Causes of hemorrhoids during pregnancy
The development of hemorrhoids in expectant and young mothers is facilitated by many factors that are associated with physiological changes that occur in a woman’s body during pregnancy and after childbirth. These factors include:
- Changes in hormonal levels - increased levels of estrogen weaken the muscle tone of the vascular wall
- An increase in the size of the uterus leads to an increase in venous pressure
- Hereditary predisposition
- Age of the expectant mother - in pregnant women aged 20-30 years, hemorrhoids are detected in 20% of cases, after 30 years - in 50% of cases.
- Frequent constipation
- Decreased or lack of physical activity
- The birth process - during childbirth, compression of blood vessels in the pelvic area occurs, which can lead to prolapse or rupture of hemorrhoids.
What are the dangers of hemorrhoids in pregnant women?
If hemorrhoids in a pregnant woman are left to take their course, this can lead to serious consequences for the health of the fetus and the expectant mother. Therefore, it is necessary to treat hemorrhoids at all stages.
Prolapsed hemorrhoids can cause rupture of venous vessels, anemia and other complications that will affect the development of the fetus.
Constant constipation and straining due to hemorrhoids lead to chronic spasm of the anal sphincter muscles and contributes to the formation of anal fissures.
Against the background of impaired blood circulation, hemorrhoidal thrombosis occurs, which, if left untreated, can lead to necrosis of hemorrhoids.
Pregnant women need to be constantly monitored by a gynecologist and proctologist in order to identify signs of hemorrhoids in time and begin treatment in the early stages.
Diagnostics
If you notice any symptom of hemorrhoids, do not delay in visiting a coloproctologist. It is important to know that under the mask of hemorrhoids other, more serious diseases can be hidden. Early detection of hemorrhoids is the key to successful treatment.
The diagnosis is established by a doctor based on complaints, examination, digital examination, results of blood and urine tests, as well as instrumental diagnostic methods (sigmoidoscopy, anoscopy, irrigoscopy, colonoscopy).
If necessary, the doctor may recommend consultation with related specialists and additional examination.
Features of treatment of hemorrhoids in pregnant women
The treatment of hemorrhoids in pregnant women requires a special approach. During pregnancy, there are many contraindications for the use of many medications. Not all medications, suppositories and ointments that are usually used in the treatment of hemorrhoids are allowed for pregnant women. Standard methods of stopping bleeding and treating hemorrhoids, such as sclerotherapy and laser coagulation, are prohibited.
At a consultation with a proctologist, women carrying a child will be given individual treatment in accordance with the patient’s current condition and taking into account the entire clinical picture.
For mild forms of hemorrhoids, pregnant women are prescribed special suppositories and ointments approved for use during pregnancy. Also, to treat hemorrhoids in pregnant women, the doctor prescribes maintaining a special diet (consumption of foods with a high fiber content), increasing physical activity (swimming, walking), maintaining “wet” hygiene (using wet toilet paper and a hygienic shower).
Every woman carrying a child should remember the possible consequences of self-medication or lack of treatment for a particular problem. If any alarming symptoms occur, as well as as a preventative measure, you must make an appointment with a proctologist.
At the Naedine Clinic, you will be assisted by qualified gynecologists and proctologists who will conduct an accurate diagnosis and prescribe effective and safe treatment. Sign up for a consultation with a specialist by phone: (8332) 32-7777
Hemorrhoids - varicose veins in the anus, caused by hyperplasia of the cavernous bodies of the rectum, are the most common proctological disease. It is believed to affect more than 10% of the population aged 30 to 50 years. According to various authors [1, 2, 14], hemorrhoids occupy one of the first places in coloproctology, and its prevalence is high and amounts to 140-180 people per 1000 adults.
In women, hemorrhoids appear or worsen mainly during pregnancy and childbirth. According to statistics, hemorrhoids are 5 times less common in nulliparous women than in women who have given birth at least once. In this case, the age criterion also plays an important role: during pregnancy at 30 years of age, the disease occurs 3 times more often than during pregnancy at 20 years of age. According to N.V. Moon et al. [5], hemorrhoids occur in 7.7% of non-pregnant women, 25.7% of pregnant women and 49.8% of postpartum women. Pregnancy, although not the main pathogenetic factor of hemorrhoids, often reveals it and aggravates its clinical course. On the other hand, hemorrhoids in pregnant women often complicate the course of labor and the postpartum period [1, 10, 11].
