Finger examination
This method allows you to assess the condition of the rectal mucosa:
- the presence of enlarged hemorrhoids,
- their size and location,
- assume the development of complications (anal fissure, paraproctitis, thrombosis of hemorrhoids, etc.)
In typical situations, the doctor may limit himself to these methods. They allow you to verify the presence of nodes, as well as determine the stage and determine treatment methods for hemorrhoids.
In unclear cases, when it is necessary to exclude cancer of the lower intestine or some of the complications of hemorrhoids, additional diagnostic methods are used:
Anoscopy. This method of visualizing the rectal mucosa makes it possible to assess its condition over a length of 12 cm. Using the anoscopy method, an anal fissure, polyps and other neoplasms are determined.
Sigmoidoscopy. Diagnostics using a sigmoidoscope allows you to see the rectum and part of the overlying large intestine at a distance of up to 35 cm from the anus.
Colonoscopy. This imaging method allows you to evaluate the condition of the colon mucosa from the rectal region to the lower sigmoid colon.
If there are complications of hemorrhoids or an unclear clinical picture, laboratory research methods can be used:
General blood analysis. This study makes it possible to diagnose iron deficiency anemia, which is a common complication in stages III and IV of hemorrhoids and is associated with chronic blood loss from the rectum.
Fecal occult blood test. This analysis is carried out if there is a need for differential diagnosis between hemorrhoids and pathology of the overlying parts (for example, duodenal ulcer).
Coprogram. This method of examining stool allows you to evaluate the presence of mucus or undigested inclusions. The coprogram is relevant for constipation of unknown etiology or for suspected diseases associated with hemorrhoids.
Clinical picture
Clinical manifestations of hemorrhoids are different in acute and chronic course of the disease.
The main symptom of acute hemorrhoids is most often pain in the anus, caused by thrombosis of hemorrhoidal vessels. In the presence of pronounced edema and inflammatory infiltration of surrounding tissues, a false impression of strangulation of hemorrhoids may be created. Most often, thrombosis of hemorrhoids begins with the internal ones, and then moves to the external hemorrhoidal plexuses, thus causing combined hemorrhoids. With this type of development of acute hemorrhoids, the main symptom is severe pain in the anus. If isolated thrombosis of external hemorrhoids develops (which is quite rare), upon examination of the perianal area, dense round-shaped formations of a purplish-blue color can be detected, which can persist for 2-3 months.
Typical symptoms of chronic hemorrhoids are periodic bleeding (usually during bowel movements) and prolapse of hemorrhoids outside the anal canal. Possible, but optional, signs of chronic hemorrhoids are pain, discomfort in the anal canal, and itching of the perianal skin.
Bleeding of varying severity is observed in more than half of the patients, which emphasizes the dominant role of this symptom in the diagnosis of chronic hemorrhoids. Typically, patients note the release of scarlet blood without clots, which can either be released abundantly from the anus, splashing the walls of the toilet, or leave a trace only on toilet paper. Sometimes streaks of scarlet blood can be detected in the stool. Most often, anal bleeding is periodic, that is, observed during or immediately after defecation. Less commonly, there is constant bleeding from the anus. Regular bleeding can lead to a decrease in peripheral blood hemoglobin levels and the development of anemia.
Prolapse of hemorrhoids becomes a characteristic sign of the disease in the later stages of chronic hemorrhoids, when dystrophy and atrophy of the ligamentous-muscular apparatus holding the hemorrhoidal plexus occurs. In the initial stages of hemorrhoid development, this symptom is the leading one only in a small proportion of patients. Prolapsed hemorrhoids are defined as soft-elastic dark cherry-colored formations, covered with mucous membrane, protruding into the lumen of the anal canal.
Pain in the anus in patients with chronic hemorrhoids is not a pathognomonic sign, as it is observed in a number of other proctological diseases. Most often, the pain syndrome is caused by the development of complications of hemorrhoids - the formation of acute and chronic anal fissure. Discomfort and anal itching can join other symptoms of hemorrhoids in later stages of the disease, most often in patients with pronounced functional changes in the colon and obturator apparatus.
