followed by histology
- If necessary, computed tomography (CT), radiography, ultrasound and magnetic resonance imaging (MRI) may be prescribed.
Determining the stage of melanoma development is extremely important, as this helps to prescribe the most effective treatment and apply the right method in the fight against malignancy.
Clinical classification. Types of melanoma
Melanoma manifests itself in various forms, there are 3 main types:
- Superficially widespread.
Tumor of melanocytic origin. The most common disease (70 to 75% of cases) among middle-aged Caucasians. Relatively small, complex in shape with uneven edges. The color is uneven, reddish-brown or brown, with small patches of bluish tint. The neoplasm tends to become a tissue defect, accompanied by discharge (usually bloody). Growth is possible both on the surface and in depth. The transition to the vertical growth phase can take months or even years.
How to determine the stage of melanoma
In general, there are two main methods for determining the stages of melanoma.
Clinical – based on an examination of the patient by a specialist and the results of a biopsy (morphological examination of a cell sample).
Histological – based on a microscopic method for studying tissues, organs and body systems, using biopsy and surgical methods. Histological analysis, as a rule, shows a higher stage of development of the malignant neoplasm. So, if a biopsy showed, for example, the 3rd stage of melanoma, then histological analysis may already show the 4th stage of skin cancer.
| Melanoma stage | Characteristics of the spread of melanoma |
| Stage 0 | Tis, N0, M0 – the earliest stage. This stage means that the tumor has not spread to the lower layer (dermis). Melanoma is found in the epidermis. |
| IA stage | T1a, N0, M0 – stage 1A melanoma, malignant neoplasm thinner than 1 mm. This stage means that melanoma has not been diagnosed. The rate of spread of metastases is less than 1/mm2. Melanoma has not yet invaded the lymph nodes or distal organs. |
| IB stage | T1b or T2a, N0, M0 – stage 1B melanoma, a malignant neoplasm thinner than 1 mm. Melanoma has been identified, the rate of spread of metastases is less than 1/mm2. Also at this stage, melanoma may not be detected, and its thickness can reach from 1.01 to 2.00 mm. At this stage, melanoma has not yet affected the lymph nodes or distal organs. |
| Stage IIA | T2b or T3a, N0, M0 – stage 2A melanoma. At this stage, the thickness of the melanoma can vary from 1.01 to 2.0 mm, and the neoplasm is identified. Also, the thickness of melanoma can be from 2.01 to 4.00 mm, but the neoplasm is not detected. Melanoma has not yet invaded the lymph nodes or distal organs. |
| IIB stage | T3b or T4a, N0, M0 – stage 2B melanoma. At this stage, the thickness of melanoma can be from 2.01 to 4.00, and the neoplasm is detected. Also, the thickness of the neoplasm may be more than 4.00 mm, but it is not pronounced. There is no melanoma in distal organs and lymph nodes. |
| IIC stage | T4b, N0, M0 - stage 2C melanoma. At this stage, the thickness of the melanoma is 4 mm, it is revealed. Melanoma has not yet invaded the lymph nodes or distal organs. |
| IIIA stage | T1a to T4a, N1a or N2a, M0 . At this stage, the thickness of the melanoma is any, it is not expressed. Melanoma has already spread to 1-3 lymph nodes located next to the area of skin that is affected. However, the nodes have not yet been enlarged. Melanoma is only visible when viewed carefully under a microscope. It has not yet spread to remote areas. |
| IIIB stage | T1a to T4a, N1b or N2b, M0. The thickness of melanoma is any, it is not expressed. Melanoma has already spread to 1-3 lymph nodes located next to the affected area of the skin. Lymph nodes are enlarged. The melanoma has not yet spread to distant areas. T1a to T4a, N2c, M0. The thickness of melanoma is any, it is not expressed. The melanoma has already spread to nearby small areas of skin or, possibly, to the lymphatic channels located next to the tumor. The nodes themselves, however, do not contain melanoma. The melanoma has not yet spread to distant areas. |
| IIIC stage | T1b to T4b, N1b or N2b, M0 . Melanoma is diagnosed at this stage; its thickness can be of any size. The zone of spread of melanoma in this case is 1-3 lymph nodes located next to the neoplasm that has affected the skin. There is an increase in lymph nodes. The melanoma has not spread to distant areas. T1b to T4b, N2c, M0. Melanoma was also detected, the thickness was any. In this case, it spreads to the lymphatic channels located next to the tumor and nearby areas of the skin. Lymph nodes are not affected by melanoma. The melanoma also did not spread to distant areas. Any T, N3, M0. In this case, melanoma may or may not be detected; its thickness can also be any. It has already spread to 4, and maybe more, clustered lymph nodes located near the site of the lesion. It can also spread to the lymphatic channels passing next to the tumor and nearby areas of the skin. Lymph nodes are enlarged. There is no spread to more distant areas. |