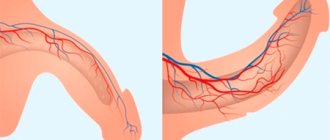
The views of researchers on the etiology of this disease are very contradictory. If Hippocrates attributed the cause of hemorrhoids to bile and mucus, then in subsequent centuries many different theories were put forward and disputed. Congenital insufficiency of the venous system, venous congestion, and disruption of the mechanism of the rectal sphincter were mentioned as the main pathogenetic factor. At the same time, none of the hypotheses based on the pathology of the venous system could explain the origin of the main symptom characteristic of hemorrhoids - the discharge of scarlet blood. The answer to this question was given relatively recently, in 1963, when cavernous vascular plexuses were discovered located in the submucosal layer of the caudal part of the rectum. Cavernous bodies are located in the area of the base of the anal columns diffusely or, more often, grouped mainly in three zones: on the left lateral, right anterolateral and right posterolateral walls of the anal canal. It is in these areas that hemorrhoids most often subsequently form. It has been proven that, in addition to veins and arteries, these vascular formations contain elastic connective tissue and smooth muscle cells. By regulating blood flow in the anal canal area, hemorrhoidal plexuses provide the basic functions of the rectum: retaining feces and defecation, providing an effective immune barrier between the internal environment of the body and the outside world. A hemorrhoid is a hyperplastic change in the cavernous tissue of the rectum, caused by an increased influx of arterial blood into the cavernous bodies through arteries with obstructed outflow through the efferent venules. The development of dystrophic processes in the anatomical structures that form the fibromuscular framework of internal hemorrhoids contributes to their gradual displacement in the distal direction [6, 19].
A major role in the development of hemorrhoids is played by impaired blood outflow through the venules from hyperplastic cavernous bodies of the distal rectum and anus. These cavernous bodies are present normally and are formed at the 3-8th week of embryonic development and are located in the area of the base of the Morganian columns. Cavernous bodies differ from ordinary veins of the submucosal layer of the rectum in the abundance of direct arteriovenous anastomoses. This is precisely the explanation for the fact that in hemorrhoids bleeding is arterial in nature. Hemorrhoids usually occur in individuals with pronounced groups of cavernous bodies. Other factors in the occurrence of hemorrhoids are congenital functional deficiency of connective tissue, impaired nervous regulation of the tone of the venous wall, increased venous pressure due to constipation, prolonged work in a standing or sitting position, heavy physical labor, and pregnancy.
The main pathogenetic factors in the development of venous pathology during pregnancy are:
- dishormonal changes;
— functional state of the vein walls;
- increase in circulating blood volume;
- changes in the blood coagulation and anticoagulation systems;
- increased intra-abdominal pressure.
A certain role in the occurrence of hemorrhoids is attributed to the abuse of alcohol and spicy foods, as a result of which the arterial flow to the cavernous bodies of the rectum increases. With prolonged exposure to unfavorable factors, along with predisposing factors, hyperplasia of the cavernous bodies occurs and the hemorrhoidal node itself is formed [4, 10, 12].
There are internal hemorrhoids, located above the pectineal line under the mucous membrane of the rectum, and external, located below the pectineal line under the skin. Approximately 40% of patients have a combination of external and internal hemorrhoids - mixed hemorrhoids. External hemorrhoids are observed infrequently - in less than 10% of patients [3, 7, 20].
With external hemorrhoids, the nodes are localized on the outside, and they should not be confused with prolapsed internal hemorrhoids. Most often, external nodes manifest as thrombosis. As a rule, bleeding from external nodes does not occur, since they are not injured during defecation. But constant stagnation of blood in them can lead to the formation of blood clots in them. Externally, the external hemorrhoidal node can be of different sizes, from 3 mm or more, which depends on its blood supply. An external hemorrhoid is usually covered by skin, while a prolapsed internal hemorrhoid is usually covered by the mucous membrane of the anal canal.
With internal hemorrhoids, there are varicose hemorrhoidal veins, which are located deep in the anal canal, so such hemorrhoids are not visible during a normal examination. In order to see them, you have to resort to special research methods: anoscopy, rectoscopy. Also, such nodes can be identified during digital rectal examination.
There are three degrees of internal hemorrhoids:
1st degree - hemorrhoidal veins are located in the anal canal, may not be palpable, cause subjective complaints by maintaining inflammation or causing bleeding.