Hemorrhoids chronic
Home» Diseases» Chronic hemorrhoids
Make an appointment with a proctologist in St. Petersburg
How to prepare for a consultation with a proctologist
During my life, I have probably written articles, lectures, reports and presentations on hemorrhoids for patients and colleagues on “War and Peace” or the now popular “Shantaram” (I am not comparing talent, of course, only volume). At the same time, it was much more difficult for me than for Lev Nikolaevich and Gregory David, since war and peace, love and death are eternal and broad topics, and hemorrhoids are an equally eternal topic, but very narrow in every sense (one might also add a thankless , since in a decent society the statement that you are the author of “Shantaram” will cause “wow!”, and the fact that you wrote a book and a lot of articles about hemorrhoids will lead to nervous laughter, with quiet requests in your ear to leave a business card for “one friend”). Relatively recently, I published my last article for the MedTown.ru portal, in which, in general, I said everything I could and wanted on this issue. Competing with yourself is a very thankless task, but your own website, in the absence of editors, moderators, bosses and other bores and retrogrades that prevent us from living and creating, allows us to include more creativity (which is what it was created for), so I’ll try.
What are hemorrhoids, or a little anatomy
So, the first thing I would like to note is that although hemorrhoids and their treatment are associated exclusively with a proctologist, you need to understand that this is primarily a vascular disease that simply affects very specific vessels in a very specific and intimate area - the anus. It is difficult to write decently about an “indecent disease,” so to understand the anatomy and function of hemorrhoidal tissue, the best example is the clitoris and penis. Both the first and second organs, which allow us to somehow diversify the gray everyday life, consist of the so-called cavernous tissue - vascular barrels (cavities), with a powerful muscle layer, which, at the moment of the appearance of a worthy object of sexual desire, are filled with blood, increasing more or less significantly in size, depending on age, mood, degree of fatigue and, in extreme cases, the availability of Viagra and other masterpieces of the pharmaceutical industry. After the hormones have worked, the caverns contract, returning blood to other organs, in particular the brain, in which thoughts about a cigarette, tomorrow's meeting, or that there are many other ways to have a good time in the world begin to appear.
The substrate of hemorrhoids is the internal and external hemorrhoidal plexuses, also consisting of cavernous vascular tissue, but it works exactly the opposite: when we are busy with all other life processes, except for the final stage of digestion, the caverns are filled with blood, providing additional sealing of the anus. At the culmination of ridding the body of accumulated waste and toxins, the cavities shrink without interfering with the act of defecation.
Another important point is the environment in which these choroid plexuses are located. In everyday life, this zone is called the anus, and in medicine, in which since ancient times it has been customary to complicate everything and hide it behind clever words - the anal canal and the lower ampullary rectum or anorectal zone (you must agree, the phrase “I treat diseases of the anorectal zone” evokes much more respect than the phrase “I treat the anus,” so our ancestors from the medieval guilds, who introduced the fashion for complex terms with a lot of Latin, can be understood). The anal canal is a very small anatomical region that starts from the junction of the skin into the so-called anoderm (squamous epithelium that covers the inside of the anal canal) and ends at the junction of the anoderm into the columnar epithelium of the rectum. The total length of the anal canal is only 1.5-2.0 cm. Along its upper border there are glands covered with valves, secreting a secret that facilitates the act of defecation, which give it a very characteristic relief (see photo, 2 - jagged line), thanks to which this border is called the “jagged line” in medical literature. The latter plays a vital role in choosing a treatment method for hemorrhoids, so the most patient readers will learn a lot of new (definitely) and interesting things (I hope) about it in the corresponding section of the site. Above the anal canal begins the rectum, or rather its wide section, which is called the ampulla, necessary for the accumulation of intestinal contents. More detailed information about the anatomy and physiology of the anorectal zone can be found in the section of the site of the same name.
The internal hemorrhoidal plexus is very well expressed in all people and is located above the dentate line, i.e. from an anatomical point of view, not in the anal canal, but in the lower part of the rectal ampulla. The external hemorrhoidal plexus is much less pronounced and is located under the skin around the anus. In this case, the cavities are distributed unevenly in the anal canal, forming “hemorrhoidal pillows”, in most people located at 3-4, 7 and 11 o’clock on the conventional dial (what a conventional dial is, you can also read in the section on the anatomy of the rectum and anus) .