| IV stage | Any T, any N, M1(a, b, or c) . At this stage, melanoma has already spread far beyond the area on the skin where it appeared. It also spreads to other organs through nearby lymph nodes. Melanoma can spread to the brain, affecting the liver and lungs. It can affect distant lymph nodes, distant areas of the skin, and subcutaneous tissues. In this case, there is no need to consider the spread of melanoma to nearby lymph nodes, as well as its thickness. But, usually, it is very voluminous and affects the lymph nodes. |
Etiology
The main causes of melanoma are based on two factors: uncontrolled exposure to solar radiation or artificial ultraviolet radiation through the use of tanning beds. Excessive passion for beach tanning or exposure to lamps with UV radiation entails a violation of the DNA structure of skin cells and increases the likelihood of cancer formation.
In addition, there are additional risk factors for skin cancer. Among them:
- Phenotype. People with light skin tones, blondes, and those with blue eyes are more likely to suffer from this disease.
- Weakened immunity increases the chances of developing skin cancer
- Having a large number of moles
- History of sunburn
- Xeroderma pigmentosum
- Age group over 50 years
- Heredity. If there were more than two relatives in the family suffering from a similar disease, this is a reason to turn to professionals for help.
- Presence of nevi (melanoform nevus is especially dangerous)
- Previously diagnosed melanoma
Pathogenesis
Medicine divides the development of melanoma into stages (according to Breslow):
- I – formation occurs only in the outer layers of the skin (in the epidermis, up to the basement membrane; thickness less than 2 mm).
- II – the tumor is found in the outer layers of the skin (thicker than 2 mm; may be characterized by the presence of an ulcer).
- III – the cancer process spreads to the lymph nodes near the affected area and/or extends beyond the primary tumor site (the border between the papillary and reticular layers of the dermis).
- IV, V – tumor cells are found in the reticular layer of the dermis, grow into fatty tissue, metastases spread throughout the body, with selective damage to organs.
Clark's microstage division includes thin, intermediate and thick (deep) forms of invasion.
Prognosis varies based on existing stages of melanoma.
If diagnosis and treatment occurred in the initial stages of the disease (I, II), then the prognosis is excellent and is 98.2% survival. Stage III leaves the chances of life within 61.7%. Stages IV, V (especially with metastasis) are characterized by a rapidly progressive and fatal course. As a result, less than 10% survive 5 years, and most patients die within a year of diagnosis.
Metastasis of melanoma occurs lymphogenously to the skin, lymph nodes and hematogenously to the liver, lungs, brain, bones, kidneys, adrenal glands. Trends in melanoma metastasis depend on the biological characteristics of the tumor. There are forms that metastasize for a long time only lymphogenously to regional lymph nodes. There are melanomas with a high malignant potential with a tendency to early hematogenous metastasis. Particular attention should be paid to such forms of skin metastases as satellite, nodular, erysipelas-like, and thrombophlebitis-like. Satellites are small multiple rashes near the primary lesion or at some distance from it in the form of spots that have retained the color of the primary tumor. The nodular form of skin metastases is manifested by multiple subcutaneous nodes of various sizes. The erysipelas-like form of cutaneous metastases appears as an area of swollen, bluish-red skin surrounding the tumor. The thrombophlebitis-like form of skin metastases is manifested by radially spreading painful compactions, dilated superficial veins and hyperemia of the skin around the melanoma.
Heredity of the disease
An independent study was conducted in Sweden, which involved 79,060 people with melanoma. Of these, only 9% turned out to be hereditary. Despite this low rate, the tumor is considered hereditary. It is assumed that a person inherits a violation of suppressors, which are responsible for suppressing oncological processes. Of the subjects with hereditary cancer, 92% were from families where there were already 2 cases of melanoma. Another 8% were among those with 3 or more cases in their family history. Scientists have also found that families with a history of melanoma have a significantly higher risk of other types of cancer.