2nd degree - nodes protrude from the anus when straining and disappear on their own.
The 3rd degree is characterized by prolapse of hemorrhoids that cannot be reduced on their own.
Hemorrhoids can occur acutely or chronically, but essentially these are phases of the same process. In acute hemorrhoids, inflammation occurs in the nodes, which, in addition to other symptoms, leads to severe pain in the anus. Spasm of the rectal sphincter increases swelling, leads to stagnation of blood in the lower rectal plexus and thrombosis of external hemorrhoids. In some cases, acute inflammation is accompanied by swelling of the perianal area and necrosis of the nodes. The often occurring tissue swelling and inflammatory infiltration create the impression of pinched hemorrhoids [2, 21].
The acute course of hemorrhoids is divided into three stages:
Stage I is characterized by thrombosis of hemorrhoids without inflammation.
Stage II is characterized by the addition of inflammation.
Stage III is characterized by widespread thrombosis of external and internal hemorrhoids with inflammation of the subcutaneous tissue, swelling of the skin of the perianal area, necrosis of the mucous membrane of the hemorrhoids.
During chronic hemorrhoids there are four stages:
In stage I, minor changes are noted in the ligamentous apparatus of the rectum, which is responsible for holding hemorrhoids in the anal canal, i.e. There was no prolapse of hemorrhoids.
In stage II, changes in the ligamentous apparatus of the rectum are expressed to such an extent that prolapse of hemorrhoids is noted during the act of defecation, but they themselves are reduced into the anal canal. In this case, bleeding may or may not be observed.
Stage III is characterized by such changes in the rectum that the prolapsed nodes no longer correct themselves, and the patient is forced to reset them himself after each act of defecation.
In stage IV, there is already a constant prolapse of hemorrhoids, and it is almost impossible to set them back. This is due to pronounced changes in the ligamentous apparatus of the rectum.
With chronic hemorrhoids, scarlet blood is released during bowel movements, prolapse of hemorrhoids, dull, incessant pain in the anus, and itching. A typical symptom complex of the chronic course of the disease consists of repeated bleeding, usually associated with defecation and prolapse of hemorrhoids from the anus. Bleeding as the leading symptom of hemorrhoids is observed in more than half of patients. Continuous bleeding from the anal canal is a complication of the disease. Prolonged bleeding from hemorrhoids leads to anemia. The second most common symptom characteristic of hemorrhoids is prolapse of hemorrhoids. There is a direct relationship between the increase in the duration of the disease, its stage and the frequency of prolapse of hemorrhoids. Anorectal bleeding, in addition to the main symptom of hemorrhoids, is a characteristic symptom of other diseases of the colon: malignant tumors, diverticulosis, nonspecific ulcerative and granulomatous colitis. Under the guise of hemorrhoids, especially when bleeding from the rectum, diseases such as polyps and colorectal cancer often occur. Therefore, for any manifestations of intestinal discomfort and, especially, when blood is released from the rectum, it is necessary to perform a digital examination, rectoscopy, colonoscopy or irrigoscopy. One rule must always be followed: at the slightest suspicion of a tumor, always take a biopsy and completely examine the colon [6, 9, 19, 21].
In modern conditions, the problem of hemorrhoids in pregnant and lactating women occupies a special place [1, 4, 13]. The clinical symptoms of hemorrhoids during pregnancy do not differ from those during the normal course of the disease. Most often these are pain in the anus, rectal bleeding and anal itching [5, 15, 22].
Often pregnant women are diagnosed with hemorrhoids in an asymptomatic stage. These women do not present complaints characteristic of hemorrhoids, but upon examination, hemorrhoidal nodes are found in typical places on the walls of the anal canal. Timely identification of pregnant women with clinically asymptomatic hemorrhoids and implementation of preventive measures in them makes it possible in many cases to prevent its development, which complicates the course of childbirth and the postpartum period [1, 13].
The clinical picture of hemorrhoids in pregnant women develops gradually. Initially, unpleasant sensations appear in the anus, especially after defecation. As the duration of pregnancy increases, more pronounced signs of hemorrhoids appear - pain, enlargement of hemorrhoids, bleeding, anal itching, tenesmus, etc. [1, 15, 22].