Thus, hemorrhoids are a disease that affects the external and internal hemorrhoidal venous plexuses, in which there is a pathological increase in vascular cavities with a gradual stretching of their ligamentous apparatus. And the hemorrhoidal node, accordingly, is a conglomerate of stretched and partially lost cavities, covered on the outside with the mucous membrane of the rectum, anoderm, or skin.
Why do hemorrhoids occur?
All mammals on our planet have hemorrhoidal plexuses, but hemorrhoids bother only great apes, and humans are several orders of magnitude more likely than our poor and wild relatives from the jungle. This fact, in my opinion, is quite enough to clearly say that the main cause of hemorrhoidal disease is our lifestyle, in particular upright walking. Of course, the question immediately arises as to why this system is implemented so ambiguously, because the Creator was aware that we would walk on two legs and invent more and more adventures with our heads and hands... In fact, even with a superficial acquaintance with anatomy and physiology of our species, a lot of such questions arise, for example, why such difficulties with procreation, would they lay eggs for themselves and continue to drink, walk and have fun in anticipation of the miracle of birth. And the teeth - why exactly? Since recently the feelings of believers in our country have become more and more unpredictable, and punishments for insulting them have become more and more severe, I will not go deeper into this topic. I only hope that when humanity itself creates the first intelligent biomechanical Creation, people will not forget to convene a medical consultation with a gynecologist, proctologist and dentist, who will try to protect engineers from rash decisions 
Patients at appointments often ask the question, “why did this misfortune happen to me?” The answer to this question logically follows from everything stated above - simply because we are people, and people of the 21st century, who actively use all the modern benefits of civilization. If proctologists had their own advertising slogan, it would sound like this: “You are Homo sapiens and you are over 40 - then we are coming to you!” My fairly long experience in conducting preventive examinations allows me to confidently say that by this age, hemorrhoidal “pillows” increase in everyone without exception. Another question is that some people are more lucky, and this does not cause active complaints for the time being; others are less lucky, and the full clinical picture of the disease appears earlier, sometimes much earlier than the specified age. So there is no need to stress too much about this. If you are tormented by the question of why you are already delving into the Internet in search of an answer to the question “how to live further”, and your peers at work seem to be clueless, think about which of them you plan to discuss your upcoming visit to see a proctologist - and you’ll understand everything.
There are a number of factors that significantly accelerate the development of hemorrhoidal disease, but according to the logic of the story, I have included them in a separate section “Prevention of hemorrhoids,” which I recommend that you read further.
What are hemorrhoids, or a few words about classification
The presence of internal and external hemorrhoidal plexuses determines the main variants of the chronic course of the disease: hemorrhoids can be internal, external and combined. From the definition it is clear that internal hemorrhoids are located inside and covered with mucous membrane, external ones are covered with skin and are clearly visible without the use of torture instruments from the proctologist’s arsenal; the diagnosis of combined hemorrhoids is made in the presence of both external and internal components.
The generally accepted option for staging hemorrhoidal disease is the Goligher JC classification, proposed in the 60s of the last century. It is based on the severity of symptoms of chronic hemorrhoids and involves 4 stages:
Stage 1 Bleeding without prolapse of nodes
Stage 2 Prolapse of hemorrhoids with spontaneous reduction into the anal canal ± bleeding
Stage 3 Prolapse of hemorrhoids with the need for their manual reduction into the anal canal ± bleeding
Stage 4: Constant prolapse of internal hemorrhoids and the impossibility of their reduction into the anal canal ± bleeding
Today, this classification is a little outdated, since with the advent of more and more new methods of treating hemorrhoids, it has ceased to fully meet its main task - to help in choosing treatment tactics. This issue is discussed in more detail when discussing methods of treating chronic hemorrhoids.