Psychosomatics
Psychosomatics is a science that classifies all diseases as psychological. Conventionally, we can identify several mechanisms that influence the launch of the “self-destruction” mechanism - depression (primary and secondary), neurosis and trauma, situational psychosomatics (acute conflict, stress) and true (associated with our psychotype).
Stressful events
Why do we associate stress with cancer? Information about the “self-destruction” of the body is genetically embedded in us. When a person’s life begins to be dominated by various kinds of stress, conflicts, problems and seemingly minor troubles that do not find relief, quick resolution and compensation, sooner or later the person begins to be burdened by this situation psychologically, and physically his body constantly produces a stress hormone that significantly affects for immunity.
We live in a real physical body, in which real, sometimes independent of us, physical laws operate. Therefore, it is important to understand that in order for the disease to develop as it does, several factors must be combined. When we take a medical history and see in it a genetic predisposition to cancer, we additionally note the consumption of large quantities of food containing so-called carcinogens, the person lives in a certain environmentally unfavorable or radiation zone, when we observe other elements of self-destructive behavior: alcohol, smoking , self-medication with medications, a regime of stress (violence) on one’s body, and when we note problems of a psychological nature, only then can we say that the risk is really high. In this case, we consider the psychological factor as permissive. Indeed, in fact, in the body of each of us there are constantly those same immature, continuously dividing cells. But the principle of homeostasis is designed to prevent an increase in their number; every second our body works to maintain a healthy state.
Depression. Previously, depression was associated only with a reaction to the disease itself and treatment. However, patient stories have shown that often the disease can occur against the background of depression itself, or secondary, when a psychological disorder appears against the background of some disease.
So it is against the background of primary depression, when in the anamnesis of patients with oncology we see that they had previously been treated for depression. Moreover, experimental studies have shown that people suffering from depression have increased levels of a protein in their blood that is involved in the formation of cancer cells and the spread of metastases in the body. Moreover, one of the versions according to which oncology is classified as a so-called psychosomatosis is based precisely on the fact that often psychosomatic diseases are nothing more than a manifestation of somatized (hidden, masked) depression.
Neurosis and psychological trauma. Another option that we see in practice, although not in all patients, is also important and correlates with psychological trauma. More often, trauma that we remember but block on an emotional level manifests itself in organ neuroses, and here we would rather work not with oncology, but with cancerophobia.
Since we correlate true psychosomatics with constitutional characteristics (what is inherent in us by nature and does not change), more often this leads to the idea that oncology has a connection with some feelings, character traits, organs, etc. Indeed, we note that, for example, people with asthenic physique often have skin and lung cancer, but this is connected not so much with the person’s problems as with his personality. By the way, speaking about what decoding or significance this or that organ has in psychosomatics, we can immediately answer that most often there is none. In a hospital, people with the same diagnosis have completely different characters and psychological problems, any oncologist will confirm this to you. “The choice of tumor location” is more connected: with a constitutionally weak organ (where it’s thin, it tears – sometimes we talk about the risk of “breast cancer” for a woman whose mother had a tumor, but a woman can inherit her father’s constitution and our prognosis will not come true, and vice versa ); with the carcinogenic factors listed above (if a person smokes, then there is a higher probability of damage to the throat and lungs; if a person abuses medications and unhealthy food - to the stomach; sun/solarium - to the skin, but this is not the law and is considered with other components); with hormonal imbalance, in particular with the peculiarities of the production of neurotransmitters in a particular person at a particular point in time (each person needs a different amount of hormone to show a particular emotion and, by and large, although this depends on the constitution, it is also due to what happens in a person’s life) and even with age (each organ has its own history of development - renewal and destruction, so in different periods different cells can divide more intensively) or direct injury to the organ (often patients indicate that before the development of a tumor this area was injured (got a cold, hit, broke, broke), but we are talking about injury not as a cause of oncology, but as a localization, no need to be confused).
Is the disease contagious?
No type of cancer, including melanoma, can pass from a sick person to a healthy person. Only genetic predisposition is passed on in the family.