About half of women who have hemorrhoids during pregnancy experience an exacerbation of the disease after childbirth. As a rule, already with the onset of labor, pain in the anal area increases sharply. During the second stage of labor, when the fetal head passes the pelvic cavity, the vessels of this area, including the rectum, are sharply compressed. Venous outflow is disrupted, blood stagnation and tissue hypoxia increase. This creates additional conditions for the opening of arteriovenous anastomoses directly into the lumen of the cavernous cavities of the rectum. The longer the second stage of labor, the more pronounced these processes are. Hemorrhoids swell, increase sharply in size, and become tense. During pushing, the anal sphincter opens, the distal end of the rectum gapes, and both external and internal hemorrhoids are clearly visible. They enlarge before our eyes, become bluish and dense. After the end of the pushing, the internal nodes decrease somewhat, and with subsequent pushing, the picture repeats. When the fetal head erupts, internal hemorrhoids, if they are sufficiently pronounced, are squeezed out and sometimes their walls rupture. After childbirth, as the anal sphincter gradually contracts, the internal nodes become smaller and reduce on their own, but often, if the sphincter contraction occurs quickly, these nodes are pinched and acute hemorrhoids occur [1, 4, 13].
Conservative treatment, the main goal of which is to eliminate pain and inflammation and normalize blood circulation in the rectal area, is carried out for acute hemorrhoids and in the early stages of chronic hemorrhoids. Conservative drug treatment can be general - drugs that increase the tone of the veins, improve blood flow through small vessels and cavernous veins, and local - wound healing, analgesic and antipruritic ointments, suppositories, microenemas and baths [8, 16, 18].
Prevention of exacerbations is also of great importance, which includes:
- combating stool disorders (getting rid of constipation and improving bowel function without prolonged straining);
- proper nutrition (a diet rich in fruits and vegetables; a strict prohibition of any alcoholic beverages, salty, hot, spicy, pickled, peppered dishes, as these products increase blood flow to the veins of the pelvic floor and primarily the hemorrhoidal venous plexuses);
- proper hygiene after defecation;
- prevention of physical inactivity (physical therapy and hygienic gymnastics help improve the function of the large intestine, increase the tone of the muscles of the anal area and abdominal wall, and reduce congestion in the pelvic veins).
The development of hemorrhoids during pregnancy, as well as its complications, especially in the postpartum period, significantly affects not only the patient’s condition, but also her quality of life. When choosing a drug for treating a pregnant or lactating woman, one should take into account its safety both for the patient herself and for the fetus and newborn, which significantly limits the doctor’s choice [1, 10, 17].
For asymptomatic hemorrhoids, women are prescribed only preventive measures.
In stages I-II of the disease, treatment is carried out with suppositories and ointments, infusions of medicinal herbs, and the prescription of drugs taken orally. After defecation, it is possible to use rectal suppositories containing analgesic components. For spasm of the anal sphincter, it is possible to add suppositories with oil.
When hemorrhoids are combined with anal fissures, or acute hemorrhoids, conservative treatment is carried out in a hospital. It includes rest, diet, cleansing enemas, laxatives, novocaine blockades in the anus, local treatment with suppositories and ointments.
In case of prolapse of internal nodes, without symptoms of acute inflammation, they limit themselves to careful repositioning of the nodes after defecation (it is better to do this in a warm sitz bath). When there is a urge to defecate, small-volume cleansing enemas are recommended. Women are strictly prohibited from heavy physical labor and certain types of domestic work.
Pregnant women suffering from hemorrhoids with prolapse of internal nodes and frequent exacerbations of the disease are subject to hospitalization and surgical treatment. The timing of the operation is determined individually. Patients with such complications are treated with surgical (hemorrhoidectomy - excision of nodes) or minimally invasive treatment methods (minor or bloodless operations). These methods include sclerotherapy, ligation, infrared photocoagulation and laser coagulation. If the pregnant woman’s condition allows, all interventions are postponed to the postpartum period. Exacerbation of hemorrhoids, especially in combination with postpartum perineal trauma, is the most common disease that affects the quality of the postpartum period.
Currently, in obstetric practice for hemorrhoids, Procto-Glivenol is widely used, which is available in the form of rectal cream (1 g contains tribenozide 50 mg and lidocaine hydrochloride 20 mg) and rectal suppositories (1 suppository contains tribenozide 400 mg and lidocaine hydrochloride 40 mg).