How hemorrhoids manifest or symptoms of the disease
Hemorrhoids in our everyday life have long become synonymous with problems. The phrase “we live in very hemorrhoidal times, in a hemorrhoidal country, and we are led by great experts in creating hemorrhoids for ourselves and those around us” is well understood by everyone without a translator. At the same time, by and large, we offend this disease completely unfairly, since it very rarely causes serious problems, i.e. There are a lot of diseases that are much more harmful to health.
Why did hemorrhoids take such a strong place in our vocabulary? This is due to exacerbations of the disease (or acute hemorrhoids) - a very painful condition when, as they say, you can’t sit down or stand up due to pain and discomfort in the anus. Both the symptoms and approaches to the treatment of acute hemorrhoids differ significantly from the chronic course of the disease, so I included a description of it in a separate article.
Chronic hemorrhoids are manifested by a quartet of main symptoms:
- bleeding
- prolapse of hemorrhoids during straining and physical activity
- the presence of external hemorrhoids and associated aesthetic and hygienic discomfort
- periodic exacerbations of the disease (thrombosis)
Other complaints, which include itching, burning and mucus discharge, can also be a consequence of chronic hemorrhoids, but they are much less common and are often symptoms of other proctological diseases, often quite serious (!). Separately, I would like to emphasize that pain is not typical for chronic hemorrhoids outside of exacerbations. If you have been bothered by intense pain for a long time, then this is definitely caused by other diseases, from a banal anal fissure to oncological pathology.
In the “Symptoms” section, complaints with which people turn to a proctologist and the possible causes of their occurrence are discussed in more detail.
Diagnosis and differential diagnosis of chronic hemorrhoids
The specialty “proctologist” (or more correctly “coloproctologist”) and specialized proctology clinics do not exist in all countries of the world. In many European countries, the treatment of hemorrhoids is carried out by general surgeons (until recently this was the case in our country), endoscopists and gastroenterologists. Even the St. Petersburg Center for Coloproctology at one time began with an ordinary general surgical department, and the proposal of our visionary leadership to specialize in the field of colorectal surgery initially caused a lot of fun and a minimum of understanding among the team. At present, especially with the gradual transition to laparoscopic surgical techniques, the need for institutions and specialists specializing in “major” surgery of the colon and rectum no longer raises questions for anyone. At the same time, all general surgeons traditionally continue to practice “minor” proctology.
I made this lyrical digression to the fact that the diagnosis and treatment of chronic hemorrhoids is considered a relatively simple task, which is why surgeons, gynecologists, urologists, and therapists deal with it. If we add to this list Malakhov and the campaign, experienced mothers, fathers, grandfathers, grandmothers and girlfriends from the maternity hospital, terabytes of flood from various forums, groups on social networks, “leftist” sites and advertising articles, etc., etc., then the proctologist is simply lost in this sea of knowledgeable people. And indeed, in most cases, a ward is not needed to diagnose “hemorrhoids” (may my colleagues forgive me): listen to complaints, look, at most, put on a glove and stick your finger into the profile hole - that’s all “science”. If we put aside shop and personal interests, then really, are proctologists really needed to treat such a simple and understandable disease as hemorrhoids?
For example, I have no doubt about the answer to this question: yes, they are needed. Any narrow specialization in any area of professional activity (not only medicine) can improve its results. With regard to hemorrhoids, a direct appeal to a proctologist, bypassing all of the above “experts,” can significantly save your time, nerves, money, and often simply save your life in the literal sense of the word. I will try to argue my opinion for skeptics and doubters.