Treatment of melanoma at different stages
The choice of treatment tactics depends on the stage of the disease and the patient’s health status.
It is important to know! Depending on the size of the tumor and clinical signs, the surgeon chooses the optimal treatment tactics. The given example of manipulations can be adjusted based on the individual characteristics of the tumor.
Stage 0 - immunomodulators are prescribed in combination with surgical removal of the tumor.
Stage I - surgery is prescribed in combination with a biopsy of sentinel lymph nodes. Most often, such treatment is supplemented with chemotherapy to consolidate the results.
Stage II - treatment is the same as for the first stage - removal of the tumor and consolidation of the result with chemotherapy and other treatment methods. If metastases are detected in the sentinel lymph nodes, the surgeon excises them.
Stage III - drawing up an individual comprehensive treatment plan, combining surgery, chemotherapy, immunotherapy or targeted therapy.
Stage IV - complex therapy depending on the condition and well-being of the patient, in severe cases - palliative treatment.
After completion of treatment, the patient is recommended to undergo regular examinations to monitor his health and not miss a recurrence of skin cancer.
You can find out the exact cost of melanoma removal and prices for histological examination of the tumor by phone and at the initial appointment at the clinic.
Read more about why laser is unacceptable and the advantages of surgical excision in the article “Scalpel versus laser”
Causes and risk factors
Melanoma develops due to malignancy (malignant degeneration) of melanocytes. No reliable causes of cell degeneration have been identified; every person is at risk of the disease. Factors that increase the risk of tumor development:
- hereditary predisposition;
- Phototypes I and II – fair skin, hair and eyes, pink freckles;
- multiple moles, age spots;
- excessive ultraviolet radiation - both natural and in a solarium;
- age over 50 years;
- endocrine diseases;
- previous melanoma.
The combination of any three of these factors is a reason for regular preventive visits to a dermatologist.
Statistics and forecasts for melanoma
Every year, about 140 thousand new cases of melanoma are diagnosed worldwide. According to statistics, this type of skin cancer affects women more often, and in every tenth patient a genetic predisposition is “to blame.
In recent years, modern medicine has made a big step forward, giving hope to patients diagnosed with melanoma - when diagnosed at the earliest stage of development and prescribed adequate treatment, recovery occurs in more than 90% of cases.
The age of the patient plays an important role in predicting the outcome of the disease. As a rule, the younger the person, the higher the chances of recovery.
Another interesting factor is that people with fair skin are more likely to suffer from skin cancer. But if a dark-skinned person gets sick, it is believed that his disease will be more severe. Predisposing factors for severe melanoma are chronic diseases and health problems.
Survival Projections
According to WHO, more than 132 thousand cases of melanoma are diagnosed every year worldwide. Women get sick more often than men. Melanoma can be inherited - about 10% of cases. However, thanks to early diagnosis and new developments in the field of medicine, the overall survival rate (up to 5 years) of patients has increased in the last 10 years. Melanoma at an early stage is characterized by a positive prognosis in treatment and stable remission in more than 90% of patients. Statistical data on five-year survival rate: I degree (up to 92%), II degree (53–81%), III degree (40–78%), IV degree (15–20%).
Sometimes the prognosis for grade IV melanoma is even better than, for example, grade II or III, since cancer cells metastasize to distant areas of the skin and lymph nodes, “bypassing” important organs and systems. In addition, the prognosis must take into account the level of LDH - if it is normal, then the chances that the disease will recede increase even more.
The survival prognosis is influenced by the age of the patients. Thus, older people have slightly less chances than young people, regardless of the stage of melanoma. White-skinned people are more likely to suffer from skin cancer, but if the disease is diagnosed in a dark-skinned person, their chances of survival are lower. Those who have undergone organ transplants, have HIV, or have serious chronic diseases also have worse prognoses for recovery.
Benefits of skin cancer treatment at MelanomaUnit
MelanomaUnit is a branch of an Israeli medical center, the basic principles of which are the highest quality of services, experienced specialists and maximum comfort for patients.
We use equipment from the best manufacturers of medical equipment, certified time-tested drugs and innovative technologies aimed at maintaining health.
Our specialists constantly improve their skills by undergoing training in Russia and abroad. MelanomaUnit doctor is to achieve the best result for the patient.
Make an appointment