The therapeutic effectiveness of Procto-Glivenol for hemorrhoids is due to the combination of two components: tribenoside and lidocaine. Tribenoside has a venotonic and anti-inflammatory effect. The venotonic effect is manifested by improving vascular tone, reducing venous stagnation, reducing the permeability of capillaries and venules and improving microcirculation. The anti-inflammatory effect is manifested by an inhibitory effect on some endogenous substances (bradykinin, serotonin, histamine), which act as mediators in the development of inflammation and pain. Lidocaine has a local anesthetic effect.
The above properties of Procto-Glivenol allowed it to take one of the leading places among antihemorrhoidal drugs, which is explained by the optimal composition, high efficiency and safety of use, especially during pregnancy (starting from the second trimester) and during breastfeeding, since it is during these periods that safety drugs is especially relevant.
Material and methods
We assessed the effectiveness and tolerability of Procto-Glivenol (cream and rectal suppositories) in the treatment of hemorrhoids in pregnant women. 85 pregnant women with clinical signs of hemorrhoids were examined.
All patients were divided into three groups depending on the stage of the disease. The 1st group consisted of pregnant women with asymptomatic hemorrhoids, who underwent preventive measures, including a diet with limited spicy foods and a sufficient amount of plant fiber, physical therapy, walks, and using the anal toilet after defecation. Group 2 consisted of patients with complaints of bleeding, anal itching, and pain during defecation. These women, in addition to the above measures, were treated with suppositories and cream with procto-glivenol from the second trimester of gestation. Group 3 (4 pregnant women) included patients suffering from hemorrhoids subject to surgical treatment. These were women with prolapse of internal nodes and with a history of frequent exacerbations, with heavy hemorrhoidal bleeding, as well as with acute hemorrhoids in the stage of necrosis of the prolapsed strangulated nodes. Pregnant women of group 3 were consulted by a proctologist, together with whom general tactics for further management were developed. These patients were also prescribed Procto-Glivenol according to individual regimens for preoperative preparation.
Procto-Glivenol cream was used for external hemorrhoids, applied to the affected areas in a thin layer 2-4 times a day, and after the pain disappeared - once for 7 days. Procto-Glivenol suppositories were used for internal hemorrhoids 2 times a day for 5-7 days, after the disappearance of painful sensations, once a day for another 7 days.
Results and discussion
It has been established that identifying pregnant women with clinically asymptomatic hemorrhoids and carrying out the special preventive measures described above make it possible to prevent the development of the disease, which complicates the course of childbirth and the postpartum period.
Clinically, the symptoms of hemorrhoids during pregnancy were almost no different from those among other categories of patients with this diagnosis. Of 85 pregnant women with clinical signs of hemorrhoids, pain in the anus was observed in 40 (47.1%), bleeding of nodes - in 28 (32.9%), anal itching - in 26 (30.6%). 55 (64.7%) of the observed women had external hemorrhoids, which was characterized by the appearance of hemorrhoids in the form of warty formations or folds, dense to the touch and not decreasing in volume upon palpation. In internal hemorrhoids (30-35.3%), the nodes were located between the folds of the mucous membrane, could be either single or multiple, collapsed when pressed and filled when coughing. In addition, in 13 (15.2%) pregnant women, hemorrhoids were combined with an anal fissure. It should be noted that if in pregnant women aged 20 to 30 years, hemorrhoids are detected in approximately every fifth, then after 30 years - in every second.
When assessing the results of therapy, the severity of remaining clinical symptoms was assessed by patients as average by the 7th day of treatment and as weak by the 15th day. At the same time, such a clinical symptom as pain during defecation was observed in 9 (10.5%) patients by the 7th day of treatment, and was not observed in any pregnant woman by the 15th day, bleeding - in 5 (5.9%) and 2 (2.4%), anal itching - in 6 (7.1%) and 2 (2.4%) women on the 7th and 15th days of treatment, respectively.
Clinical tolerability was assessed by patients and doctors on a scale: excellent, good, average, poor. Tolerability of treatment with Procto-Glivenol was excellent and good in 96% of cases.
conclusions
1. Procto-Glyvenol is the drug of choice for the conservative treatment of hemorrhoids and the prevention of its complications during pregnancy. The use of Procto-Glivenol, both in the form of cream and rectal suppositories, is an effective way to treat pregnant women with hemorrhoids.
2. The speed of action and good tolerability make it possible to recommend Procto-Glivenol for widespread use in obstetric practice.