First, regarding the slightly pretentious statement about saving lives. Something hurts, itches, starts to bleed, or starts to fall out of your anus - we will skip the first thoughts on this matter due to the high probability of using profanity, and the second thought, naturally, is “it’s hemorrhoids.” And this idea is fundamentally wrong, since there are a lot of diseases that manifest themselves in exactly the same way, but are much more serious. The list of the most dangerous ailments that require the earliest possible start of treatment is given below:
- rectal cancer
- colorectal cancer
- anal cancer (squamous cell carcinoma)
- familial polyposis
- villous tumors of the rectum
- Crohn's disease
- nonspecific ulcerative colitis
- polyps of the rectum and colon
Agree, the list is quite long. If you're thinking that you're too young to worry about such problems: this is partly true, since the peak incidence of intestinal cancer occurs at the age of 50-60, but only partly. The youngest patient I treated with a villous tumor was 19 years old. Before me, she had been examined several times and treated for “hemorrhoidal bleeding” for more than six months, although a banal digital examination by an experienced specialist would have been quite enough to make a diagnosis. Over the past year, three patients from 38 to 45 years old came to me, who were treated for about a year for perianal dermatitis, although a banal visual examination by a specialist would be enough to suspect squamous cell carcinoma and take a biopsy, etc. Crohn's disease, ulcerative colitis and polyposis are, in principle, diseases of young age, the incidence of which has been growing in both Europe and Russia over the past decades. If you comply with diagnostic standards - mandatory anoscopy and rectoscopy for patients of any age, mandatory appointment of fibrocolonoscopy after 50 years or according to indications, then the differential diagnosis of hemorrhoids does not pose any special problems (the only “but” is that it is better to undergo such diagnostics, of course, in specialized institutions, so no one has canceled the “human factor” and medical errors). But the initial appeal to the zombie box, the World Wide Web and experienced fellow citizens, unfortunately, completely eliminates this stage. Patients begin to blindly use advertised suppositories and ointments, most of which contain anti-inflammatory and analgesic substances, therefore relieving the symptoms of any of the mentioned diseases, which further strengthens the patient’s belief that it really is hemorrhoids (“suppositories are for hemorrhoids”). The result is lost time, during which modern medicine makes it possible to achieve recovery in most cases, using fairly humane methods. Turning to “familiar doctors” such as your gynecologist, your urologist, your local doctor, and even your surgeon (which is often unpleasantly surprising) is also a “double-edged sword.” Doctors, of course, are aware of diagnostic standards, but very often they skimp on them. The reasons are absolutely clear: gynecologists, urologists and therapists do not perform rectoscopy themselves, “why send a good person to other specialists, it’s clear that it’s hemorrhoids”, fibrocolonoscopy is a very unpleasant procedure, “why bother him/her, it’s too early for big problems” etc. An experienced proctologist, regularly seeing the results of such pseudo-humanism, eventually loses it completely. You can read more about early cancer diagnosis in the sections “prevention of colon cancer” and “prevention of anal cancer.”
Now about saving time, nerves and money. There are currently a lot of proposed methods for treating hemorrhoids: from drug therapy to minimally invasive manipulations and several surgical treatment options. And the doctor’s art is not just in making a diagnosis (this is really a small trick), but in competently selecting a treatment method depending on the individual topographical features of hemorrhoids, the severity of complaints, the psychological status of the patient, concomitant pathology and some other factors. It should be noted that this is a very difficult task. For its competent solution, in addition to sufficient experience, the method of examining the patient (on the back, on the side, in the knee-elbow position), the time of the examination since the last exacerbation or childbirth, the type of instrument (anosocope) that is used for diagnosis, and even the method of preparation for the examination. Proctologists discuss the “insidiousness” of hemorrhoids in terms of diagnosis very often on the sidelines. It is a well-known fact that hemorrhoids in the examination chair and the same hemorrhoids in the operating room are two completely different hemorrhoids, since when the patient relaxes under anesthesia, everything becomes an order of magnitude more neglected. Even doctors with sufficient experience make mistakes in choosing treatment tactics: you spend a long time doing ligations and sclerotherapy, after you understand with the patient that the attempt was unsuccessful, already in the operating room, looking at your handiwork after giving the patient anesthesia, you think “Oh my God, Am I really the ***** who offered the person non-surgical treatment? True, with experience such cases become much less frequent. It is worth adding to this that I know quite a lot of general surgeons who can operate on hemorrhoids at least as well as I can, but at the same time they are sure that only a well-sharpened scalpel can be better than a scalpel. When you tell them about the good results of minimally invasive treatment, they chuckle sarcastically, like “tell these tales to your patients.” When you have a consultation with such radicals, you may hear only two sentences: either “welcome to the operating room” or “it’s too early, come back in a year or two.” I also know many doctors who work in commercial clinics that do not have operating rooms, and have no less (most likely even more) experience in using ligation and sclerotherapy than I do. But they are characterized by distortions in the opposite direction: since for surgical treatment the patient needs to be “transferred” to another clinic, they will torture you with minimally invasive methods for a long time and persistently, and only when you begin to express slight bewilderment about the lack of expected results, will they say with a sad face that They did everything they could and will send you to the hospital (I think it’s clear that no one will return the time and money spent to you).
Summarizing this section, which unexpectedly for me turned out to be similar to a propaganda and educational lecture (I apologize for the verbosity), the main advice is that if the complaints listed above appear, be sure to go for a face-to-face consultation with a specialist, make sure that it is really hemorrhoids, and then with Decide with peace of mind who you trust more, Malakhovsky medicinal cucumber or traditional medicine. To diagnose chronic hemorrhoids, an examination by a specialist and anoscopy is sufficient; for the purpose of differential diagnosis, it is very advisable to undergo sigmoidoscopy. You also need to be prepared for the fact that the doctor may, based on indications or age, suggest that you undergo a fibrocolonoscopy, or at least an immunochemical test for occult blood. If the doctor has doubts about which treatment method to offer you, he may prescribe a short course of drug therapy and a follow-up visit at the end of treatment - this is “good manners” and is not done at all in order to “get” extra money from you. Selecting a treatment method for hemorrhoids is not as simple a task as it seems, so I advise you to choose a clinic that has both an inpatient and an outpatient office, and a doctor who deals with both surgical and minimally invasive treatment of hemorrhoids (in St. Petersburg, for example, there are at most several dozen such specialists) . You can read more about methods for diagnosing hemorrhoids in the corresponding section of the site.
Complications of chronic hemorrhoids or whether it is necessary to rush to treat it
Frightened patients who are too actively motivated to treat hemorrhoids by the sharks of the domestic medical business often turn to our Center for a “second opinion.” Since various horror stories are the most effective way of persuasion, this resource is actually used very often and without any twinge of conscience. According to corporate ethics, it is not customary to say anything bad about colleagues, so I will not list St. Petersburg clinics with a “tarnished” reputation in the professional environment, and you can understand people... When you are sitting in a well-known state Center, and you are not concerned about the question of where to find patients (more often you think about where to get two more hands and a time machine), as well as the cost of rent, advertising, consumables, etc., it’s very easy to puff out your cheeks in righteous anger. And when you live and work under the constant oppression of all of the above and much that is not mentioned, every patient who comes to you is literally “worth its weight in gold” and you really don’t want to let him go untreated for some ailment (including an absolutely mythical one). I recently opened my own doctor’s office, because in my own hospital it is becoming very crowded and difficult to provide consultations (often there is simply no time, and there is too much organizational chaos), so now I sympathize with the owners and employees of commercial clinics with knowledge and from the bottom of my heart. But in my opinion, the difficulties of running a medical business in our country are still absolutely no excuse for a predatory attitude towards people who turned to you for help, and a reasonable compromise between greed and conscience can always be found.
So, the most common motivators used to persuade people to urgently undergo treatment are given below:
- If you don't treat hemorrhoids now, there is a high risk of getting colorectal cancer
- If you don’t urgently get treatment right now using minimally invasive methods, then in the near future hemorrhoids will become “general’s”, and you will definitely fall into the clutches of sadistic surgeons
I think it’s already clear from the tone of the previous paragraph that all of this, to put it mildly, is untrue. Periodic inflammation of the rectal mucosa and its constant injuries due to prolapse of hemorrhoids, theoretically, of course, do not have the best effect on the oncological background, but there is no reliable data on the direct and significant connection of chronic hemorrhoids with the risk of developing rectal cancer in the medical literature. Therefore, in this regard, there is no rush to treat hemorrhoids and there cannot be, but with differential diagnosis, indeed, the issue is much more pressing, which has already been discussed earlier.
Regarding the thesis that it is urgent to catch and neutralize the disease before it reaches an advanced stage, this is also a very ambiguous question. Yes, it is clear that the early stages of the disease can be treated well with humane methods, while advanced stages can only be treated with surgical methods. But the transition from stage to stage takes not days or months, but years, even in the presence of additional unfavorable factors associated with lifestyle. Therefore, when, after the first exacerbation in your life, in the absence of regular complaints, they try to “grab you by the gills” and persuade you to urgent treatment, there is only one reason for this - to cheer up the doctor and investors of the clinic. There is always time to think or wait for a more financially and organizationally convenient period of your life to begin treatment for hemorrhoids, with very rare exceptions, which will be discussed below.
So, having dealt with non-existent problems, let’s move on to the real complications of chronic hemorrhoids. There are not many of them:
- regular bleeding leading to anemia
- exacerbation of hemorrhoids (or acute hemorrhoids)
- concomitant proctological diseases, for which the presence of chronic hemorrhoids is a good background and one of the main causes (rectal fistulas, anal fissures)
- purulent processes in the pararectal tissue (acute paraproctitis), the cause of which is also often acute and chronic hemorrhoids
Constant bleeding is the only serious reason for an insistent recommendation to start treatment without delaying it, and in the case of heavy ongoing bleeding, a reason for urgent surgical treatment (although this happens infrequently).
Acute hemorrhoids are a case when the patient does not need to be persuaded to undergo treatment; often it is even the other way around, you have to explain that surgical treatment in this case is not the best choice and you need to be patient a little and treat yourself with suppositories, ointments and tablets. You can read more about the tactics of treating exacerbations of hemorrhoids in a separate article on the site.
The presence of concomitant proctological diseases significantly influences the treatment tactics of hemorrhoids, in most cases being the reason for surgical treatment, and in the case of acute paraproctitis - for urgent surgery.
The article turned out to be too verbose (I wrote it on vacation with a lot of free time, which doesn’t happen often), but I hope that this is not empty verbiage, and patient readers learned a lot of new and useful things about the most common pathology with which they come to a proctologist. The site provides a lot of additional information about hemorrhoids, which can be found on other pages:
- Anatomy of the anal canal and rectum
- Acute hemorrhoids
- Treatment of hemorrhoids (this is a whole section with descriptions of all existing treatment methods)
- Prevention of hemorrhoids
There are also pages with a detailed description of the main diagnostic methods (consultation with a proctologist, anoscopy, rectoscopy, fibrocolonoscopy) and how much mental and physical torment you will experience if you decide to seek help from a specialist.
And finally, if I was convincing enough, I invite readers to take an autograph during a face-to-face meeting (coordinates and telephone numbers are in the “Contacts” section), or continue communication in absentia, for this there are the “Ask a Question” and “Reviews” sections.
Sincerely, Anatoly Ivanovich Nedozimovany, associate professor of the course of coloproctology at Pavlov State Medical University of St. Petersburg.
How to prevent hemorrhoids?
You can prevent the appearance of hemorrhoids if you adhere to the following rules:
- Food + water. To prevent hemorrhoids, try to eat more fresh vegetables, beans, and fruits. Less bread, red meat, cheese and dairy products. Avoid alcoholic drinks. It should be remembered that regular consumption of 8-10 glasses of clean water per day helps to loosen stools and prevent constipation.
- Stool thinners. For example, bran or plantain.
- Sport. Light physical activity and reducing the amount of time spent in sitting and standing positions reduces the risk of hemorrhoids. Another rule: do not lift things that are too heavy. This creates additional pressure on the anus and pelvis. If you do lift, try to do it while exhaling.
- Healthy bowel movements. What is this? First, don't spend too long on the toilet (many of us simply enjoy reading magazines in a "private place" and playing games on our smartphones). Secondly, do not overexert yourself during the bowel movement process.
Knowing about the symptoms of hemorrhoids, you can always prevent the development of the disease. And don’t forget to undergo medical examinations at the ACMD-MEDOX clinic!
Methods for treating hemorrhoids
If you consult a doctor in a timely manner, you can very quickly return to your previous life and forget about all your problems forever.
The easiest way to recover at an early stage is to take painkillers, anti-inflammatory drugs, and anti-blood clot medications specifically prescribed by the doctor to stop bleeding. Here it is important to take a certain dose at a specifically prescribed time. A specialist will tell you about this and how much the treatment costs. The disease can be cured by pathogenetic therapy, which normalizes digestion and eliminates constipation with the help of a special diet and enzyme preparations. In addition, you can try symptomatic therapy, which should improve venous tone.
Antithrombosis therapy is also actively used in many clinics. During treatment, doctors prescribe a special heparin ointment. If an acute disease is detected, doctors use combination therapy.
The most effective modern method of treating hemorrhoids is surgery, but it is used only in advanced forms of the last stages of the disease. If earlier this method was considered the main one in the treatment of hemorrhoids, now doctors are actively using the minimally invasive method and other modern, more patient-friendly options.
Features of internal hemorrhoids in women
Hemorrhoids can be called a “bisexual” disease, equally likely to affect both women and men. But the physiological characteristics of women can become a factor leading to hemorrhoids. This disease can manifest itself in the fairer sex for a number of reasons:
- Features of physiology. During menstruation, the vessels of the pelvic organs are filled with blood and this is an unfavorable moment for the appearance of hemorrhoids.
- Some gynecological diseases.
- Passion for diets. It's no secret that figure is very important for women. Throwing yourself into the loophole of certain dietary restrictions can lead to chronic constipation, which can negatively affect the condition of the rectum.
- Pregnancy. At this time, women’s motor activity decreases, the load on the entire body and on the vessels in the pelvic area also increases. Pregnant women often suffer from constipation. The enlarged uterus compresses the pelvic vessels.
- Childbirth. There is even a special term - postpartum hemorrhoids. During the birth of the baby, cracks may occur when pushing. Lumps in the anus and rectum.
Diagnosis of hemorrhoids
The patient's diagnostic examination plan should include:
- taking anamnesis;
- examination of the perianal area - you should pay attention to the condition of the skin, the presence of skin hyperemia, maceration, determine the degree of prolapse of hemorrhoids, the possibility of their self-reduction and the severity of bleeding;
- digital examination of the rectum - the presence of compacted hemorrhoids, polyps, anal papillae is determined, the functional state of the anal sphincter is assessed;
- clinical blood test - anemia and its severity are detected, as well as the manifestation of systemic inflammatory reactions;
- anoscopy - visually determines the condition of the internal hemorrhoids, the mucous membrane of the distal part of the rectum, the dentate line and the epithelium covering the anal canal;
- sigmoidoscopy - performed when colonoscopy is not possible and is intended to assess the condition of the mucous membrane of the rectum and distal part of the sigmoid colon;
- colonoscopy - performed to exclude other diseases of the colon that manifest similar symptoms.
Differential diagnosis
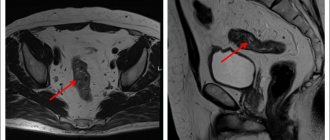
Polyps, villous tumors, cancer
Differential diagnosis should be made with sessile, non-moving broad-based polyps, polypoid formations (adenomas) and rectal cancer. Diagnosis of internal hemorrhoids not complicated by thrombosis, edema or prolapse is usually not difficult. Suspicion of rectal or anal cancer must be resolved through a mandatory biopsy and microscopic examination of the material obtained.
Hypertrophied anal papilla
If a dense formation is detected, the stem of which originates from the area of the dentate line, one should think about a hypertrophied anal papilla. An accurate diagnosis is made based on the results of anoscopy.
Rectal prolapse
Rectal prolapse can be partial (incomplete), affecting only the mucous layer of the intestinal wall, or complete, with prolapse of the entire thickness of the rectal wall. Incomplete prolapse may affect only part or the entire circumference of the rectum. Difficulties may arise in the differential diagnosis of prolapsed internal hemorrhoids and complete or incomplete rectal prolapse. It should be noted that internal hemorrhoids are formations that are not uniform in thickness and are separated by grooves, while with prolapse of the mucous membrane a cylindrical protrusion with clear boundaries is determined.